
Probiotics are often marketed as the ultimate solution for gut health. From supplement bottles to yogurt ads, we're constantly told that these “good bacteria” can transform digestion, boost immunity, and even improve mood. But what if probiotics don’t make you feel better? What if they make you feel worse?
You're not alone if you’ve ever experienced bloating, brain fog, fatigue, or digestive discomfort after taking probiotics. This article’ll explore why probiotics can sometimes backfire, including their connection to histamine, FODMAP intolerance, and underlying gut conditions.
Long before modern probiotic supplements, our ancestors consumed probiotics naturally through fermented foods. Sauerkraut, kimchi, yogurt, kefir, and pickled vegetables were dietary staples, supporting gut health without the need for capsules or powders.
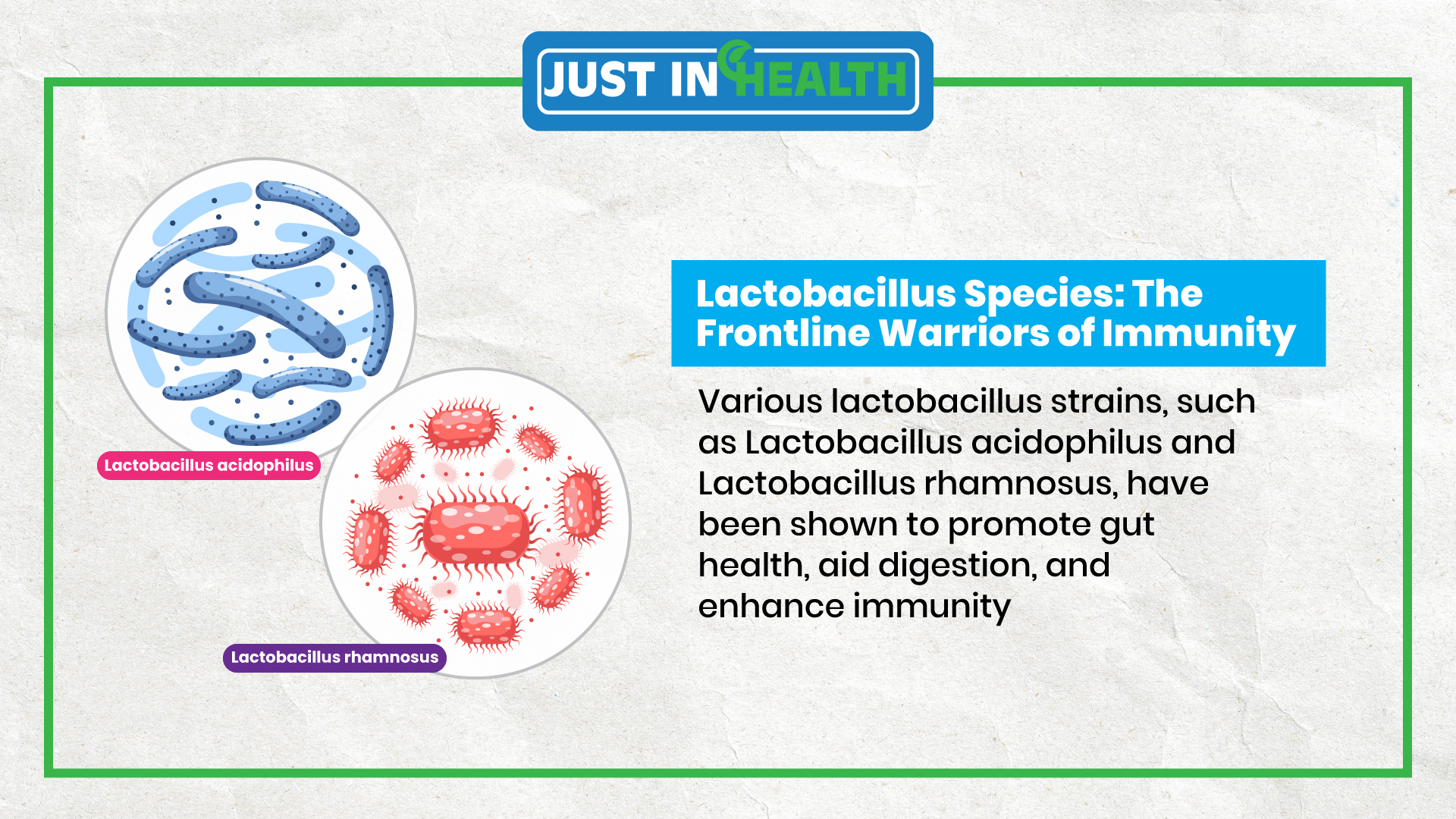
The Lactobacillus genus is one of the most well-known probiotics, often found in fermented foods. These bacteria help balance gut flora, improve digestion, and support immune function.
However, not all strains are beneficial for everyone. Some Lactobacillus species can increase histamine production, leading to unexpected side effects for those with histamine sensitivity.
Histamine is a naturally occurring compound involved in immune responses, digestion, and brain function. However, when histamine levels become too high, it can lead to symptoms such as:
Certain probiotic strains produce histamine as part of their metabolic processes. Consuming high-histamine probiotics can trigger uncomfortable reactions if your body struggles to break down histamine due to a deficiency in diamine oxidase (DAO).
Histamine-producing probiotic strains:
Histamine-friendly probiotic strains:
If you suspect histamine intolerance, switching to low-histamine probiotics or increasing DAO enzyme support may help reduce symptoms.
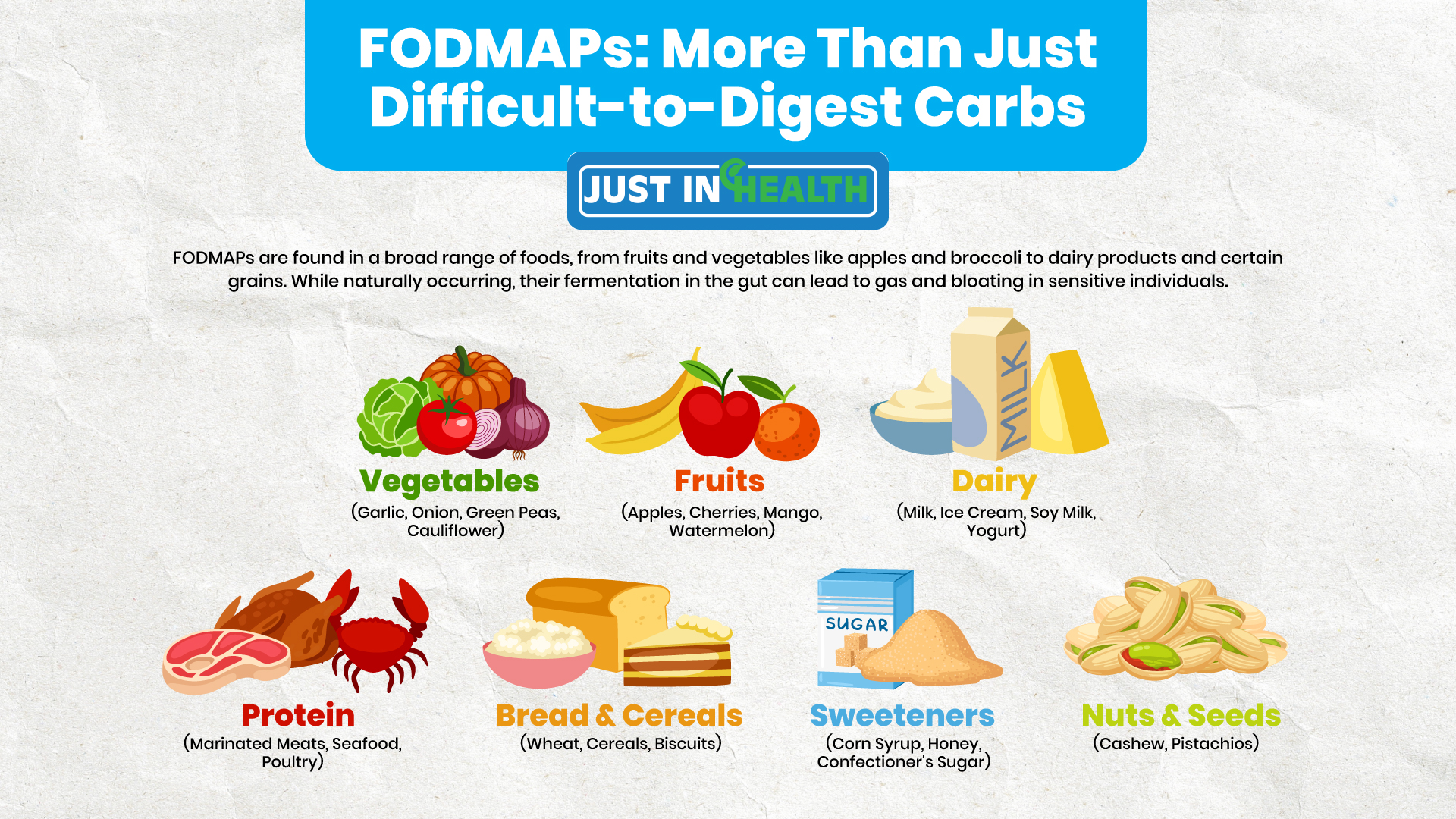
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that are difficult to digest. Foods high in FODMAPs can cause bloating, gas, and stomach pain, particularly in people with irritable bowel syndrome (IBS).
Some probiotic strains, particularly those that ferment carbohydrates, can increase gas production and worsen FODMAP intolerance symptoms. If you experience bloating or discomfort after taking probiotics, FODMAP sensitivity could be the cause.
Tips for minimizing probiotic-related bloating:
Sometimes, probiotics can worsen gut health instead of improving it. Here are some underlying conditions that may make probiotics problematic:
SIBO occurs when bacteria overgrow in the small intestine, leading to bloating, gas, and diarrhea. Probiotics can fuel the fire by increasing bacterial fermentation in the wrong part of the gut.
Symptoms of SIBO:
If you have SIBO, consult a doctor before taking probiotics.
H. pylori is a bacteria that can cause stomach ulcers and chronic gastritis. Probiotics can sometimes aggravate symptoms if they disrupt the delicate balance in the gut.
Signs of H. pylori infection:
Testing for H. pylori can help determine whether probiotics are right for you.
Parasites like Giardia can cause digestive issues, and introducing probiotics may trigger a stronger immune response, leading to temporary discomfort.
If symptoms persist, stool testing can identify hidden infections.
Not all probiotics are the same. Some support digestion, while others boost immunity or regulate mood. Identify your needs before choosing a probiotic.
Spore-based probiotics like Bacillus subtilis are more resilient and can survive stomach acid better than traditional probiotics. These may be a better option for those with sensitive digestion.
If you’re new to probiotics, start with a low dose and increase gradually. Keep track of symptoms and adjust as needed.
Probiotics can be a game-changer for gut health, but they’re not always the right fit for everyone. If you experience bloating, headaches, or digestive discomfort, you may need to reconsider the type and strain of probiotics you’re using.
Listening to your body and consulting a healthcare professional can help you find the right balance. When it comes to gut health, one size does not fit all.
Yes, especially if you have SIBO or are sensitive to FODMAPs. Some probiotic strains ferment carbohydrates, producing excess gas.
For most people, mild side effects subside within a few days to a week as the gut adjusts. If symptoms persist, consider switching to a different strain.
Yes, Bifidobacterium infantis and Lactobacillus gasseri are low-histamine options better suited for those with histamine intolerance.
If probiotics consistently cause discomfort, it may be best to stop and reassess. Consult a doctor to determine whether another approach to gut health is needed.
Absolutely! Fermented foods like yogurt, sauerkraut, and kefir provide natural probiotics. However, if you're histamine-sensitive, opt for fresh, non-aged ferments.
Recommended Products:
References:
“The Historical Use of Fermented Foods” by Dr. Linda A. Lee ↩
“Gut Health and Immunity: Unpacking the Connection” by Prof. Maria Collins ↩
“Histamine Intolerance and Probiotics: What's the Connection?” by Dr. John D. Reeves ↩
“Tailoring Probiotic Supplements: A Guide” by Dr. Sandra Clark ↩
“The Wonders of Saccharomyces in Gut Health” by Prof. Elena L. Martinez ↩
“FODMAPs Explained: Digestion and Sensitivities” by Dr. Hannah Brown ↩
“Unpacking Gut Issues: Beyond Probiotics” by Dr. Sam G. Peterson ↩