
Dr. Justin Marchegiani and Evan Brand go in depth about H. pylori infections and the conventional medical treatment using antibiotics versus the natural solutions. Learn what it is all about and how it can be treated when you listen to this podcast.
 They talk about the different studies made and publications that will help us understand what H. pylori is all about and how to effectively get rid of it. Find out what the testing methods are to check if you have certain infections. Also discover the mechanisms of how H. pylori can be spread so you can avoid getting infected.
They talk about the different studies made and publications that will help us understand what H. pylori is all about and how to effectively get rid of it. Find out what the testing methods are to check if you have certain infections. Also discover the mechanisms of how H. pylori can be spread so you can avoid getting infected.
In this episode, topics include:
00:52 About H. pylori
06:48 Mainstream care/conventional treatment
07:40 Conventional medical treatment vs natural treatment
14:45 Gut killing protocol and supporting affected body systems
19:30 Testing methods
Dr. Justin Marchegiani: Evan, it’s Dr. J. What’s going on? It’s Monday.
Evan Brand: Yes, sir! Back in the trenches, looking at some more lab results, and we got an email that requested this topic that we were probably gonna get to anyway which is on H. pylori, something that is honestly, once again, I feel like I say it—sounding like a broken record—but honestly more common that I though, so Mil, she sent in an email saying that she loved the podcast and she loves to actually hear our case studies and that she’s working with clients, too, and she’s seeing a lot of infections and she wanted to hear a podcast on H. pylori. So here we are. Thanks Mil from Melbourne, Australia.
Dr. Justin Marchegiani: Love it. Well, what do you think about H. pylori? I mean, that’s quite an—it’s an infection that I see probably over a dozen times a week in my clinic. I’d say at least 50 times a month, no problem. That’s pretty easy. It’s pretty common. What’s your take off the bat? Before I go on my little rant.
Evan Brand: Well, it’s something that you have to rule in or rule out because what I was talking with you about off air is a guy that I was working with, for some reason we haven’t run a stool test right out of the gate, so we just started with adrenal treatment and we sort of hit a wall. Some of the anxiety was reduced. Some of the depressive symptoms were reduced. The energy was increased. But we were still hitting this wall with some of the GI symptoms, some of the tinnitus, etc. and so I figured, okay, well, it’s time we need to circle back and run the stool test and that’s when we found Klebsiella and H. pylori. So for me, it’s something that you really have to rule in or rule out, and if you’re just hitting a wall or you’re not getting results with your program, this could be an underlying factor that—that many people don’t even have on their radar.
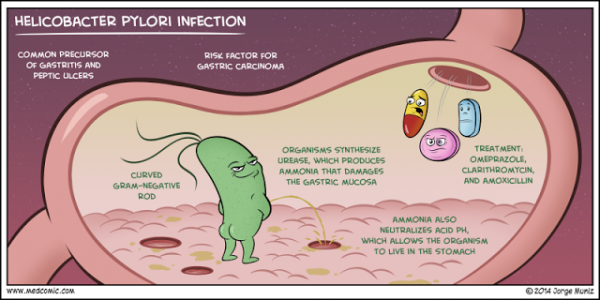
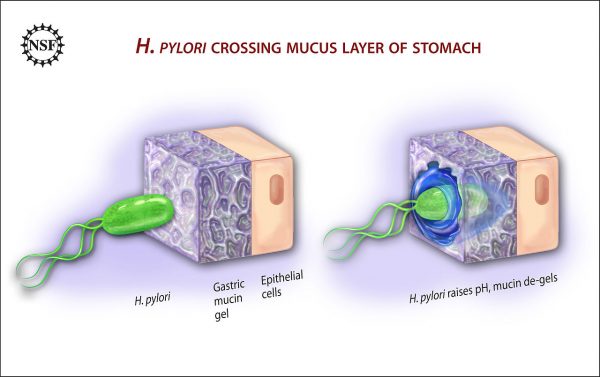
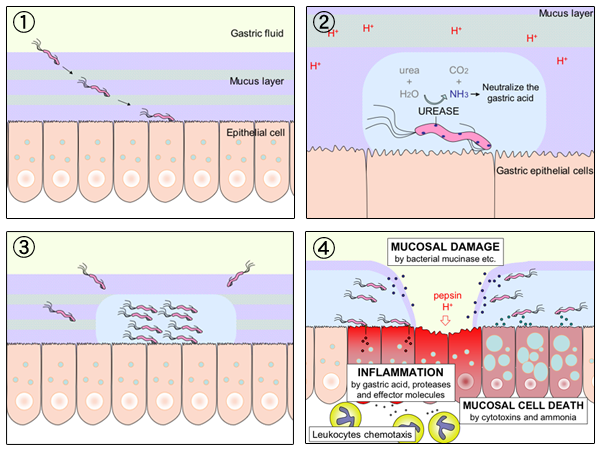
Dr. Justin Marchegiani: Yeah, I totally agree. I find H. pylori, it’s an opportunistic bug meaning if you’re under stress especially if you’re eating gluten and grains. If you have other type of toxic stress going in by eating, say pro-inflammatory foods, any type of body system stress is going to decrease your body’s ability to secrete hydrochloric acid because you’re lowering your parasympathetic nervous system which is like that vagus nerve that really helps you rest and digest, and that kinda opens us up. It lowers that force field to bugs that we may get in contact with like H. pylori and one of the mechanisms that H. pylori has is we have kinda like the gastric fluid in our tummy and then we have this mucous layer. And this mucous layer that kind of like provides this buffer protection against our epithelial cells. These are the cells that line—that really make up our stomach lining and the H. pylori comes in there, does a couple of things. It takes urea and it converts it to CO2 and ammonia via the enzyme urease. So H. pylori secretes this enzyme called urease that then takes increased ammonia and increased CO2 from the urea. Urea is a byproduct of protein metabolism. So we know how important the stomach is for breaking down protein. So imagine we have this set of dominos. I give this analogy to my patients all the time because it just—it’s what clicks with me the best. The first domino that has to knock over for healthy digestion is in the stomach and that’s gonna be low stomach acid. Low stomach acid activates an enzyme called pepsin. It turn pepsinogen into pepsin which helps break down protein. And again, stomach acid, the HCl is pH driven. So HCl, hydrochloric acid, drives pH down but when we eat protein, we have this urea that spits off it and if we have H. pylori in there, that’s gonna take that urea, turn it into—I’m sorry, take the urea via urease and turn it into ammonia and CO2. Ammonia’s got a pH of 11 that raises the pH, that low pH that—I’m sorry—that—that pH now that’s now raised up, it’s more alkaline, that’s gonna affect us from activating our digestive enzymes and the inflammation by the H. pylori starts to wear away that mucous layer and—and we have all the cytotoxins and the ammonia that’s now there, starts to damage those mucosal cells.
Evan Brand: Yeah, so I wanna go through some of the symptoms here that people notice. Basically long story short, what you’re saying here, we’re gonna have a severe compromise of the whole digestive process in general. So when I asked this male client, take a look at your fingernails, so he had the vertical ridging, which is something I also had, too. But we knew that there was some sort of protein malabsorption going on. So that’s one of the symptoms right there, is that some of these people they may even—I’m sure you’ve seen in some of the vegetarian and—and vegan clients as well. They may have just an intolerance for meat. But it’s an H. pylori infection. It’s not that they need to be a vet—a—a vegan or they’re built for a vegetarianism, they may—may have this infection that’s causing them to not do well with protein in general. So some of the symptoms here, you know we have the weakness, the tiredness, lightheadedness, irregular heartbeat, cold hands, cold feet, depression, easily bruising, stomach upset, weight loss, diarrhea or constipation and on and on. So a lot of the nutrients that you’re not gonna be absorbing from your food, that’s gonna show up when your fatigued. So that’s why if you go think about all these people out in society, going on acid blockers and energy drinks for their symptoms, they need to just look and see that there may be an H. pylori infection.
Dr. Justin Marchegiani: I 100% agree and H. pylori on one extreme it can cause deeper issues, right? We know like the mainstream type of issues it can cause is like increases in gastric cancer, gastric lymphoma and also ulcerations—that’s like one extreme. The problem is a lot of people that have H. pylori may not be at that level of extreme. They may have brain fog. They may have fatigue. They may have joint pain. They have migraine headaches. They may just be moody because remember when you affect digestion of proteins and, the ionizations of minerals, that means being able to take minerals into your bloodstream, lots of other symptoms can happen not just at the pathological extreme. So conventional medicine looks at things from the extremes. Functional medicine looks at things basically everything in between. And we know that if we have digestive issue, that’s gonna affect absorption. We know if we have gut inflammation, that’s gonna affect leaky gut and create bottlenecks for us getting us these important nutrients to have healthy metabolism and mood and performance from getting into our system.
Evan Brand: Yeah, so the problem is once again with the mainstream care here, is that you’re going to come across antibiotics and antibiotics are not going to be best option because some of the time you can have a rebound effect, right? So someone may go on an antibiotic, think that they’re better and then they’re actually not gonna get rid of the infection. So a lot of times you got for the conventional treatment here, you may get antibiotics and acid blockers at the same time, instead we like to look at the botanical alternatives, that honestly are just as effective if not more without not even 1% of the amount of side-effects that you’re gonna have with this conventional medical treatment. Do you wanna elaborate on that?
Dr. Justin Marchegiani: Right. So you’re talking about the conventional medical treatment versus kind of the—the natural and some of the side-effects with them all? Is that kind of–
Evan Brand: Right.
Dr. Justin Marchegiani: What the angle? So the conventional medical treatment is something known as the Prevpac or triple therapy. It typically is a combination of clarithromycin, amoxicillin, some type of proton pump inhibitor like omeprazole or Prevacid and sometimes they—they’ll sub in like bismuth instead of the proton pump inhibitors. So those are like the triple therapies. Now we run some genetic stool test that will actually see a lot of patients have resistance to clarithromycin, which is interesting that mean—that’s like kind of the big killer in this triple therapy for 2 weeks. They’ll give these three combination drugs together and I see a lot of patients that have these types of issues where they’re resistant to the antibiotic. Now that’s a problem because is the therapy gonna work? Probably not. And then also are we addressing the underlying issues that cause the compromised immunity to fall prey to the H. pylori to begin with? No. Are we fixing the collateral inflammation to the mucosal cells that were damaged? No. Are we fixing the underlying digestive issues from the low stomach acid and the low enzymes? No. Are we looking at the other co-infections that may be involved like Giardia or maybe a small intestinal bacterial overgrowth or yeast overgrowth or maybe a deeper parasite infection? No. So you can see all these other issues, it may just not be that simple of looking at one infection. And some people do get better on the triple therapy, but I’d say the majority of patients that I see have already been treated for H. pylori that have it, and they did not get resolution and a lot of times the antibiotics made them worse because they probably have this detoxification issue that was backed up because remember, detoxification pathways primarily run from B vitamins and sulfur amino acids and if our digestion’s impaired, well, there goes the protein, right? To—to run our phase 2 pathways. And if we have issues with gut bacteria being out of balance, well, the gut bacteria helps produce B vitamins, so you can see all these mechanisms kind of get knocked down and—and just treating the H. pylori with an antibiotic may not be the underlying—may not be the best way to go about it. It may cause more symptoms than—than actually fixing the issue in a functional medicine way that’s more linear like we talked about in our last podcast about our—the right path to healing.
Evan Brand: Right. So another piece, too, that I wanna mention is if you are going this conventional route, you’re never gonna get told to change your diet. You’re never even gonna get told that what you eat has a relationship to how you’re feeling with this H. pylori. So if you’re just doing supplements, even if you are going the natural route, but you haven’t adjusted the diet, your results are gonna be limited there.
Dr. Justin Marchegiani: Absolutely and let’s not forget, right? The same cells that make stomach acid, the parietal cells in the stomach, they’re also the same cells that produce intrinsic factor. Intrinsic factor is this binding protein that binds to B12 in the food, in the stomach, and then our tummy then—or I should say our intestinal tract reabsorbs it at the end of our small intestine in the area called the ileum. So we bind it up to this stuff, we basically tag it with this intrinsic factor in the stomach and then we re-absorb it at the end of our small intestine in an area called the ileum. Now this is interesting because we need stomach acid to liberate B12 from our food, and this is actually coming from Harvard School of Public Health’s website and they actually talk about the fact that it’s estimated that 10-30% of adults over the age of 50 are low in stomach acid.
Evan Brand: I’d say it’s like 90%. What do you think?
Dr. Justin Marchegiani: Yeah, I was just about to—to go into that. So like the big thing is, right? They’re looking at everything from like a pathological extreme.
Evan Brand: Right.
Dr. Justin Marchegiani: So, you mean just because you’re at pathological cut-off, what if you’re knocking up against it, you know? How many years do you have to knock up against it before they consider you, you know, very, very low in stomach acid? So I would say it’s much higher than that. I would—I’m 100% on your—on your level here. But the thing is, a talk about how stomach acid is require to liberate B12 from the food. Now why is B12 so important? We need B12 for healthy nervous system. If we don’t have enough B12, we’ll get something called subacute combined system disease or posterolateral scleros—sclerosis where the myelin sheath in the nerves will actually get worn away from lack of B vitamins, B12 in particular and we also need B12 to mature our red blood cells. Immature big goofy red blood cells have a hard time carrying oxygen and nutrition. So low B12 equals bigger red blood cells that aren’t mature, right? Red blood cells actually get smaller as they get more mature. As they are immature, they are bigger. It’s kinda like the opposite. Imagine like babies being born like 10-foot adults and they get more mature as they get older, it—it’s—that’s kinda how it is with the blood cells. So we see these big goofy cells that can’t do their job and that means lack of nutrition, lack of oxygen and basically overall lack of neurological health and methylation which is so important, too.
Evan Brand: That’s scary. So it really is—this is one of the biggest pillars that could collapse someone’s health journey if they go undiagnosed and untreated with this issue.
Dr. Justin Marchegiani: Absolutely and then H. pylori, like if you look at H. pylori, it’s got wo little walls. It’s a gram-negative bacteria, so how I kinda draw the analogy because I—I use analogies a lot because you don’t ever have to remember a story. People can hear stories and they—and they get it, right? People could think of maybe a story that their grandfather or grandmother told them when they were younger, and they heard it once and they still got it. So if we kinda teach in stories, we just say it once and they got it. But imagine H. pylori, it’s got like two cell walls, that’s a gram-negative bacteria. So imagine like anyone that watches Game of Thrones, right? We’ll use the castle analogy here. So imagine you got this like moat around the castle, that’s like the first wall of defense that H. pylori has. And then we have like the actual castle wall as like the second wall of defense. So we have two walls, right? We have the moat and then we have the castle wall. So it’s harder to kill these bacteria that have two walls obviously because it’s harder to get across the moat and then have the energy to climb up the wall. So imagine that’s kinda like H. pylori. Now in the outside before you get into the moat, imagine all of these traps, all these land mines, right? That’s what’s called LPS. They’re these little things that sit on the outer second wall that are basically toxic. LPS stands for lipopolysaccharide. It also stands for endotoxins. So it literally is a toxin. So imagine with H. pylori, we got the—we got the moat. We also have the big castle wall. That’s layer one and two. And then outside of the moat we have all these land mines. And that’s why H. pylori is so hard because the land mines are essentially a toxic stress on our body because as we kill the H. pylori, it can create more symptoms because our liver and our detox pathways have to process those land mines or those LPS/endotoxins.
Evan Brand: So what you’re saying here, it’s not gonna be just a gut-killing protocol when we come into treatment. It’s gonna have to be a multi-pronged approach here where we’re supporting the actual body systems that are getting affected by this dump essentially, which is the same thing that can happen with like parasitic infections, too, right?
Dr. Justin Marchegiani: Yeah, so we may use things like ginger because ginger is a biofilm type of buster. So biofilms are like imagine the—you know, on those outer two walls, we have these protective agents that make it harder for you to disable those land mines or harder for you to—to scale the moat or scale the wall. So the biofilm agents allow us to kind of attack those two walls easier so we can use things like ginger, as a really simple or easy one. A lot of the herbs we’ll use, we’ll have biofilm busters already in it. We may give extra enzymes to provide biofilm busters. We may give things like diatomaceous earth to help break down biofilms as well. And then we may—may even give extra binders like citrus pectin of various vegetable fiber pectins to basically put straightjackets around these crazy endotoxins. So imagine someone’s in a bar, they’re getting all rowdy, right? The bouncer comes in and puts their arm around their back and escorts them out. That’s what some of the fibers do. That’s what the charcoal also does as well. Diatomaceous earth can also help with that. So we have a lot of our different binding agents that we use in conjunction with some of the herbs. And again, you really wanna do this in—in sequence, so we always wanna work on body system one before body system two. Body system one being the hormones, two being the gut and infections, and three being detox. And then even before that, that sets the foundation is always the diet and lifestyle stuff. So you always wanna make sure if you have an infection, you’re better off working with a functional medicine doctor or practitioner because I’ve seen patients get far worse and far sicker doing these protocols on their own because what happens is you start feeling like crap and then you don’t know what to do. Because you only have one data point and because you’re getting sick and this is the first time you—you’ve felt it then you kind of go into freak out mode. So it’s always good to have someone that’s done it, in my case, a couple thousand times and—and I know you—you’re right up there, too, with your experience. So you want that experience because it gives you the confidence that you know you’re on the right track. Like if I’m going to Mt. Everest next summer to hike, you know, Everest, right? I want to go with one of those trail guys that have been all the way to the top. I don’t want to go on that journey alone because, man, it’d be pretty scary when it starts getting windy and stuff, and you don’t know what to do.
Evan Brand: Yeah. So something that’s cool that you just said, I’m glad you brought up the adrenals, you know, body system one here. I’m looking at a study, it was from 2012, and it was titled Effects of Alpha Tocopherol and Ascorbic Acid on H. pylori. Long story short, the H. pylori intensity was decreased by increasing the ascorbic acid concentration in the body. So a lot of times, you and I are using vitamin C anyway with adrenal support, hormone programs, and so that’s something that I usually keep in place is the vitamin C supplementation during H. pylori because we’re gonna be able to up the speed or up the—what they call here—eradication rate. It says by impairing the microenvironment created by the bacteria and facilitating the diffusion of antibiotics, which may be that’s herbal antibiotics and in our case, into gastric mucosa. So that’s a pretty cool finding there that we can actually see vitamins that we’re using for other protocols for this protocol, too.
Dr. Justin Marchegiani: Yeah, and also there’s a study here from the Journal of Psychosomatic Medicine, they talk about mucosal wound healing being impaired via stress. So they–
Evan Brand: I believe it.
Dr. Justin Marchegiani: They talk about that the data suggest here that something, you know, transient predictable, even relati—relatively benign can significantly affect the consequence of wound healing. Now it talks about mucosal wound healing. So now if we extract—extrapolate that to our gastrointestinal mucosa, we could see how supporting someone’s adrenals would then help balance and modulate cortisol levels, and if we know cortisol is important for that musical healing, you can see how us addressing body system one before we go into body system two being incredibly instrumental at setting the table for that nice immune mucosal wound healing environment.
Evan Brand: Definitely. Stress is a killer. I mean, it comes up in every conversation we have, I think.
Dr. Justin Marchegiani: I 100% agree. And so we know like the conventional H. pylori symptoms, a lot of people don’t have those, right? So then you gotta know well, just because you go to your primary care doctor and they say that you don’t have it, or maybe they do a breath test, and remember what I said, right? Urea gets metabolized to CO2 and ammonia, the ammonia is what screws up the stomach acid but the CO2 is what they’re measuring on the breath test. So the typical testing methods are CO2 via the breath test.
Evan Brand: Yup.
Dr. Justin Marchegiani: We have blood via the IgG, IgM, IgA, which is an indirect immune response looked at via the blood. We also have a villous or a gastric mucosal sample because we’re looking at trying to clip away a piece of that maybe H. pylori in the stomach or first part of the small intestine, but you know, if we don’t get it, that could be like putting a bucket in our—in our lake and pulling it up and saying, “Oh, it’s just water. That means there’s no fish in the lake.” So we don’t wanna just also have that same mindset and say, “Well, look, there’s no sample there. Well, the doctor may have missed it.” It’s very possible that that could have happened. We also have—we also have your stool antigen test which is a great test to look at. We like Biohealth stool antigen, and then we also have genetic test like PCR, polymerase chain reaction. We use a handful of labs like GI-MAP or Diagnostic Resource Group, and they’re—they do really good work and anyone that wants to get access to those labs, check out either Evan’s site or my site for access to those labs so you can get fully looked at, but again, we wanna look at it in conjunction with body system one as well. Just don’t make the mistake of just going after body system two. I’ve seen hundreds of patients get sicker doing that and they end up having to come back anyway and do it all over again and they waste a few months of their time and money.
Evan Brand: Oh, gosh. Spend—spend a couple minutes here, what happens to these people that ignore the order of operations?
Dr. Justin Marchegiani: Well, symptoms get worse, and again like I said, LPS is a toxin, so if you’re in the camp of having detox pathways impaired, right? And we could see that on organic acid test. We may see things like hippurate or you know, many of the different organic acid markers out of range—sulfate, pyroglutamate, right? These are all markers that bends the weight. These are markers that correlate to detoxification that could mean our phase 1 and phase 2 cytochrome P450 oxidative pathways are backed up and it may be hard for us to escort toxins out of our body.
Evan Brand: Yup, that makes sense.
Dr. Justin Marchegiani: So triple therapy is the conventional treatment. We use some different herbs in our clinic. We mentioned some of the biofilm agents, some of the binders. We use a bunch of various gut-killing herbs like clove or wild indigo, berberine herbs, mastica, oil of oregano, wormwood. We do different things like the ginger and again, it’s gonna be in the right dose, in the right amount. And the big thing—here’s the X factor, the X factor is do you have a co-infection along with the H. pylori. I have 3 patients this last week that not only had H. pylori, they had Giardia and they had Blasto.
Evan Brand: Oh, man.
Dr. Justin Marchegiani: Now what would happen if we just went after H. pylori alone or they just did the triple therapy for H. pylori alone?
Evan Brand: Yeah, it’s not gonna work. You’re still gonna have symptoms, that’s for sure.
Dr. Justin Marchegiani: Yeah, I mean let’s say you went the conventional route and let’s say, you added metronidazole or Flagyl in to kill Giardia. Well, great. I mean, the research only says that works a third of the time. Awesome. So now you—you roll in the dice. You have a 66% chance that none of that’s fixed and most doctors would never come, you know, even look for the Giardia anyway. So then you’re really set up for a world of hurt. So we wanna sequence things the right way. Typically, one infection at a time; sometimes we’ll do two if people have a stronger constitution, we’ll add in two. But you can see that we talked about the test. Some people may have to get all 6 tests done to evaluate whether or not they have H. pylori. I had one person recently took 4 times to get rid of the H. pylori. Most of the time it’s one or two, but sometimes it can take 3 or 4 and then we also know it can be spread pretty darn easily. In a lot of third world countries for instance, one of the main mechanisms is actually flies, because people are defecating in the streets. It’s like—I know like a lot of countries like India, I think 300 million people in India are still defecating the street. It’s crazy to think that because you know, that’s a third of the population in India I think. And if a fly goes in there and lands on someone’s stool that has H. pylori and then let’s say flies into your house and flies on your meal, you could easily get H. pylori vector that way.
Evan Brand: Wow.
Dr. Justin Marchegiani: They also talk about here—and we’ll put all these studies into the transcription so everyone can go look at it later but they also talk about vaginal secretions, being a mechanism for H. pylori so intercourse, husband and wife, that’s gonna be very common, and even saliva. So non-sexual relationships that may be intimate like you know, kissing your—your son or daughter, right? That—there’s still a saliva interaction or even just sharing silverware or—or food or glasses. There could still be a connection there because we know saliva is a mechanism and we know vaginal secretions are also a mechanism, too.
Evan Brand: I was trying to find a world map here, but it does show that in—this is just on PubMed talking about the evolution of H. pylori resistance to antibacterial agents that in Asia greater than or equal to 80% of the H. pylori cases are already resistant to the antibiotics in the first place.
Dr. Justin Marchegiani: Right, right. They are resistant to it and that’s what we see a lot on the—on the DRG and the GI-MAP test. We’ll see a resistance to that clarithromycin which is that typical—typical antibiotic used to treat it.
Evan Brand: Yup, and they have here talking about the metro—how do you say that one? Metronidazole?
Dr. Justin Marchegiani: Yeah, that’s Flagyl basically.
Evan Brand: Yeah, resistance to that one, too. The resistance isn’t as common in—well, it’s you know, greater than or equal to 20% in the USA and other developed countries, but that’s—that’s still massive.
Dr. Justin Marchegiani: Right, and just so you know, there’s not a ton of research on H. pylori being transmitted via vaginal secretions, but this paper here in sexually transmitted infections in 2000 is putting that out as a hypothesis. We’d have to look at more—more recent papers, but they talked about that it’s being a potential reservoir especially with the right environmental conditions, and they also talked about potential reservoirs for H. pylori or feces, the cheek—the cheeks, right? The kissing. Think food, saliva and dental plaque. So because these are potential reservoirs according to the research, it’s also a potential for it to be spread. Now we can’t say, is it a one to one? Right? When you kiss someone with H. pylori, do you get it? No. Because we have something known as IgA which is our local immune membrane killer that lives in our mucosal system in our mouth, in our gut, and vaginal canal or urinary canal, gut tracts, that can knock it down. So if you have good constitution and good IgA levels, you can beat it out. That’s why we talked about H. pylori being opportunistic, where there’s more stress, low stomach acid, lower IgA. Think of your defense systems being down. Think of the, you know, the old Star Trek film where the force fields are down. The Klingons can attack and their lasers hit a lot harder when the force field’s down than when it’s up,
Evan Brand: Yup, makes perfect sense.
Dr. Justin Marchegiani: Any other feedback you wanna give, Evan?
Evan Brand: I think that’s it. I think that was really good coverage. I was glad that we were able to zoom in, zoom out, and sort of paint a good picture here.
Dr. Justin Marchegiani: So I just wanna say to any potential patients listening. The diet piece is gonna be important. Cut the grains and the gluten and the refined sugar, and the junk out of it. Get the sleep and the blood sugar timing stuff down. But then if you’re still having some of these symptoms, the next step would be to evaluate body system one and two and three, maybe not all at the same time, but at least body system one and two to start, and get on a comprehensive program so you can move through the mountains or the woods, or that your healing journey confidently and not feel like you’re grasping for straws when there’s a—a setback that—that can happen from time to time.
Evan Brand: Right, so once again, here’s another piece that we’ve uncovered of why the diet and fitness industry has such a horrible success rate. Here you go.
Dr. Justin Marchegiani: Awesome. Well, hope everyone enjoys this podcast here. This is such a big issue that I see in my clinic, and I see it day in and day out. I see about 50 H. pylori cases a month and about, I’d say 30-50% of the population have this infection, but if you’re having symptoms at all or you just want to be—have optimal health, you should get the H. pylori eradicated and be infection-free. Everyone has the right to be infection-free.
Evan Brand: Definitely.
Dr. Justin Marchegiani: Alright, Evan. Great show.
Evan Brand: Take care.
Dr. Justin Marchegiani: Take care! Bye!
Evan Brand: Bye!
References: https://www.ncbi.nlm.nih.gov/pubmed/9625226
http://www.hsph.harvard.edu/nutritionsource/b-12-deficiency/
http://www.ncbi.nlm.nih.gov/pubmed/11218379
http://sti.bmj.com/content/76/6/489.full
http://www.mayoclinic.org/diseases-conditions/h-pylori/basics/definition/con-20030903
http://www.healthline.com/health/helicobacter-pylori#Diagnosis5