
In this week's episode, we explore the top 5 ways to heal leaky gut syndrome, a condition that can significantly impact your overall health. Beginning with a thorough understanding of the syndrome, we delve into the importance of a balanced diet and the key role that nutrition plays in healing. Further, we'll discuss the benefits of nurturing your gut microbiome with probiotics and prebiotics, explaining their sources and importance.
We will also highlight the intriguing connection between mental health and gut health, emphasizing stress management techniques for better gut wellness. Finally, we'll help you identify common gut irritants and suggest practical strategies to combat them. Featuring insights from experts in various fields, this article is your guide to restoring optimal gut health. Don't forget to like, share, and subscribe for more health-centered content!
In this episode, we cover:
01:06 – What Is A Leaky Gut?
05:13 – Gastro-Intestinal Permeability
06:06 – Nutrients to Help the Gut Lining Strong
09:42 – Probiotics and Prebiotics
15:21 – Physical and Emotional Stress
16:24 – Q & A
20:48 – Food Toxins
24:02 – Molds
26:33 – Q & A
29:59 – Autoimmune Elimination Diet
32:16 – Underlying Root Causes
35:38 – Q & A
45:17 – Takeaways
Hey guys, Dr. Justin Marchegiani here. Today, we're going to be talking about the top five ways to reduce and or heal a leaky gut. This is a really important topic. I see it all the time. Many people get confused about leaky gut. They think about leaky gut like it's its own entity, something you have to solve within itself, where really leaky gut is more of a downstream effect of a lot of upstream problems.
So I tell people anytime I see someone with a chronic gut issue, I just assume that there's some level of gut permeability happening downstream. To what degree does it matter? Because it's not going to change my treatment. So I might like to put my focus exactly on areas that actually change treatment. If it doesn't change treatment, okay, nice to know. Now, let's pivot and go to the actual solution.
So, real quick, excited to do today's podcast. Today, we're going to be diving into leaky gut and the root causes and the solutions again. Put your comments down below. I am live here as well, so if you want to chime in with some questions as we go, if it makes sense, I will answer it guys.
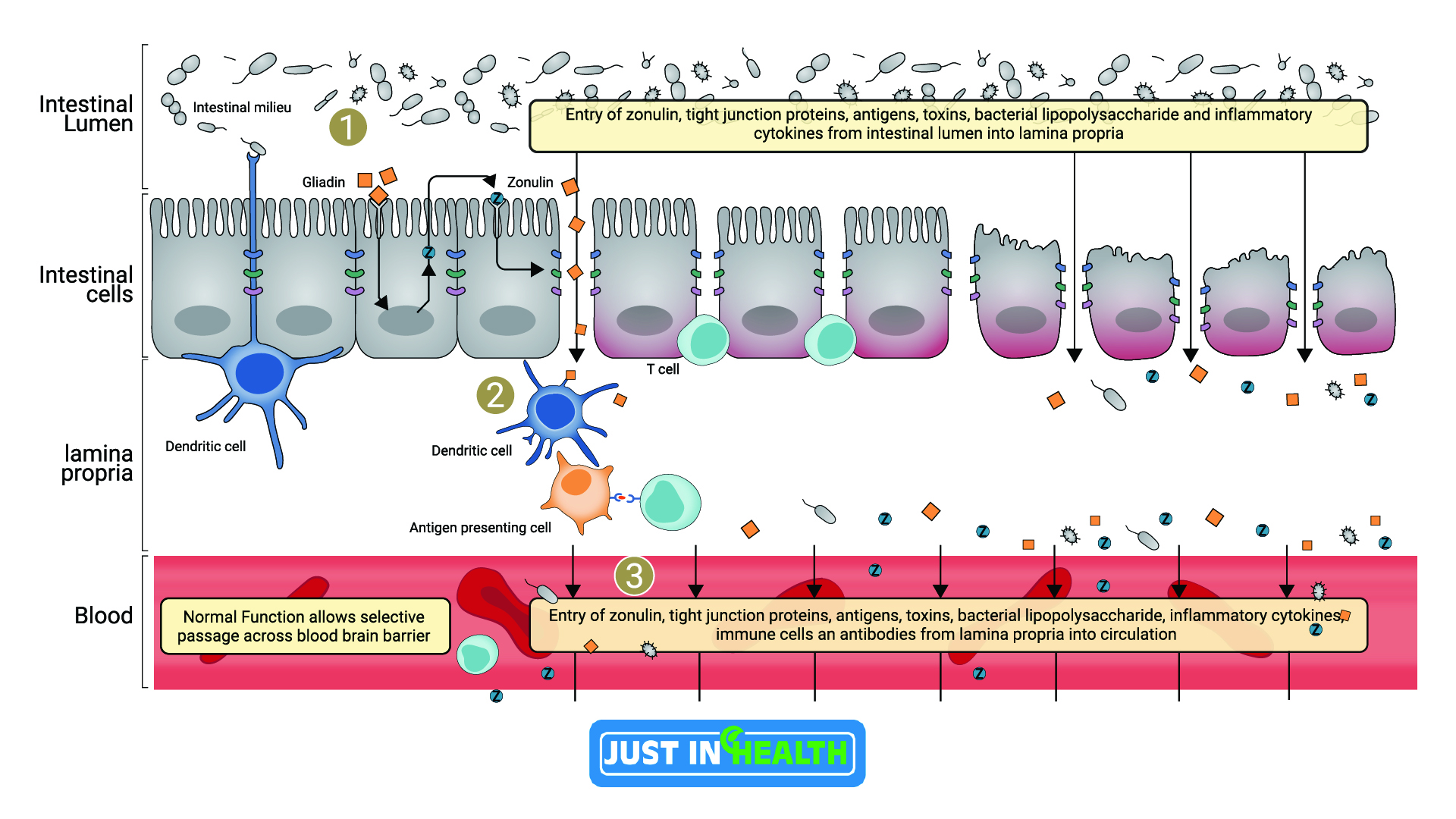
All right, so what is leaky gut out of the gates? You have this protein called zonulin. It's a protein, and essentially, put your fingers together like this if you're watching me on video. I'm putting my fingers together like in a prayer pose like you're saying a prayer. Essentially, this is your tight junction, this is your gut lining. Think of this as what happens in your small intestine. This is what prevents the outside and the inside of your gut. So technically, food's actually outside of you even though it's in your gut, and then it gets absorbed into your microvilli and it goes into your bloodstream, so it goes outside in.
So this is the barrier. This is your gut lining right here. And essentially, zonulin is a protein and that protein will essentially unzip that gut lining. I'll show you guys a couple of pictures so you can kind of get a visual here because I know it's a little bit confusing. Here's a picture of zonulin right here. Zonulin essentially will impair or increase the permeability of the gut lining. So when you increase zonulin, you're going to increase gut permeability. So for instance, there are studies on probiotics actually reducing zonulin and helping to heal gut permeability. We'll go into some of that here today as well, really excited.
So if you look at this right here, there's lots of different causes of gut permeability. Here's your gut right here, here's the gut lining right here. You can see these little proteins; this would be like your zonulin protein. These are the tight junctions that hold these gut cells together. And when we decrease, when we cause stress and we start to have zonulin go out of balance, this tight junction right here can unzip and then you start to get all of these bacteria, viruses, gluten, different toxins, different chemicals start to get into that bloodstream where normally there wouldn't be that exposure.
It would technically be outside of the body. So that's an important thing to look at. We have these tight junctions here. This is your fingers together. We have that zonulin protein and zonulin is going to cause that gut permeability to increase and we're going to go through the factors today and what actually drives that. It's really, really important. Essentially, zonulin makes the holes bigger. So when we have that increase in zonulin, it's going to increase the gut permeability.
Let's look at it a different way here. This is a really good one here. You can see in this particle here, gluten for instance. Gluten is one powerful stimulator to increase zonulin. Zonulin is going to increase with gluten exposure. You can see here the tight junctions right here. This is where my tight junction starts to slip apart and that's going to allow a more permeable gut lining. This is very important.
As the gluten slips in, you can see all the different immunological reactions that are happening. You can see transglutaminase, you can see T cells, you can see helper cells, you can see antigen-presenting cells. All this down below is just showing that the immune system is going wild and is attacking different tissues of the body.
So with Celiac, it may start to make transglutaminase antibodies and endomysial may start to attack and wear down the microvilli. So zonulin is that protein that helps to facilitate that unzipping effect. It's really important we want to do things to curb and reduce zonulin. That's the key. Zonulin is more of an effect, not a cause. We have to look at the underlying reasons why that zonulin is increasing.
All right, let's dive in here and kind of go over a couple of the big driving factors. So, factor one, we talked about what the gut lining is. Now in conventional medicine, most people won't respond to leaky gut. This is kind of like a slang, it's kind of fringy. What is leaky gut? When we talk about leaky gut, just consider it gut permeability or gastrointestinal permeability. It's like talking about adrenal fatigue. People aren't going to address adrenal fatigue. They're going to think that's hokey. So we talk about adrenal dysfunction or HPA axis stress because that's going to be more recognized in the peer review literature and through professional speak.
People think, “Oh, leaky gut. What do you have, sepsis? You're going to die?” They look at things and they kind of pathologize it. So we want to be able to communicate appropriately. So when I say leaky gut, we're really talking about the slang of gastrointestinal permeability. We're talking about the protein zonulin increasing and that opening up the tight junctions and that allowing different driving different proteins different components on the outside of the body in. So just keep that in the back of your head.
So, gut permeability wise, we talked about what that is. Next big driving factor: nutrition, all right? What are some of the nutrients to help that gut lining, to keep it strong, to keep the integrity up? Because these tight junctions, right, are made up of proteins, so you need good protein to hold, keep that gut lining integrity dialed in.
So one of the big proteins, there's going to be the protein that's going to be in bone broth. That's going to be glycine, glycine, and proline. So the compounds called proline-rich peptides (PRP), they'll extract that from colostrum, or we'll do glycine from bone broth, or we'll take collagen peptides. These nutrients and amino acids are very powerful. They provide a good building block for the enterocytes, these are the sites that make up that gut lining, so enterocytes glycine, proline, very powerful building blocks.
You can also use amino acids like glutamine, are also very helpful and provide a good energy source for the gut lining. So nutrients are very important. Again, protein, in general, is going to be incredibly helpful. We have to have good amino acids, good protein. Again, the more impaired your digestion is, the more I like collagen peptides, the more I like bone broth because these things are already broken down and more bioavailable.
You know, the biggest problem with the carnivore diet for some people is it's hard to break down a lot of protein. If you're eating a 20-ounce steak, it's hard to break that down. You may need enough stomach acid, enough enzymes, maybe even bile to be able to manage that protein and fat. So we have to make sure we have the ability to break down that protein, to break down that fat, because when your gut's impaired, when your gut's inflamed, your gut lining may be sensitive and you may not make enough enzymes and acids. One thing I wanted to show you here too-
Check this out: Mucus is also really important. The mucus provides a barrier on the gut lining. Now there's bacteria in the gut called acromancia that provide that mucous integrity, that help that gut lining stay strong and have that extra mucus bilayer. You also have cells, I think it's in the stomach as well, your goblet cells, goblet cells also help reduce mucus as well, and so they secrete mucin, which is that protective layer.
And so if your gut is inflamed, it's possible that those goblet cells will not produce adequate levels of mucus. So mucus is really important, the goblet cells are very important for that, and the more chronic gut inflammation we have, the more impaired those cells will be, right? We have the goblet cells that are producing essentially mucus that provide that gut barrier layer. We also have our parietal cells that produce hydrochloric acid, and they also produce intrinsic factor that helps us absorb B12. B12 is a really important nutrient for our blood to form, right?
If we don't have adequate levels of B12, we're going to form what's called megaloblastic anemia, which is essentially a really big goofy red blood cell, right? Red blood cells are opposite to humans, right? Humans start off small and get big, red blood cells start off large and undifferentiated, and they get smaller and differentiated, and if we don't have enough B12, they stay big and goofy and undifferentiated, so that's what a megaloblastic anemia is. Mega meaning big, and then you have the opposite, which is a microcytic hypochromic anemia, which is a micro small, really anemic blood cell.
That's going to be from low iron, and again, if we're not absorbing these nutrients, and we don't have adequate healthy blood cells, we're not going to be able to carry oxygen, and we're not going to be able to carry nutrients adequately. So very important on that front, nutrition, iron, B12, really important nutrients, glycine, proline, glycine, proline, and glutamine are going to be key nutrients there for the gut lining.
And I would just say being able to break down your protein as well, that's really key. Probiotics very powerful, love me some good probiotics. Again, some people get gassy when they take in probiotics. Let's take a look at this one, let's study right here, this is an excellent one. So if we go find here probiotics and zonulin, and this is very interesting. I wanna see if I can go back and get the actual…
So dysbiosis can trigger the release of zonulin, right? Zonulin is that protein that starts the unzipping action of the tight junctions when the tight junctions separate, that gut lining can open up, these enterocytes can open up, and then undigested and foreign particles can go through. So dysbiosis is a very powerful trigger of zonulin. Now when you have a lot of dysbiosis, the problem is this study is looking at probiotics, and it's looking at probiotics actually blocking that release of zonulin, so probiotics decreasing it.
The problem is if you have a lot of dysbiotic overgrowth, maybe call it SIBO, I just like the word generalized dysbiosis because then we don't have to get location-specific, that could potentially cause more bloating, more gas, more brain fog because you're probiotic intolerant. The analogy I have is it's like going out into a your front lawn full of weeds and just trying to throw down a whole bunch of seeds thinking you're going to make a difference, but really you have to do a better job cleaning out the weeds first and then coming in there and putting down the seeds.
Let me see if I can get the summary here, the conclusion, but it was very interesting in this study. This study here talks about probiotics and different pathogens, talks about the tight junctions, and essentially what they found is tight junctions are going to open up with different pathogens, antibiotics are going to impact it as well, and it's going to allow that gut lining to be more permeable.
Let me see if I can find this here. Discovery of zonulin protein with tight junction regulatory activity in the epithelial cell sheds a new lightning understanding of the role of the gut barrier in promoting health, as well as the function of different diseases. Such events lead to various extra dysfunctions. Pathogenic and probiotic bacteria and the compounds they secrete undoubtedly affect the properties of the intestinal barrier.
Coincidentally, there's an increasing number of reports, treatments, methods that target the gut microbiome, which suggests the prevention of gut barrier defects may be a viable approach. This is talking about from COVID's perspective, but if we talk about it, I just found it in the study earlier. Probiotics reducing zonulin.
Yeah, right here, this study right here. According to a meta-analysis, probiotics and symbiotics have a significant effect of reducing serum zonulin compared to placebo. This was a study I wanted to show you guys earlier. And this one here, the effects of bacterial infections and probiotics on zonulin. Probiotics have a significant effect of reducing zonulin. Some studies will actually show that prebiotics, which are like the fertilizer for probiotics, and probiotics together may not have the zonulin modulating effects as optimal as probiotics by themselves, so you gotta keep that in mind.
I typically always add in probiotics after we've removed a lot of the dysbiotic bacteria, as some of the studies showed a lot of this dysbiosis, and that can happen from processed food, indigestion, can happen from antibiotic exposure, but different dysbiosis can drive gut permeability. While at the same time, once we've cleaned some of that out, that's going to have its own effect of reducing gut permeability.
We add in probiotics shown to have a modulatory effect of bringing down that zonulin. And if you look at some of the studies that were out there, there was a doctor over at Harvard University, Alessio Fasano. He was one of the big studiers of gluten, and he had, he was back in an Italian University in the mid-2000s. He went over to Harvard. His big kind of claim to fame is looking at zonulin and its impact, and gluten being the biggest driver of it. But he was looking more for a medication to reduce zonulin.
My issue with medications is if it doesn't address the root underlying cause, it's going to tend to have side effects. That's the problem with it. It's like the Vioxx of 2003 when they were trying to block the Cox enzyme, acylo oxygenase enzyme. Well, the problem with it was, yeah, it helped produce inflammation, but that enzyme was also very important for the gut lining and the heart to repair. So when you block that inflammation from that enzyme, you had some good inflammation reduction effects, but then you also increased the chance of strokes and heart attacks and other gut issues because that enzyme was so important to building up that tissue.
And so you gotta be careful because if the root cause is up here, and you're managing downstream effects, inherently, you're going to have side effects, right? Same thing with the HMG-CoA reductase enzyme, that's the enzyme that statins work on. Well, you block that enzyme, okay, but the mevalonic acid pathway is downstream that produces CoQ10, so very important, right? Because that's really an important mitochondrial building block and nutrient to run the Krebs cycle and to run electron transport chain to produce ATP, so very important.
So if we go back here, right, we have talked about probiotics. Probiotics are going to have modulatory reducing effects of reducing that zonulin protein. Prebiotics as well, some studies will show probiotics more, some studies will show prebiotics probiotics less. Again, I always recommend adding things in one at a time.
Some people get bloaty and gassy when they add in prebiotics, and if that's the case, they always recommend go slow but add probiotics in first and do it after you've done kind of a kill phase, so you've kind of cleared out the landscape and you have a much better chance of being probiotic intolerant if you're just coming in and dropping a whole bunch of probiotics and you haven't fixed digestion, you haven't fixed food allergens, you haven't addressed any of the inflammation in the gut, you're more than likely to have problems.
Stress is a big one, alright? I see that quite frequently. There are studies on runners, for instance, going out for a long marathon run, training session, and testing gut permeability and seeing an increase in gut permeability. And why is that? Because of the stress hormone cortisol breaks down proteins. Well, the tight junctions are proteins, right? It's protein-based, protein-driven, that helps keep that gut intact.
And so the more catabolic you get, whether it's from excess emotional stress or excess physical stress, you have a greater chance of cortisol, which is incredibly catabolic, to break down that gut lining and increase gut permeability. So exercise is a big one. So you see it a lot with marathon running because it's very adrenally intensive, if you will. Could even be excess CrossFit. If you're really sore and you're breaking down that muscle faster than you can build it up, excess exercise could be a problem, taking cortisol out of balance and causing that tissue to break down.
And I'll pause for a quick second here, guys, and we'll just, answer or ask a couple of questions here. Could typhoid cause leaky gut? Yeah, I think typhoid could, right? It's a… I'm pretty sure typhoid's a bacteria. Let me just double-check on that, bacteria, virus. I'm pretty sure typhoid, yeah, it's a bacteria. So I would think it could be, absolutely. I mean, if you look at some of the studies here, right, some of the data here. I'll try to pull one up. Good image. So when you look at gut permeability, here's a great image right here. You see viruses, bacteria, gluten, toxins, all these things have a powerful effect on that gut lining, really powerful.
A couple more questions here for you guys. Wait, where do you get zonulin from? Zonulin's made by your body, all right. It's a barrier opener, essentially. When you increase zonulin, you increase gut permeability. And so, there are things that drive zonulin up, and there are things that drive it down. For instance, there are compounds that modulate zonulin for the better, like glutathione and vitamin D. Vitamin D has a powerful effect of reducing zonulin.
Vitamin D and zonulin – you'll see studies on that. Vitamin D is powerful in helping to reduce zonulin. Glutathione as well. Now, one of the things that increases zonulin is gluten, right? Your immune system will produce it. Gluten will increase gut permeability. According to Lessio Fasano, gluten was one of the top two stimulators of increased gluten, even in people that were gluten-sensitive – there are studies on non-celiac gluten sensitivity. They would see people that ate gluten, they'd measure zonulin, their gut permeability, protein.
More zonulin, more gut permeability. And they would see people that were in Celiac, they weren't even autoimmune, and they would see this increase in zonulin being produced with gluten exposure. So the whole idea is, “Hey, maybe I don't have to be Celiac, maybe I don't even have to be sensitive to gluten or even get bloated or gassy, and I'm still impacting my gut lining and increasing that gut permeability.” So really important to keep that in mind, yeah.
So exactly, John wrote in there increases the permeability of the tongue section is 100, yep, and that's by Fasano. Now Fasano was brought over by Harvard like I mentioned because they want him to, I think more than likely, to find a drug for it. I think there may even be something in the pipeline for it. But the problem with drugs like I mentioned with the Cox inhibitors of Viox of the early 2000s is you're not going to get to the root cause if you cause if there are other factors upstream that are driving the issue and then you're going to block it downstream, you're gonna create a side effect. It's going to happen 100 percent.
Can candida contribute to gut permeability? Yeah, it definitely can. So candida produces acetaldehyde, which is like a byproduct similar to alcohol that can be stressful on the liver. It also can spit off different mycotoxins as well, and mold can spit off mycotoxins that can increase gut permeability. All these things are factors in that, for sure. And if we look at this little art, this little part right here, let me see if I can find that picture again, but you'll see in the study here, it showed all kinds of different things, all kinds of different images of things that were driving the permeability.
Dysbiotic bacteria is a big one, and with people's processed diets, lots of acellular carbohydrates, that just means processed food. Right? Flours, grains, sugar, right? These things are going to feed and essentially flourish like a petri dish, all these bad bugs. So very important to keep that in mind, excellent.
Alright, keep on moving on here, guys. Talked about stress. So stress is important because if we are in that chronic sympathetic state, and we're over-secreting cortisol or maybe our cortisol rhythms are out of balance or maybe we're over because of over-exercise or inflammatory food like some of these foods like I mentioned, we talked about foods being a driving factor, right? Like gluten, casein – these are all driving factors. But can those foods also impact our adrenals and then make us less stress resilient?
So now when we start adding emotional stress on our body or physical stress on our body, now our system is actually going to be less resilient, right? A healthy nervous system is going to be more resilient and more adaptable. Unhealthy nervous systems are going to be less resilient and less adaptable. A little bit of stress comes your way, and it takes you hours to recover. We want a more adaptable, chameleon-like nervous system. Very important.
So now we talk about toxins, right? So we can just break it down really simply to food toxins. Gluten, casein – these are going to be powerful ones. Gluten and casein are powerful ones. Now, gluten has been a big deal over the last, I'd say, 50 years. Things have increased due to a lot of the pesticides. So Roundup or glyphosate is a big one. They used to just spot Roundup and spot it and use it, you know, like you could just on certain things to kill. And then what they would do is they would take a bacteria out of certain resistant plants. They found that these plants, you couldn't quite kill them with Roundup.
So instead of being very particular and going around with sprayers and targeting the weeds and stuff like they would with typical pesticides, they found this bacteria in certain plants that were resistant to Roundup. They took the DNA and what that was making that plant more resistant to it. They pulled that DNA out, spliced it into the wheat, and now you have Roundup Ready wheat. Now, what does that do? Well, now, instead of coming in and spot-treating pesticides as needed, and usually that was done, let's just say, earlier in the growth process, so a lot of that would be off the wheat in the grains when it came to harvest.
Now, they would actually take planes and just spray it through the whole field. So instead of coming in and spotting it, now you need less people, less workers, and you just use a big plane. And instead of doing it earlier on in the season, they would do it throughout the season. They found that if you use wheat even at the end of the season, the growing season, it would desiccate the wheat and actually dry it out. And that also increased the gluten levels, supposedly, and it also increased the zonulin, or I should say the Roundup glyphosate residue on the gluten on the grains.
So now you have gluten that has more protein in it due to the desiccation, and you have Roundup used later in the season, which created a greater residue. And so now when you take zonulin, you take all this glyphosate in, this Roundup, and that's going to now increase that zonulin because glyphosate is a powerful stimulator to increase zonulin, which makes your gut more leaky, more permeable. So very important.
So we have the farming practices being changed. Instead of spot-treating things, at first, we were using natural things. We would kind of rotate the crops, and then we started pulling the weeds. And then we would use maybe natural pesticides like diatomaceous earth, or you do white vinegar, and you do high doses of it. Now you have more chemical-based pesticides like Roundup is a chelator, so it would take typically, grab – it's a glycine-based molecule, right, similar to collagen, actually, which is interesting because glycine is an amino acid. But it would have, that's why it's glyphosate. And it would essentially pull away the minerals, it would strip the minerals.
So the problem with glyphosate as well, there's some data showing that it also decreases the mineral in the soil, thus making the plants less nutritionally dense. Because if plants don't have good mineral in the soil, it's a chance that they're going to make less vitamin C. They're going to have less nutrients because minerals and healthy topsoil predicate good healthy nutrition in the actual plant. They're totally connected. It's like you drinking toxic water and expecting you to be healthy from it, right? You need good healthy, clean water because your body is made up of that. Very important.
So our big toxins here are going to be glyphosate. We can throw mold in there, right? And we've done, I've done podcasts on where this mold comes from, whether it's in your home due to a leaky roof or we have chronic high humidity or a crack in the foundation, wherever it is. You want to look at it, find out what the underlying reason is, and then try to treat it as best of your ability. There are different tests you can do to assess that. Take a look at the Jeff Bookout podcast I did last month, all on mold, but at least getting some plate testing done is going to be a good start.
We'll put a link down for some of the plate tests, leave it open for an hour, close it, send it to the lab, and then we'll take a look at it and see what kind of molds there. But you really want to get to the root cause of why that mold is there. If it's a leak, address it. If it's chronic high humidity, address it. If it's due to like a basement crack, foundation, you want to look and get to the root of it outside the scope of today's podcast, but just keep an eye on that and definitely test it and assess it.
And you may want to look at testing your own urinary mold levels too. But first look at your home. That's easy. That's a little more simple, especially if you see mold in the wall or you have like drywall spots on the ceiling because water is leaking that gives you a kind of a tell-off something's going on there. Hope that helps.
So we have mold, we have, we can put other types of organochlorine pesticides are going to be negatively impacting, right? Definitely going to have some impacts on the brush border. They're going to be a stressor on our detoxification system because a lot of them are estrogen-based. Very important. Casein is another one. Casein is a powerful one. Casein is a major protein in Dairy. So in Dairy, you have casein, you have whey protein. Whey protein tends to be a little bit more anti-inflammatory and better. But casein is going to be a powerful stimulator.
Lots of correlations with casein and type 1 diabetes. Gotta look at casein from that perspective. Things like butter are going to have less casein. They're gonna have lower casein, lower lactose, and mainly butter fats. Now if you get clarified butter, which is essentially ghee, they're going to essentially heat it up, siphon the foam off on the top, and use the butter fat in the middle. That's what ghee is. And so it's clarified, so there's less lactose and less casein. I'd say butter is like 98-99% lactose casein-free, but for some people, that may not be enough.
And that's where case that's where a good ghee butter is better. I prefer to cook with ghee because of the lactose being skimmed off and the casein skimmed off. It has a higher smoke point, so you can have it on the stove top longer without it browning and oxidizing. So, I love cooking with ghee butter. I use it on my vegetables, or I'll put it in my coffee. That's what I did, my buddy. I'll do a two percent, I'll do unsalted butter on that one, grass-fed Kerrygold, my favorite.
Let me get a couple of questions for you guys. Only eat organic wheat if you eat it at all. Yeah, I mean, I would say try to avoid wheat if you're gonna do grains, try to make sure it's sprouted. The sprouting and the fermentation will, should they have the fermentation aspect, will decrease the amount of gluten in the grains. According to, I think it's the Celiac Society, they said that it's okay for celiacs, the Celiac Society, I think said it was okay for celiacs to eat not sprouted grains, but sourdough bread.
The fermentation of sourdough will decrease the amount of gluten in there. Now, I would typically say eat no gluten at all if you have any types of autoimmunity, none. But the Celiac Society is pretty on top of that stuff, and the fact that they think that sourdough is a better option is interesting. Now, sprouting grains is interesting because there's some data showing that sprouting actually increases gluten. The benefit of sprouting is you're soaking the grains, and what that does is it's going to deactivate some of the anti-nutrients, some of the lectins, some of the phytates, some of the salicylates, some of the anti-nutrients that can also be harmful to the gut lining because there are anti-nutrients in plants, right?
Animals have essentially teeth and claws, plants don't, and so they have anti-nutrients. And so different lectins, you're going to see them in nuts or seeds, so soaking that can also be very helpful for the gut lining. Cooking your vegetables, steaming them, sautéing them, especially if you have a lot of gut lining issues. We'll have our patients use an Instant Pot to cook their meal because that's going to really cook everything down, and you'll be able to utilize a lot of the broth to get nutrients in, and it really tenderizes it.
Think of cooking as pre-digestion, I tell patients a lot. If you look at the history of Cro-Magnon or Homo gastor, you'll see in a lot of evolution of our ancestors through access to nutrients. And so when fishing started to happen and we started getting the omega-3 fish out, that increased brain size, brain size created the advent of the hand ax. The hand ax allowed us to open up bones and get the bone marrow out. As we access more nutrients, these nutrients allowed us to then have higher brain function, where we were able to create weapons and weapons that were able to kill animals from farther away.
Now, this is important because if you're going after a bear with a spear, right, well, you're getting pretty close to an animal. That animal is big, you may not make it out in the process. And so, developing weapons that allowed you to be from far away, like a bow and arrow, allowed you to more successfully and safely hunt animals and get access to more nutrients, more amino acids, more fatty acids that would help your brain grow.
There's a reason why the raw material of the brain is mostly going to be cholesterol and fatty acids. People don't realize that, and so if your raw material is made out of this, right, cholesterol amino acids, the frame of my house is made out of wood, you would think that you would need more of that raw material to keep it strong, to keep it built up, right? So keep that in the back of your mind. A vegan vegetarian diet will not be the most optimal diet to support brain health because of that. Talked about the gut lining and Proline and Glycine and glutamine as well being really helpful building blocks for the enterocytes in for that gut lining as well.
All right, so the big toxins out of the gate: your typical organochlorine pesticide. We talked about Roundup and glyphosate. We talked about mold toxins as well, just kind of gave you a good cursory overview of where to look in those areas too. An Elimination Diet is going to be helpful because there'll be some people that may be sensitive to eggs, maybe sensitive to nuts or seeds. Until you want to look deeper because these foods are healthy, like if you're following a paleo diet and you're eating eggs and nuts and seeds, you may think, ‘I'm on it, I'm doing a great job,' and you probably are.
But that's why it's great to do an autoimmune Elimination Diet as well. Now, some people may even be more sensitive, and that's where the fodmaps go in, low FODMAP, or even going carnivore can be helpful because carnivore is the ultimate autoimmune and Low-FODMAP map diet. It's cutting out all the potential carbohydrate fermentables, right? FODMAPs, or fructo-oligo-disaccharide, mono and polyols, and those foods are going to be in probiotics, which are good, but they're also going to need onions and garlic and broccolis, and they can feed essentially be a primary fuel source for a lot of that dysbiotic bacteria.
So pulling that out can be helpful, cooking the foods down, a lot of the fibers down, can also be helpful. Carnivore is the ultimate because some people I've seen are really sensitive to even healthy vegetables that are low FODMAP. Just maybe the anti-nutrient load in those vegetables, maybe it's the salicylates, maybe it's the phenols, maybe it's some other anti-nutrient in there can be too much for some people, and so going full carnivore for some may make sense.
For most, I try to do an autoimmune lower FODMAP because you can at least get some carbohydrates, you can at least get some micronutrients in the vegetables. You can get potassium, you can get magnesium minerals from that. You can at least get maybe some safe starchy carbs, whether it's from carrots, whether it's from squash, parsnips, turnips, rutabager, those are some good options.
So outside of that, I hope I kind of laid some things out. When you look at leaky gut, obviously taking a medication for it would not fix the underlying issue because the proteins onulin are going up due to an inflammatory response upstream. So you cannot remove the downstream effect without removing the upstream cause. So just kind of keep that in the back of your head. We did it with Vioxx; we did it with all kinds of other drugs, and we have side effects. One out of three drugs the FDA approves ends up getting pulled from the market a few years later, right? So even all this phase one, phase two, phase three, eight years of study, one out of three drugs gets pulled after the fact. Okay, look that up, very important.
So think about the underlying root causes here. Root cause number one, make sure what is leaky gut. Zonulin goes up, gut permeability goes up, tight junctions are a protein. This protein is it keeps that those enterocytes intact when we increase zonulin due to the many different factors that we've talked about, whether it's gluten, whether it's not having enough good amino acids and nutritional support, glutamine, glycine, proline, good nutrition, good nutrients to help with oxygenation, mitochondria, iron, especially if you're anemic or Celiac, right? That's a big common factor, low B12, that's an impact.
If we are getting inadequate levels of probiotics, if we have a lot of dysbiosis, our probiotic levels are low, lactobacillus, bifidobacter, the different subspecies, if we have a lot more dysbiotic bacteria, klebsiella, citrobacter, pseudomonas, morganella, prevotella, these dysbiotic bacteria are going to increase endotoxin. They're also going to produce histamine. So then now you're more inflamed, you have all this endotoxic load on your liver, and then now you're overproducing histamine, so now you may be more sensitive to citrus, bacon, maybe you're starting to have wheels or urticaria or hives or brain fog. So it's important to get the gut bacterial imbalances knocked down.
Of course, stress makes a big deal. I told you about Marathon running studies and looking at gut permeability, excess emotional stress increasing gut permeability, and these things also lower IgA Sega. That's your kind of immune mucosal barrier that lines that intestinal tract. That's that first-line immune kind of defense. We have it in their saliva, have it like in our nose or our eyes or our ears, vaginal, urinal canal, rectum, intestinal tract, all there. That's your first line of defense for your immune system.
And the adrenal stress, the adrenals connect with that, right? Because if we're exercise stress, whether it's running CrossFit, whether it's emotional stress, they're going to play a big role with cortisol, and cortisol is very catabolic. Cortisol breaks down protein and your tight junctions proteins, a really important thing for that.
And toxins, mold toxins, moldy home, glyphosate, your different pesticides, organochlorines, those are going to be your big ones out of the gate. We could throw Mercury; we could throw lead in there, those are also going to be other driving compounds, driving toxins. So it's good to look at all that stuff. It's very, very important. And again, the main nutrients that are going to have a big role in modulating – talked about some nutrients that are important for good health, but the main nutrients that we're going to need for modulating are zonulin, glutathione, and glutathione is a sulfur-based amino acid, it's a tripeptide, it has cysteine, glutamine, glycine.
So glutathione is going to play a really important role with zonulin. Making some notes here, and like I mentioned, vitamin D, another one, vitamin D is going to keep that zonulin down as well. So glutathione, really important, vitamin D, really important, keeping inflammation down, really important. That's why we'll look at things like Epx or eosinophilic protein, or we'll look at cow protectant, these are good inflammation markers to look at what's (35:32) happening with the gut lining.
Yeah, ghee does have a great flavor, I totally agree. Leaky gut and colon cancer correlation, there probably is. I mean, anytime you see cancer, there's always going to be a correlation with inflammation and cancer almost always. You're going to see problems with vitamin D in cancer; you'll see high levels of insulin in cancer; you'll see high levels of estrogen and cancer. There's strong correlations for all those things absolutely.
There's a cologuard test that looks at inflammation, that kind of gives you more of a risk factor of where you're at with the propensity of cancer. But the problem with a lot of those tests is they don't really give you actionable information. I always look at tests and say, “Does it change my ability to dictate care? And what to do?” If it doesn't give me the ability to change things, it's just kind of like putting a thermometer outside. It just tells me what is okay. It's 98 degrees. I should probably wear shorts and a t-shirt. It doesn't tell me how can I change that, right? Not that you can change the weather, but in my analogy, we want to do things upstream that we can have a changing effect on here.
Can ox bile and enzymes cause die-off after a week of higher dosage. I mean, it's possible. Higher dose enzymes, especially can, you know, can go after things. I mean, typically, enzymes like that will be taken away from food by taking it with food. It's possible. It's possible you could have that effect. Too much bile, there's something known as bile acid diarrhea. So, I always recommend if you're like titrating things in, just start low and work your way up. So, if you're at two and then three, or three to four, and you notice more loose stools or some problems, just back off a little bit because it's possible you overdid. I know you had some good benefits getting your enzymes and bile up when we chatted last week. So just try to calibrate that dose.
If you feel like you're doing a little too much, just pull back on that a little bit and you may benefit with throwing in just maybe a little bit activated charcoal or bentonite clay at bedtime, just to kind of sweep up any debris that could be in the gut.
Is leaky gut always associated with autoimmune conditions? Well, some of the non-celiac gluten sensitivity studies showed people that essentially had no issues, no autoimmune, no celiac, no nothing, but they saw an increase in gut permeability, and so that's fascinating. Autoimmune conditions are on the rise, and so the way I look at it is we all have potential risk, right? And so the more we can keep zonulin lower, that's going to help our chance of our epigenetic predisposition playing out, right?
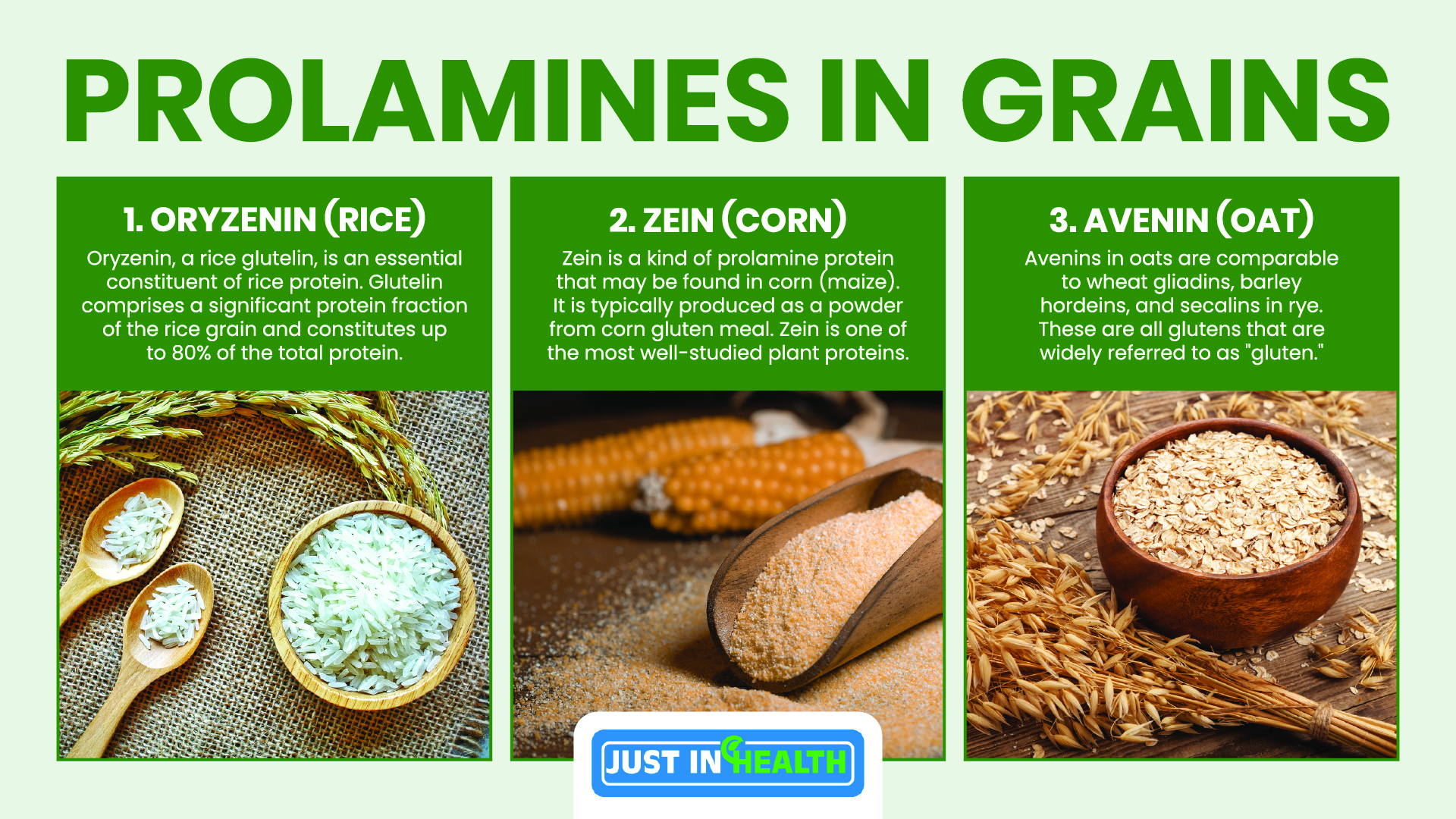
We made that genetic predisposition like I have Hashimoto's, but I'm able to keep my antibodies really low. Doesn't really express itself, and so I'm going to do things to keep zonulin in check, whether it's vitamin D, whether it's probiotics, whether it's keeping gluten and grains out altogether because other proteins like rice has oryzenin, corn has zein, oat has avenin. These are all prolamines, essentially glutens under the umbrella of prolamines, and they have a familiar resemblance, just like if you hung out with your cousin or brother, people may say you kind of look alike, right?
All right, guys, awesome questions. Do you think that one question here I wanted to hit it? Do you think that you are one of the best at interpreting the GI map test? Oh my gosh, well, I appreciate that. I would say I'm knowledgeable. I've done it thousands of times. You know, done it over the last GMS has only been out maybe seven or eight years, but I've been doing this for over a decade, almost a decade and a half now, so I have a lot of experience. I'll just say I have a lot of experience.
The key thing is I see a lot of people go over these tests, and the big thing is you have to look at what tools do you have in your tool belt based on the results that you see. Because a lot of people, they look at it, well, unless it's in red, I'm only going to do this one thing if it's in red, but what if this is a little bit out of balance? And then what does this tell me about my overall function upstream with my gut? If my function is not optimal, what other things can I do to bump up and improve my function so my digestion is better, my absorption's better, my immune functions better? So, there's a lot of little tweaks that I think can be done. The more insight you have, the more little tweaks you can make that will improve things upstream. So good question, though.
Don't take Colestyramine, I mean, it will make everything worse. I mean, so Colestyramine is a cholesterol bio-sequestering compound that was used to lower cholesterol in the early 80s, and they came out with statins in the 90s. And so yeah, it can create some side effects. You know, if you're going to lower cholesterol or, I should say, lower bind up mycotoxins, I like some of the more natural binders, whether it's fulvic minerals or bentonite clay or activated charcoal, but if you don't have your gut dialed in first, I would get your gut dialed in because that can create some constipation and slow down motility. Excellent guys.
Dr. J. King gallbladder. Let's see here, where'd your question go, Can gallbladder or liver issues caused leaky gut? Well, if you're not breaking down fat, it can definitely create inflammation with having all this undigested fat in your gut. I think it can, so I think it could be a contributing factor, having lots of fat globules there. I see that cause more diarrhea a lot of times. You'll see a lot of floating stools. You're not going to absorb your important vitamins like Vitamin A, which is really important for the gut lining as well, and so I would say it could be a contributing factor.
I don't know of a specific study on it, but I think it could be a driving factor. The problem with studies and functional medicine, here's why I hate studies in functional medicine. You got a lot of these people on YouTube. They're like, “Oh, this study, that study.” Here's the deal, most studies come about because people notice something. They work with patients. They're clinically having observations of someone doing well on this or someone doing well on that, someone, oh, the first doctor that ever cut out gluten at one point, right?
Which was William Dickey in the 1940s, post-World War II, he was in the middle of World War II. He's the Dutch pediatrician. He manages the pediatric ward in a hospital in World War II, right? The whole Nazi war that was going on. They had rationing from the Germans, and because of that rationing, they had to cut out wheat, barley, and rye, and so when they cut these foods out, William Dickey noticed like so many of his sick kids in the Pediatric Ward were getting better. He's like, wait a minute, what's going on? And then after the war was over, they added these foods back in, he noticed these kids getting worse again. He's like, wait a minute, something's happening here, and that's where he started to push down the rabbit hole of studying gluten and its effects on the gut.
So you can see the reason why we started studying gluten was not because someone said, hey, let's study gluten. It's because we were treating patients, we were noticing we were having observations of success, and we said, hmm, these are good results, let's study it more. So, I look at that. I think you can glean more data from clinical observation, and then over time, doctors say, let's go do studies on it, but it just takes years later to have the clinical observation and have the study to support it. So, if you're looking for data and studies that tell you what to do, you're like years behind the time.
I think it's good to say, hey, I'm having these observations, let's share it with colleagues so people know about it and they can do it themselves, and let's get some studies done in the meantime. But the problem with functional medicine, unlike the William Dickey study, we have these observations, we notice, is that in the functional medicine world, I call them levers or inputs. We work with patients. We're putting a lot of inputs into the system, meaning getting your vitamin D levels checked, I'm working on dysglycemia, I'm cutting out inflammatory foods, I'm making sure you're digesting your food, I'm making sure your bowels are regular, I'm getting you to bed on time, we're modulating cortisol, we're giving you extra nutritional support for nutrients that you're low in, low iron, low magnesium, low potassium, low B12.
Well, there are 10 inputs. Well, the problem is science, the gold standard is double-blind placebo control where they control variables one at a time. Well, there's like 12 variables right there. Good luck doing that double-blind placebo control study. They may just do one study and then say, okay, we'll do everything the same and then just take out vitamin D or take out, you know, you do one nutrient at a time, and that is just a slow boat to figuring out what is going on. That's part of the reason why functional medicine, it's so hard to do studies on functional medicine because of all the different inputs and the variables to the system.
And that's why you may do a study where you say, okay, let's just work on blood sugar, let's have you eat protein in every meal, all right, now let's have you do carbs at every meal, how did you feel, right? That's how research will be done. You would ideally isolate the variables, and in some way, you'd want to double-blind placebo control, meaning the person doesn't know what they're doing, and then the doctor given the intervention is not. That's the gold standard. It's really hard to do that in functional medicine because we're not just prescribing a single drug that is moving the needle. We're making diet and lifestyle changes that are holistic and across the spectrum.
Great questions, guys. I hope that helps. Hope you enjoyed today's podcast. Put your questions down below if you want to dive in deeper, you want more support, there'll be a link down below where you can reach out to myself and get support functional medicine-wise worldwide. If you want to dive in, justinhealth.com. There'll be a “Work with Dr. J” button where you can click that and get access to me and my staff and my team directly, happy to help you guys out, and again, feel free, there'll be a link down below for you guys to leave me a review, justinhealth.com/itunes. Write me a review, love it.
It helps more people like you get to access some good info and change your health. I just ask people just take one thing. Just don't get overwhelmed. Use that kaizen principle. Take one thing, apply it so you can get some kind of benefit, some kind of improvement in your life. Once you feel good and once you've mastered it, add one more thing. That's the best thing out of the gates, guys. All right, guys, hope you guys have a phenomenal day. I will be back tomorrow for more. Have a good one. Take care, y'all. Bye.
Mold Plate Test:
https://justinhealth.com/products/mold-test-kit/
Schedule a FREE Consult: Click Here!