
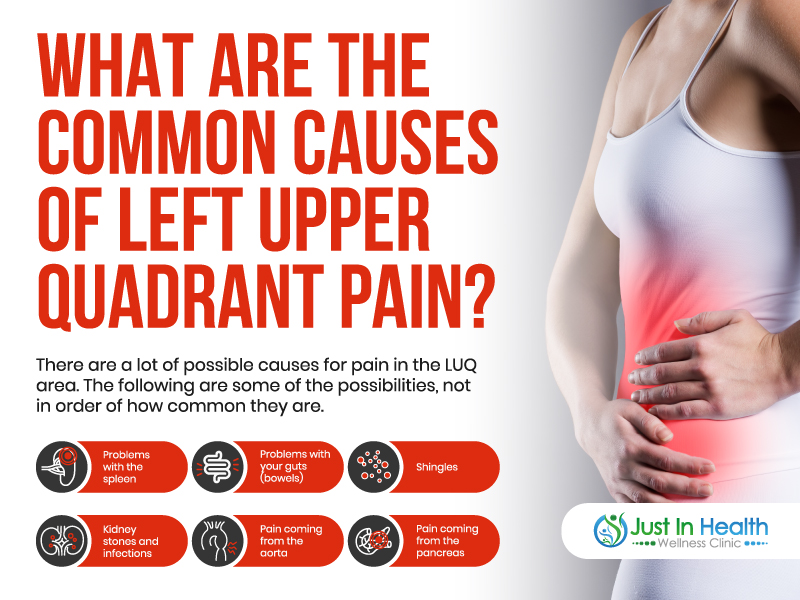
Pain in your upper left (UL) abdomen under your ribs can have a variety of causes. Several vital organs exist in this area, including the spleen, kidney, pancreas, stomach, colon, and lung. One of the most common origins of these issues is due to digestive problems. Heartburn typically happens when acid comes back up from the stomach into the esophagus. It can result in discomfort and a burning sensation in your chest. The pain can feel burning, sharp, or cause a tightening sensation.
Additionally, Gastroesophageal Bowel Disease, commonly called acid reflux, is a condition that occurs when you experience heartburn more than two times each week. Irritable Bowel Syndrome is also a chronic condition that involves a group of intestinal symptoms that usually occur together. The symptoms can differ in severity and duration from person to person. Inflammatory Bowel Disease (IBD) also includes any disorder that can cause inflammation in your gut; the most common of these conditions is Crohn's disease and ulcerative colitis. Dr. J and Evan emphasized that having your daily food and environment checked. Possible modification is a basic essential thing to do to avoid gut issues that can compromise overall health.

Dr. Justin Marchegiani
In this episode, we cover:
0:32 Stomach Burning and Irritation
8:48 Causes of Stomach Cancer, General Inflammation
14:27 Herbs
19:26 Bacterial Overgrowth causing Stomach Problems
27:41 Mood, Stress, Depression and Anxiety Conditions
Dr. Justin Marchegiani: We are live. It's Dr. J here in the house with Evan brand. Evan, how are we doing today, my friend?
Evan Brand: I'm doing great. You ready to dive in and talk about heartburn? One of the most common issues one of the trending issues that's always trending because us as a modern society, we have a lot of issues with hypochlorhydria, which is the technical term for low stomach acid. And so you and I are going to break down some of the reasons some of the root causes some of the triggers, and then some of the solutions. So where do you want to start?
Dr. Justin Marchegiani: It's a great question. So out of the gates here, we're chatting about what h pylori stomach burning stomach irritation, so there's a lot of root causes here. I would say out of the gates here, let's hit H. pylori first.
Evan Brand: Let's do it. So I had H. pylori. So I'll tell you from personal experience, and you and I clinically have seen many, many, many cases of H. pylori, let's start with a conventional approach to it. So first of all, the testing for H pylori is not very good in the conventional world. And there's an issue with false negatives. Luckily, the DNA stool test that we use is very effective, and we can find it very accurately. And conventional treatment is going to be what's called triple therapy, or sometimes quadruple therapy, which is three or four antibiotics at the same time to try to kill this helicobacter infection, which if you look at the microscopic photo of it, it kind of looks like a jellyfish, it's got this creepy little look to it with a creepy little tail. It's not a pretty little bugger, but man, it causes damage to those parietal cells which secrete stomach acid. And this is something that was very controversial for many times until the researcher actually infected himself with H. pylori and gave himself an ulcer. Right? You and I talked about that story before.
Dr. Justin Marchegiani: Yeah, that was Dr. Marshall. I think in the in the mid 80s. He couldn't get funding for his research. So he's like, hell, let me be the subject. And so he just infected himself with it. And h pylori, like you mentioned, is that he had a co shaped helix shaped kind of bacteria that kind of burrows into the gut lining. This it's controversial because, well, I shouldn't say it's controversial, we know that it can cause ulcers and stomach inflammation, we know that it can affect acid secretion. Now, a lot of people complain that it's an increase your acid levels, H. pylori tends to actually decrease acid levels. It creates an enzyme called urease, which takes the metabolite from urea protein metabolism, it turns it into co2, and then also ammonia and ammonia is got a pH of 11. So in the typical urea breath test for H pylori, they give you a bunch of urea. And the whole thought process is if you have h pylori, you're going to have more of that urease. And that urease is going to convert that urea into ammonia and co2, then thus a positive co2 level is going to be give you the H pylori indicative for a breath test. Now that ammonia has got a pH of 11. So it will start to neutralize and start to move your stomach pH in the more alkaline direction. So kind of one to six is going to be your acidic scale, okay? One is going to be 10 times more acidic than two, two times 210 times more acidic than three, and then you get to seven, which is going to be neutral, that's your water. And then everything above that base are alkaline, right? And so ammonia is that 11. So you're taking that pH in your stomach that should be around one and a half to two and a half and you're moving it more neutral. And so of course, that can affect a whole bunch of problems in your stomach from indigestion, dyspepsia, you're not breaking down your proteins, you're not activating your enzymes. And also H. pylori can thin out that gut lining. So part of the reason why people feel like it creates more acidity is because your gut lining gets thinner, your gut lining gets thinner that's making you more sensitive to acid in your stomach. It's kind of like if I got a sunburn, right? If I got a sunburn, and I went out the next day in the sun, did the sun get hotter? Well, it feels harder when I'm in the sun with a sunburn, right? Did the sun get hotter? No, it is your skin's more sensitive. That's when you're out in the sun. It feels like it's 150 degrees out but it's not. It's the same thing with your intestine you got a sunburn got that feels more irritated. Thus that acidity the acid that you're putting in there may cause some irritation just like going out with a sunburn.
Evan Brand: Yeah, that's great analogy check your microphone to it sounds like it may switch to your headset, make sure it's on your USB and I'm going to riff on h pylori for a minute because my personal experience with it was not fun. I lost a lot of weight and I was kind of freaking out honestly like I lost so much weight and I couldn't stop it and no was no shortage of calories. I was eating plenty of good meats and good fats and I just kept losing weight and I think h pylori is really one of those big stepping stones or maybe the better analogy is the domino effect. And once the age polarize there, as you mentioned, it kind of in activates your enzymatic process. So your pancreatic enzyme function, the release of the stored bile from the gallbladder is going to slow down or be reduced. So this is what I think leads to a lot of the SIBO or the bacterial overgrowth dysbiosis problems that you and I see clinically because when we find h pylori, we go down to page three of the stool tests and then boom, now we see Prevotella and klebsiella and Pseudomonas And all these other bacteria that are thriving so many people have heard of SIBO because it's trendy, and they'll come in and they'll do SIBO protocols. But if they don't get rid of the H pylori, I'm convinced that's one of the smoking guns that allows the dysbiosis to take place. So, long story short, if you're someone listening, if you've treated your gut before using antimicrobial herbs, or possibly even antibiotic therapy, and you didn't get better, or maybe you got better and you relapsed, consider that you've missed one of two things mold toxin, which is weakening the immune system or number two h pylori, and it could be coming from your spouse. So if your spouse is not being treated, they could have reinfected you and that's why you're on the merry go round and you can't get off.
Dr. Justin Marchegiani: 100%. So h pylori is one of the first things now, people say, well, a large percent of the population has h pylori, and that that is true. And so the question is, are you immunocompromised with that h pylori is an issue we're not. There are a lot of people that can survive on four or five hours a night sleep. But once you become stressed, and your adrenals become dysfunctional, and your diets been poor for a while, that four or five hours of sleep may not be enough. So you have to look at the context of the person for sure.
Evan Brand: Yeah. It sounds decent. It could just be the bitrate or something I do believe you have it on your USB now. It just sounds like it's a little grainy, but it I know on our local and it will be just fine. So it's, it's plenty good enough for today.
Dr. Justin Marchegiani: Okay, excellent. All right. So out of the gates here, just kind of hitting all the right things that we're chatting about. So we talked about the susceptibility for H. pylori, right. h pylori is going to be one of these things that may be a problem in people that have symptoms. So if you have symptoms, if you have issues, we want to look at that and the gates for sure. I think that's gonna be a top priority. Anything else you want to highlight regarding other infections? I know SIBO was another one that could potentially affect digestibility and your stomach cebo is going to hit more of your small intestine, but some of that bacteria overgrowth can move its way and migrate to the stomach as well for the gastric area.

Evan Brand: Yeah, well, I think H pylori is probably the biggest smoking gun but like you're not talked about many times, you can have permission to have multiple things wrong with you. Right? You said that so it's funny because we'll see Candida will see bacteria will see H Pylori, which is bacteria will see parasites will see worms. So the cool thing is when we come in with the testing, we're often using full spectrum herbs. And what I mean by that is we're going to try to knock out Candida bacterial overgrowth, the H pylori, the parasites, often we can do it in one fell swoop. And it's really fun to do this in children or young adults, because they tend to get better faster. Like if I see a five to 15 year old kid and we're working with them. It's amazing how much faster they get better than like a 70 year old adult, for example. It's something that I think shows the immune system being weak long term, this can be a bigger problem. So when you hear about stomach cancer, and the ulcers and esophageal problems, and GERD and some of these more scary diagnosis, these, these are likely more long term infections, or it could be the virulence factors, which are something that we test for if you look into the research, H. pylori by itself is not going to cause a ton of problem in the short term. But when it has these virulence factors that essentially strengthens the disease, the way I think about it is like the little whale shark, or actually, whale sharks are huge, but the whale shark with the little fish that kind of swim under its fins, to me, those are the virulence factors, they kind of strengthen the main host there, they're allowing the H pylori to thrive, they're allowing that shark to do what he needs to do, they're helping to maybe eat parasites off of the shark, so they're kind of helping him hang around. That's how I think of these virulence factors. It doesn't change the protocol much, but when we see a ton of inflammation or when we see a ton of gut damage, it's good to be able to link that back to a stool test.
Dr. Justin Marchegiani: 100% here, the virulence factors are going to look at those cytotoxic proteins and it's a genetic susceptibility of this H. pylori is going to produce more toxins that are going to increase your chance of ulceration increase your chance of stomach cancer, increase your chance of just overall general inflammation. So it's nice to look at the virulence factors. Now we have a couple we have like Virdi, VagA, iSay, these different virulence factors, these are cytotoxic proteins. And so it's good to look at that. Now one of the things we'll also look at in regards to intestinal inflammation to kind of make correlations is we'll look at calprotectin. Calprotectin is another systemic marker that's excellent to look at, because it plays a major role with inflammation in the gut as well. And so that's a really good one. So it's like a C reactive protein for your gut. CRP is a basically an inflammatory marker for the body. C reactive protein. calprotectin is a protein produced by the white blood cells in the intestine. So when there's more inflammation, more cytokines, more interleukins, nuclear factor, Kappa beta, all these inflammatory presence, it's going to give you more of a window that that's happening now. It doesn't tell you what the cause of it is. So you need to do detective work and get to the bottom it's going to be usually one to four or five things. Something of infection, some type of food allergy, some type of immune stressor, whether it's exposure to mold or heavy metals, okay? It can also be gut permeability where things are getting into the bloodstream and you're having this, I mean, a logical reaction, those would probably be the big four out of the gates. And then I think, also just if you're eating a lot of junky inflammatory foods, omega six grains, a lot of pro inflammatory foods, those could also drive it too.
Evan Brand: Yeah, I would say there's probably an autoimmune component to right if you've got Crohn's or ulcerative colitis or something like that, that may elevate that. And I know some of the stuff we talked about, if you try to take our conversation and put it in front of your GI doctor, they may not follow us on some of this stuff. But they will follow us on the calprotectin. I mean, that's a pretty common marker that it's going to be tested in conventional gastroenterology. So if you're trying to like educate your doctor, if they're willing, enable cool, you know, send them this podcast, hopefully, they're open to integrating some of these things into their practice. But often, we've had many people that have been the GI doctors, 5 10 15 doctors before they come to somebody like us. And unfortunately, they've had very poor testing, and they've had very poor treatment. That's why they're still needing help. And we're usually at the end of the rope, which you would think puts a ton of pressure on us, but I think you and I are used to and I actually enjoy it. Because in contrast, what we do makes the other people look silly, and our success rate is so good that it's really it's a blessing to be able to have some of these tools on hand. And it's really fun and inspiring to be able to give people hope. And some of these chronic gi issues like heartburn or reflux or GERD, or some of these esophageal problems like what they call like issues with the LES to lower esophageal sphincter that can become very traumatic. And people think that surgery or drug is the answer. But we don't have to go there in the majority of cases.
Dr. Justin Marchegiani: Yeah. And also, when you start to have you know, a lot of dyspepsia, that's like the bloating, that's the nausea, the burping the belching, when you start to have that, right, that lack of acidity in the intestines, if you have a lack of acidity, you also have a lack of enzymes more than likely because acidity is an important trigger for enzyme activation, right, because a lot of our enzymes are pH sensitive. So if you don't have a nice low pH, they're not going to activate and also that bacterial overgrowth, and you can look at bacterial overgrowth in the stomach usually be a glucose breath test. Now, the conventional breath test that we use for like SIBO is we'll use a lactulose blood test, or lactulose breath test where you swallow a lactose solution. And then you're gonna, you're going to blow into a bag, and you're going to get a baseline and then you're going to swallow the lactose solution, and you're going to blow every 20 minutes. And you can sometimes see an increase in gas that first 20 to 40 minutes, usually being reflective of the stomach area, usually in that first 120 minutes gives you more of the small intestine. And if you do a glucose breath test, that's going to give you more of a window into what's happening in the stomach. Now, typically, what we do is i'm doing more of a store test and I'm getting a global look at bacterial overgrowth in the intestinal tract as a whole. Obviously, when we're testing stool, it's all moving through the intestine. So you can't say Oh, that bacteria is in that part of the intestine or that part of the colon or that part of the stomach, you can't really do that because it's all moving its way out and getting mixed up, right. So a breath test could be helpful for that. Now, for me, it doesn't necessarily change a lot what I'm going to do, because if I see him does a lot of klebsiella or citrobacter, or I see some h pylori or I see a lot of organic acids showing him parade or fenzbenzoate right are two three phenolacetate, right different markers indican. And that tells me we got some problem especially indicate indicates one of those bacterial overgrowth markers that also has to do with more increased putrefy protein. So that's going to be a good indication that there's some stomach issue going on and dyspepsia issue going on. So if I see that that's going to gear me in that direction to be focused on addressing the stomach. And when we do herbs, guess what you can't just target one part of the intestine, when you give these herbs is going to move its way through. Some of these herbs are going to target things more specific to h pylori like mastic gum or bismuth. But obviously, some of those are still going to have general antimicrobial benefits that will move down the entire intestinal tract. And some even have anti parasitic benefits too. So it's hard to just target things we do know there's a history of herbs that tend to be more selective to certain things in the intestinal tract.
Evan Brand: Yeah, great, great, great segue to into the herbs. So let's go into that now. And we'll be providing some links, we'll put them in the show notes. We'll put them in your podcast app. So if you're listening on your iPhone, you should be able to check if you're on Justin's podcast listening, you should see some links for his products. If you're on mine, you should see mine we have custom formulas that we've created in partnership with professional healthcare company so we don't use any kind of consumer manufacturing. Most supplement companies, they gather products from around the world and they just label them up in a warehouse and ship them out. But they're not professional. So there's typically not as much tests. If any testing at all purity potency, those kind of things are not well tracked, we're very anal about what we do, because we have to get results clinically. And if we don't, then people don't get better, and they don't come to us. So we have a legitimate reason we have to be of the utmost quality. This is stuff that you can't get through consumer, like Whole Foods, places, or Amazon, these are professional so that that's, you know, just a little bit about quality. But in terms of the stuff we're using, as you mentioned, we have different blends. So sometimes we're going to go with more of like a mastic gum, clove berberine, Wild Indigo blend, these are things that can be both anti inflammatory, anti microbial, anti antifungal, anti parasitic, and then we have some where we've got a little bit of gut healing nutrients, like we might throw in a little bit of some dgl into the blends. So now we're doing two things at once, which is great, we're killing but we're also soothing the gut lining, which is probably so irritated, as you mentioned, this thing is thinned out from the infection itself. And then we go into more of the antifungals, too. So we may stack. If we see on the organic acids, you've got an anti fungal need, then we'll throw that into on top of the anti microbial need. And that's where the magic really happens. There's a synergistic effect. So rarely Are we going to come in with just oregano oil or just garlic, we're likely going to use a combination of possibly 510 or even more herbs. And then if you want to comment on that, and then let's get into the the question of like, where do probiotics fit into this equation? What about digestive enzymes and increasing stomach acid? Where does that fit into this equation? So if you want to hit on the herbs at all, then let's transition.
Dr. Justin Marchegiani: Okay, so first off, I think people come in with stomach issues saying, Hey, I have an H. pylori issue. And that's it. So I think, one you have the right to have more than one infection or gut imbalances happening at the same time. So it's really important don't get myopically focused on one infection, there's probably multiple issues. You could have h pylori, you could have some level of bacterial overgrowth that involve other types of infections, like klebsiella, or Pseudomonas or citrobacter. You could have a fungal overgrowth, you could have a parasite infection, as well. So all those things can be present. And also, you're probably going to have a lot of dyspepsia where you're having bloating, nausea, indigestion because you're not breaking down your foods adequately. So you're going to need to follow my six R's right and moving the bad foods and again, that could be different for everyone. Some people that could be a paleo template, others it could be an autoimmune, it could be a low fodmap template as well could be a low histamine could be a gassers SCD template. So there's different templates we're going to plug in, depending on how sick or how chronic this issue is. And then number two, we're working on enzymes and acids to really work on digesting things better. And again, acids tend to be anti microbial. Also, bile acids, which are produced by your gallbladder are also anti microbial. So if you have biliary insufficiency, you're not breaking down your fats, inadequate levels of bile salts will create a a more hospitable environment for bad bugs to grow. So that's the second are placed enzymes, acids, bile salts, third are repairing the gut lining and supporting the adrenals and the hormones because the adrenals help really provide a good anti inflammatory environment. So if you have imbalances in your cortisol function, you may have a lot of inflammation that's not being managed by your adrenals. And then of course, on the repair side, you kind of hit it earlier. Some of the repair nutrients that we're going to use maybe glycine could be L glutamine, it could be zinc. Zinc is very helpful. A lot of studies showing that to be very helpful with gut permeability. I would say DGL licorice, aloe okra, vitamin A. These are really important nutrients that come down the gut lining early I also like ginger and manuka honey. Manuka is used in hospitals in burn units, because it's very anti inflammatory. So I like a little bit of manuka honey, and my ginger juice tea recipe is wonderful. Any comments on that?
Evan Brand: Yeah, that's delicious. I'm a huge fan, too. And the good news is, depending on what's going on, you could start soothing the gut a bit early. So as you mentioned, there is kind of an order of operations. But depending on the case, if someone's in real bad shape, we may come in with some of those soothing nutrients early. Let's talk about probiotics, too, because this is a confusing one for a lot of people. They just hear online, a podcast, a blog, a website, they'll hear probiotics, probiotics, I think it's time to just throw it in. And a lot of people have a bad reaction to that. I think we actually did a whole podcast on this, like when and why probiotics may make you feel worse, but why don't you give us just some sparknotes on that, when and why and how do we integrate probiotics entities.

Dr. Justin Marchegiani: So people tend to have stomach issues in general because they have this bacterial overgrowth in the gut, that's going to affect the esophageal sphincter from closing. They also have a lack of enzymes and acids. So the food's rotting, it's putrifying, and transfer defying and creating lots of different gases as a result. Now, people tend to have a lot of bad bacteria in their gut, they tend to be very sensitive to fodmaps fermentable carbohydrates, fructose, oligo, disaccharide, mono and polyols. And again, probiotics tend to have fodmaps in it because probiotics are inherently fermentable right fermentation breeds bacteria, good bacteria growth, they can also breathe bad bacteria growth, right? And so if you're consuming a lot of probiotics and you have a lot of bad bugs, it can really create a feeding frenzy just like throwing chum in the water. When there's sharks around. It creates a feeding frenzy. If you go to your local Lake, I go down to Lake Austin and start chumming the water, right? Well, there's no sharks down there. So you're not gonna see any sharks come in, right. And so think of probiotics and a lot of fermented bowls. They may be reasonably good and healthy for you. But if you have sharks in that water, and you chum the water, you just create a feeding frenzy.
Evan Brand: Wow. And that you're saying, with probiotics, you're not necessarily even talking about prebiotics?
Dr. Justin Marchegiani: Correct. Again, people that have more extreme fodmap and SIBO sensitivity. That's where probiotics start to become more of an issue. You can still have some SIBO and fodmap sensitivity, and you may not get rise to the level where probiotics are problem, right? So people that are out there and having problems with their kombucha or their sauerkraut, you know, it could also be a histamine issue, because probiotics and fermentable are also high in histamine so they could dovetail and be a couple of different things happening at the same time. Either way, if that's the case, we still have to work on fodmap restriction, because when we deal with gut bacterial issues, we starve on one side with diet changes. We kill on the other side with specific antimicrobials, and then we crowd out and overpopulate on the last component so we we starve kill and crowd.
Evan Brand: Yeah, that's great. And then the saccharomyces comes into the equation too, right? Which is kind of marketed and sold as a probiotic, but technically is a beneficial yeast, I love saccharomyces it's something-
Dr. Justin Marchegiani: It crowds out it crowds out so it has beneficial effects of crowding out and also is shown to be very anti cdiff. Anti h pylori, anti blasto and it has immunomodulating benefits increasing IGA levels too.
Evan Brand: Yeah, we love saccharomyces it helps them mycotoxins too. I've seen it in a lot of people. And when I talk with Dr. Nathan, who is a guy who treats a lot of mold patients, he talked about saccharomyces being great for specifically, I think it's actually metabolizing, or changing the structure of the mycotoxins to make them more water soluble, but there may be sort of a crowding out effect with the mole too. So it's just a great overall thing. So if you're working on a gut healing protocol, and you haven't used saccharomyces, that may be something to chat with your practitioner about, it may be something great to add in.
Dr. Justin Marchegiani: Yep, I like it, that makes a lot of sense to me. So when we have that upper left quadrant pain, right, your stomach for the most part is going to be just right in usually this area here. So this is kind of your, this point right here is your HCl point. And this points more of your enzyme point. So like pancreas, small intestine is like really right here, stomach's usually going to be right in this area here. And then you have the esophagus, going up here, obviously, right, and then this esophageal sphincter can stay open. When we don't have enough acidity and we have bacterial overgrowth, then you can have a lot of that regurge of that reflux happening when we have inadequate levels of assets. So one thing if you kind of take your hand right here, and you follow the sternum down, right, we're kind of tucks into the left, if you rub it a little bit, and it's a little bit sensitive. That points normally sensitive anyway, but if it's really heightened, is a chance there's inadequate levels of HCl in the stomach. So that's a good little kind of pressure point there.
Evan Brand: Yeah, and people listening that can't see he's showing this down right there at the sternum, and then you can follow the rib line down to the left, or you could follow it down to the right, and you could check both sides. That's a really cool thing that you can do in person when you're working with the practitioners, you can palpate these points. And I remember when I was in one of my schooling lessons, we were with the teacher, and we had a lady who lay down on the table and everybody was coming up and palpating and man, this lady about jumped off the table when we hit that HCl point. So of course, we didn't have a stool test on her but man, I bet she had some infection going on.
Dr. Justin Marchegiani: Yeah, and it's good to rub that and then you can kind of rub a couple other spots to see if it really is heightened and then you can also start start treatment. Right, make diet changes, add in support, right? start addressing microbials down the road and see if that changes but again, the biggest thing I really want to highlight for people listening, we live in this antibiotic culture today, right you have an infection, antibiotics, antibiotics, antibiotics, and so what tends to happen as people are in kind of my six are step right the fourth are is moving the bugs right? replace the net or remove the bad foods replace the enzymes and acids and bile salts, repair the gut lining and the hormones remove the infections, repopulate good bacteria, pre probiotics, retest that fourth Rs a movie infections, people go to this first. We live in this like, antibiotic generation people are programmed Kill, kill, kill, kill, kill, it's the biggest mistake you can make. Some people can get away with it. If you're really healthy and you don't have an overabundance of inflammation, you can get away with it. Most can't. And they end up creating a whole bunch of problems. And I tell my patients the first rule of functional medicine right the first rule of Fight Club is don't make yourself more sick. It's really important So that's why that fourth R where that remove that second remove right the first removes the food. Right. The fourth R the second remove is removing the infections, we do it in that order, because we're trying to calm down the immune system, trying to support our anti inflammatory system so they can deal with inflammation and stress better. We're working on digesting and breaking down our food or working on motility that allows us set the table so we can come in there and wipe out the bad bucks.
Evan Brand: Yeah, he kind of alluded to it. But just to make it clear, you're actually improving your immune system by clearing out these infections. And some of these herbs we're using may have immune supportive benefits too. So that's just the real joy of what we do is you're boosting the immune system, you're letting the gut heal by removing the infections. It's just amazing. And when you get the spouse involved too, like if you're seeing a rebound case where husband feels great and then the wife sick and back and forth, you know, they may be passing the H pylori between each other even children who I mean I was sharing water bottles with summer my daughter when she was two, I tested her when she was two she had real high H. pylori. So I'm convinced I may have given it to her, I don't know. But luckily, we did herbs and she's in good shape now. And when we retested her the H pylori is gone. So I'm glad that we're able to get it resolved. But this is a problem that affects kids. So like when someone hears heartburn, they automatically picture old Betty sitting in the wheelchair with the gray hair and she's got indigestion she's got her santech in her hand. No, it's not just her. I mean, this could be two years old, this could be 10 15 20 30 40 years old. So don't discriminate. This bacteria does not care what you look like and how big or small your or anything. This is a bacteria that affects all people across the population. So if you have these issues, get tested, don't guess. And if you need help clinically reach out we work on this issue all the time, it's one of my favorite things to do is work on these gut infections. So if you need help clinically, we work around the world with people we send testing to your home, you do the labs, we get them back to the lab for reporting. And we jump on a call like we're doing now and we talk about it and we help you make a protocol help you fix your issues once and for all. So if you want to reach out to Justin, you can have his website, JustinHealth.com. If you want to reach out to me, EvanBrand.com and like I mentioned, we've got some links, we've got some gut healing products and some things that we're okay with you guessing on, there are a couple of things you could do out of the gate. But ultimately, you need to know what you're up against. Because as we alluded to, you may not have just h pylori, you may have other infections. So coming in with the glutamine, the zinc carnosine, that lm that kind of stuff that kameel, the ginger, the Manuka, it's awesome. But that may not be the right order of operations, it may help you by some time, but you got to clear the bugs.
Dr. Justin Marchegiani: 100% and there's a lot of studies out there looking at H. pylori, for instance, with a lot of mood and stress and depression and anxiety related conditions. And they find that when a lot of the H pylori is addressed, some of these changes occur as well with these issues improve or they talk about antidepressant drugs working better now. Now, why is that happening? Now, I believe the reason why it's happening is because when you address some of these bacterial overgrowth, you're absorbing your nutrients better, you're absorbing your protein, you're absorbing your fat, and in some cases, probably absorbing their drugs better, so they work better because they're in their system. Now, I personally believe if you're not breaking down your proteins and your fats, these are functional building blocks for your neurotransmitters, that you're going to have some issues in regards to your mood and your cognitive function and potentially energy because a lot of the nutrients and minerals and B vitamins have to get absorbed that way too. So if you have issues with your gut, don't just think hey, this is just a gut issue. Therefore my only symptoms are dyspepsia bloating, gas, nausea, constipation, depression, diarrhea, you could have fatigue, you could have cognitive issues, you could have mood issues, depression, anxiety, sleep, right. So we have to get kind of outside of the we have to go into the extra intestinal world meaning symptoms outside of just your gut related symptoms. And so it's possible if you've h pylori, you may only have fatigue and mood issues, and sleep and it's very possible. So you don't want to just get hung up on the digestive symptoms thinking I'm okay. You could have things outside of the gut area.
Evan Brand: Yeah, and you don't even recognize it. And the psychiatrist is certainly not going to suggest that our anxiety and depression is an H pylori infection. And that was it for me. I mean, I had panic attacks and anxiety. I mean, I was a wreck when I had gut infections. I will tell you personally, and clinically, I've seen the link between mood issues and gut issues. And I had a lady that I had maybe the last two months, I did not give her any anti depressant herbs at all. All we did is work on her gut and within six weeks, she said her depression was 90% better. And she just said it kind of nonchalantly and I'm like you said you were depressed for 20 years during our initial call or you're not realizing what we've done in six weeks just by working on your gut. We've as you self reported a 90% reduction in depression which you've had for 20 years. That is insane. That should be on the Billboard. That's Beyond the headline news, but I think there's just some ignorance about the link between gut and mood issues. So hopefully the psychiatric world and the gastroenterology world can start to get more integrated because right now they're still very, very separate which is no good for the population.
Dr. Justin Marchegiani: Yeah, here's an article in the get the Journal of gastroenterology research and practice. It's called the rule of H. pylori, and regulating hormones and functional dyspepsia. So if you get right to it, it says H. pylori strains have been shown to affect the secretion of several hormones including five five hyphen ht or five HTP. That's the serotonin melatonin precursor ghrelin which affects mood and appetite, dopamine gastrin, which affects HDL levels. So and then has, it might be the cause of psychological disorders of functional dyspepsia. So, essentially, there's a strong connection with H. pylori hormones, and a lot of the neurotransmitters and appetite regulating compounds so really important, right, H. pylori, we have to go above and beyond just thinking this is a digestive issue. It can affect mood, energy, sleep, and of course, hormones as well.
Evan Brand: You and I talked about this kind of like we're just like tying our shoes and cooking some breakfast. Would you have for breakfast today? Oh, I had some pastured eggs and bacon and sausage. What about you? Oh, yeah, handful of some avocado because, like we talked about it, like it's just so nonchalant. But I mean, if this were to be the headline news, like you and I, this podcast we just ate if this were to be like, the trending thing of the week and 300 million people heard this. I mean, we could put a huge dent in the world, I think we're doing a great job. We've got good numbers, but my God, if this was like the trending interview of the week, I mean, just imagine people would have so much more hope for their mental health, their physical health, their heartburn. This is empowering stuff here.
Dr. Justin Marchegiani: Yep. And don't expect your conventional medical doctor to know about this stuff unless they've gone through more integrative kind of nutritional, natural, functional type of continuing education. Most dermatologists don't even understand that your skin has a direct connection with your diet, right? They still have pamphlets in the dermatologists office saying what you eat has nothing to do with your skin. Most people that have eaten crappy and change their diet to be much more healthy, they can tell you one of the benefits you see is your skin, right? We know inflammation, and oil secretions all have a major effect with inflammation, grains and six junky carbs. While Same thing with our gut, there's that same level of disconnect all throughout medicine, because each, let's say medical specialty only knows their thing. And you know, when you're working 60 to 80 hours a week, you're not going to have the time to really keep up with the literature and what's happening. And, you know, if you're relying on your medical school training, well, typically that information has to be around for 20 or 30 years before it gets into a medical school curriculum. So what you're getting in medical schools, and they'll be 20 to 30 years behind probably at least 20 years behind time. So don't expect your doctor to be in the loop on this thing. So you got to really go outside of the box and, and educate.
Evan Brand: Yeah, I mean, I've got a very close family member who has a nanny for a well respected neurologist, and the neurologist home is filled with frickin mold. And no wonder the kid has a lot of issues and no wonder the mom has gut issues and the dad has brain fog and everyone's exhausted and they don't sleep good and they have skin issues. It's like your neurologist, those are mycotoxins. Those are killing your brain. Do you not know it? Nope. She doesn't know. It's crazy, man. So hopefully we can continue to do good work like we're doing and spread this word because man. Yeah, we're still in the stone age's and a lot of aspects.
Dr. Justin Marchegiani: Yeah, no, I think we're on top of it. Well, if you guys enjoy today's podcast, we really appreciate it, head over to EvanBrand.com or JustinHealth.com. You can subscribe to our email list. You can become a patient we work with patients all over the world happy to help you. Especially in the day and age the last year how things have gotten more virtual. It's great to have access to good clinicians and doctors, virtually so we can provide that for you. And if you enjoyed today's podcast, write us a review. Click Below the link you'll see a link for a review, write us a review. And also share this with friends and family. We appreciate it Sharing is caring. If you enjoyed it today, apply one thing, share it with one person that you love that could help them. Evan anything else?
Evan Brand: No, that's it. You did a great job and we'll be in touch next week. So take it easy and have a good one.
Dr. Justin Marchegiani: Have a good one y'all. Bye now.
Evan Brand: Bye bye.
International DSL GI MAP Genetic Stool Test
Genova Organix® Dysbiosis Profile