
In this week's episode, we delve into the fascinating world of skin and histamine from a functional medicine perspective. We begin by exploring the skin's multifaceted role as a barrier, a detoxification organ, and a direct reflection of our internal health. Then we shift to the topic of histamine, a crucial immune system messenger, often misunderstood and overlooked, that can significantly impact our skin and overall health when imbalanced.
Our guest expert, a renowned functional medicine practitioner, shares insights into histamine intolerance, discussing its often-overlooked relationship with conditions like eczema, hives, and psoriasis. Additionally, we touch on how diet, gut health, and genetics can influence histamine levels, and consequently, skin health. Finally, we wrap up by exploring holistic strategies to balance histamine levels, fostering not just healthier skin, but improved overall wellness.
In this episode, we cover:
01:48 – Topical Remedies
03:19 – Histamine – Gut Connection
05:13 – Molds, Antigens and Anti-Histamine
09:45 – Low Stomach Acidity
10:49 – Other Symptoms
13:55 – Functional Medicine Remedy Approach
16:31 – Mold Toxicity
21:57 – Adrenals
Dr. Justin Marchegiani: Hey guys, Dr. Justin Marchegiani here with Evan Brand. We're super stoked to chat about skin and histamine. We're going to talk about all things getting histamine and natural ways you can improve your skin and environmentally not getting triggered. Evan, how are you doing, man?
Evan Brand: I'm doing pretty good, except I had this mosquito bite this morning on my thumb, and it was itching. And I thought, “Okay, we gotta talk histamine and skin,” because, believe it or not, mosquitoes can still trigger a histamine response, even if it's not a bee sting. You can still get this itching response from it. So I took a histamine Mast Cell support, which is like a blend of quercetin, and geduchi, and perea leaf, and some of these other herbal Mast Cell stabilizers, and it calmed it down. I could have also taken homeopathic leadum, which is for insect bites. I think everyone should have homeopathic leadum on hand. Or I could have even used histaminium hydrochloricum, the histamine-reducing homeopathic remedy.
I was not an expert in homeopathy, but as you and I know, with kids bringing stuff home from school, I started diving into Homeopathy. It can be an incredible tool for stuff like this. Now, it's not root cause. I still have a mosquito bite, but it's a great way to tamp things down. Three out of five people we work with clinically, folks that are new to the show, we're functional medicine providers who work worldwide with people, helping resolve their issues by running functional medicine lab tests that we send to their door.
Then we jump on a call, review those labs, and make protocols. That's what we do. In the middle of all that, we see a lot of skin issues that are really linked to gut and histamine. We're going to break some of that down.
Dr. Justin Marchegiani: Totally. So, a couple of things out of the gate. We could talk about some environmental things like bites and things like that. We have eczema, we have kind of things that are more autoimmune as well. There's a big impact on food and gut permeability and gut bacteria, but some topical things you could take a penny and you could put it right on top of a skin of a mosquito bite because pennies, even though people think they're copper, they're actually zinc-coated. So the zinc on the outside of a penny can actually be very calming on that mosquito bite.
The second thing, my favorite thing, is witch hazel. And you want to get alcohol-free, and just, you want the pure astringent. You don't want witch hazel total, you want pure witch hazel, alcohol-free, organic and that is the best thing for any itch or any bite. It's anti-inflammatory, it's also anti-itch, and it does help with kind of the inflammation as a whole and promotes healing as well. So, love me some witch hazel.
The third thing which is going to be good just for the itch is going to be rubbing alcohol, isopropyl alcohol. That's also very good for just knocking down the itch. My favorite is witch hazel though because it has a dual purpose on the inflammatory side and the healing side.
Evan Brand: Yeah, I recommend witch hazel for hemorrhoids too. It's been pretty helpful for that.
Dr. Justin Marchegiani: Yeah, you just dash them on a cotton ball and then just, you know, dab that in there. And then also, if you have hemorrhoids, the root cause of hemorrhoids usually that bearing down and just kind of, the hemorrhoidal veins get inflamed. And also, if you have excessive wiping, a good bidet, we talked about bidets pre-show, bidets can be very helpful for just decreasing the friction on the wiping because you're just having a water stream cleaning your tush. And so that's a good option as well for decreasing inflammation that way as well.
Evan Brand: I don't think we've done a hemorrhoid show. Maybe we should do that. But yep, on the conversation of histamine, what I was saying is a lot of people you and I see clinically have skin issues. And the cool thing is we often improve skin issues by fixing other things, meaning we'll listen and we'll say, “Okay, I hear you on the skin issue. However, your labs reveal you have these two parasites, you have H. pylori, you have these histamine-producing bacteria.” See, there's a lot of dysbiosis in the gut that we talk about, but most people don't realize that you could be literally a histamine factory internally because of dysbiosis.
Dr. Justin Marchegiani: Yeah, you mentioned that. We know Pseudomonas, we know Klebsiella, we know Citrobacter, right? I had a conversation with one of the lead lab techs over at GI-MAP Diagnostic Solution Laboratory. They talked about the big bacteria associated with histamine production. That's going to be your Klebsiella, your Pseudomonas, your Citrobacter. So, you have this endogenous histamine, right? And then you have exogenous, right? That's coming from outside.
So, that's going to be all of the junk in your environment, whether it's pollens or danders or weeds or seeds or even molds, right? And so, if we can make your inside of your house pristine, that's going to be key. So, everyone, really good, higher quality HEPA filter with a VOC filter on it to really knock down those internal antigens histamines, that's going to be helpful. And then, like you said, you've got to go inside to get the endogenous, what your body's making. Exogenous, this is what's coming from the environment outside in.
Evan Brand: Yeah. And then throw in the dietary histamine component as well. So, at my worst, I remember using an avocado. Yes, I had a terrible headache from an avocado, and I thought, “What the hell?” And it turned out to be histamine-related. So, I cut it out for a while, started working on my gut, and it improved. And if people haven't heard my story, it was all mold. Mold was the big driver of it. Now, yep, Lyme, Bartonella, Babesia, some of these tick-borne infections, I've seen those as a massive driver of histamine intolerance and Mast Cell Activation as well.
But I think mold is really one of the bigger ones. And of course, we know mold increases dysbiosis in the gut. So, these are some of the big things you need to be looking at if some you're someone who's listening, if maybe you're stuck on Claritin or Zyrtec or some other allergy med, you're an ENT's not going to talk to you about this stuff.
Dr. Justin Marchegiani: Exactly. And so when it comes down to the gut bacteria, like you mentioned, that gut bacteria is going to obviously drive histamine. And then you have the exogenous stuff from the environment, and then the food stuff could be just enough to put you over the top with your histamine bucket, where maybe if the gut was better or the environment was better, that wouldn't be a thing. You wouldn't have to be that strict to cut out citrus or to cut out bacon or those kinds of things. But when the histamine bucket's full, it's good to pull out as many variables as possible. Would you agree?
Evan Brand: Definitely. Like corn blue corn chips and salsa, pretty delicious, but man, that's like a histamine bomb. So, if you're reacting to something like that, it's wise to lower the load. You can take things like DAO, the enzyme that your body naturally produces to break down dietary histamine. However, that is typically just a crutch. I mean, it's not going to get you out of the woods here if you have an internal problem going on like mold driving the histamine.
Dr. Justin Marchegiani: Yeah, most people, they are using things like DAO or quercetin or bromelain or N-acetyl cysteine, and those are great too. I like them because the typical H1, H2 blockers, whether it's Allegra, Singulair, Zyrtec, they're going to have a lot of side effects potentially, brain fog or other types of fatigue issues as well. So, I'd rather use something natural. Again, if I recommend those things, I'm always trying to fix the gut as well. There are some people that just have had allergies for so long and maybe their immune system is a little bit overly heightened, and that's where we fix the gut.
But it's good to use these things over a medication. And then like Evan talked about earlier, we're going to recommend a really good quality air filter, whether it's the Air Doctor or an Austin Air or an IQAir, something to get the overall load of what's in the air down. So those are all a couple of really big things.
Again, conventional medicine, like on the skin side, because we kind of have histamine topical with like urticaria, hives, rashes, eczema, the topical stuff that's typically recommended is usually a corticosteroid. Or on the natural side, maybe they'll recommend like calendula or something. And then we'll do like some of the witch hazel, some of those things to help. Typical conventional medicine will do corticosteroids. They may even do like immunosuppressant medications like Elidel, tacrolimus, those kinds of things to kind of calm the immune system down. But you've got to get to the root. So think about what's driving it from a root immune system kind of cause perspective.
Evan Brand: We'll think about people that go in for like a dental procedure and they get antibiotics, then they have some dysbiosis, some relapse with their gut, and all of a sudden, they've got histamine problems. Or maybe you get a tick bite, or maybe you move into a new home or a condo or an apartment, and all of a sudden… So I really encourage you, if you're looking at yourself and your story, try to plot the timeline, like, “Hey, after I moved into this new place, everything fell apart with my allergies. Well, why the hell didn't you have allergies before? Now you do as soon as you move in.” Well, I would investigate that environment. Something with your environment changed.
Dr. Justin Marchegiani: 100%. The environment's big. Also, people that just go and get surgery, we talked about your wife earlier, just the anesthesia that's given can have negative impacts on the microbiome. So even if you didn't get antibiotics but you got a procedure done, you should be on some good probiotics for at least a month or two afterwards just to make sure that you don't have this nasty rebound due to the anesthesia.
Evan Brand: Yeah, it's crazy how quickly you can get derailed by accident. It's not like they're intentionally wanting to hurt your gut and create histamine intolerance when you go to the dentist. And I don't know, let's say you get some tooth extraction or some deep cleaning and they send you home with an antibiotic. They don't know they're setting you up for histamine intolerance. They're just not thinking like that. They're thinking, “Hey, I don't want an infection going into the blood.” And that's the primary goal.
Dr. Justin Marchegiani: So yes, yeah, I agree. And so we talked about just the immune system, right? Most allergies, whether it's skin, whether it's topical, it's just an overactive, or I should say a very sensitive immune system. And we know 80% of your immune system is in the gut, in the malt, gastric-associated lymphoid tissue. That's your stomach. And then your malt, mucosal-associated lymphoid tissue. That's your small intestine. And so we know 80% of your immune cells are there. So if we have inflammatory foods coming in, that's a problem.
Sometimes your diet can be great, and it's just the higher histamine. It could be the bacon, it could be some of the citrus foods, right? That could be problematic when your bucket's already full. Sometimes it's just not being able to digest your foods, not having enough acid because you're stressed or enzymes because you're stressed or because you have a lot of bile, low bile salts. Those are all big deals. Plus, when you have low hydrochloric acid, that actually disinfects and makes it harder for bacteria to grow in your stomach. So just the idea of having low stomach acid, not having enough, that can make the bugs actually grow.
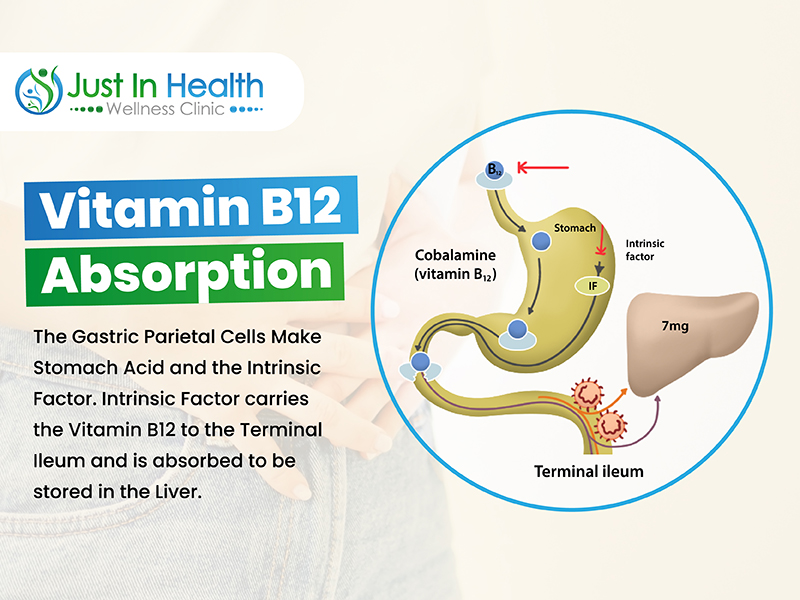
Evan Brand: Makes sense. So, in the case of H. pylori, which we see often, that's 51% of the population, give or take, has it, when it becomes too high, damages parietal cells, reduces stomach acid. You're saying that would also be a way that you could be set up for this histamine intolerance because of the hypochlorhydria?
Dr. Justin Marchegiani: Yeah, and then also, the parietal cells that make stomach acid are the same cells that make intrinsic factor which helps you absorb B12, right? It's a relay race. It hands the baton off in the stomach from the parietal cells to the intrinsic factor, and that baton gets reabsorbed in the ileum at the end of the small intestine. So, if you don't have that, if you don't hand the baton off with the intrinsic factor in the stomach, then you're not going to absorb that B12 at the end of the intestinal tract.
Evan Brand: I think we should paint the picture of what does this person look like, meaning, okay, they have some skin issues, they have some histamine problems, but what else do they have? I want to throw a couple of other symptoms into the mix that you may see because people, I don't think they make the connection between the mood and the histamine. So, histamine can act like a neurotransmitter, right? So, you may see irritability, anxiety, other neuropsychiatric problems.
What about fatigue? What about brain fog? Yeah, depression. Yep, strong mood connection. How would you say that people would manifest if they have a histamine problem in terms of energy, motivation? Do you see a role there or an effect there?
Dr. Justin Marchegiani: Yeah, I mean, there can definitely be the energy, the mood stuff. Obviously, we have the low-hanging fruit of urticaria, hives, itchiness. Maybe we have allergic shiners because we have a lot of lymphatic pooling underneath the eyes. We have those big bags under their eyes. It could be all of those different things. It could be excess itching, scratchiness, perioral dermatitis with excess histamines.
So, women are notorious for having it because they have higher levels of estrogen a lot of times. They have estrogen dominance or if they're on birth control pills, that can throw off the immune system and make them a little bit more sensitive. And then they can develop other types of dermatitis issues due to their hormone imbalances. That can throw things off too.
Evan Brand: Okay, so now you're talking about the estrogen-histamine connection.
Dr. Justin Marchegiani: Bingo. Yep, that can play a major role.
Evan Brand: Okay, and then what about issues with progesterone? Because I've noticed when I've done topical progesterone, it's helped reduce histamine symptoms.
Dr. Justin Marchegiani: Well, progesterone can go downstream into cortisol, so progesterone is actually very anti-inflammatory. And so, a lot of times, people that have low progesterone, a lot of times they're pulling that progesterone downstream to make more cortisol because they're inflamed. But when that progesterone drops, that further increases the estrogen dominance, which can throw off your immune system. So, that's why progesterone is super helpful for the immune, but it's also a GABA chloride channel opener, so it gets the GABA into the brain and really helps with relaxation and sleep. So, you may find that higher histamine, brain fog, irritability, mood stuff as well, and that progesterone is playing a role in it.
Evan Brand: Yep, okay. Sex drive, I've seen that to be affected as well in this whole histamine conversation. Some people, they may notice increased sex drive. Some people, it crashes and they're flatlined. Honestly, I haven't seen one way or the other.
Dr. Justin Marchegiani: With progesterone?
Evan Brand: No with Histamine.
Dr. Justin Marchegiani: It could be, you know, either one. Some people, if they have a lot of insulin resistance, you know, you can get a little bit of a bump in your androgen as a female, but that's also going to drive infertility. It can drive excess hair growth and acne. But you may get a little bump in libido as well. It's not necessarily good because it's throwing off your other hormones at expense.
Evan Brand: Okay, so let's talk about where should someone start if they have this problem, any of these issues? Maybe they take a hot shower and they get itchy, and then they eat something they think is affecting them, and then they think they're reacting to the pine pollen and they've got some diarrhea. Where do we start with these people from a functional perspective?
Dr. Justin Marchegiani: I think from a functional perspective, it's always going to be food and environment, right? So, obviously, food makes the biggest impact, but it requires some changes. It's actually easier just to probably get a really good air filter because it's just like, I make the purchase, I get it, I set it up, I put it on, and it's one and done. There's no real habit change. It's just on. So, I think a good air filter is good, doing some sinus flushing with some saline to clean out the allergens because you go outside, you're like, “Oh, I'm now I'm inside. I got my air filter on.” But you still got this colony of mold and antigens from outside in your nose. And so, you're like, “Oh, this air is all clean.” But get that junk up there, get it cleaned out.
So, we'll use some xylitol, whether I like the Xlear Max, which is a good one if you're really sensitive because it has aloe and some capsicum, which is the homeopathic anti-inflammatory. Or I'll do the Rescue, which breaks down those mold biofilms or antigen biofilms, and then you flush it out with some saline. Then you can get it out. Now you're breathing nice, clean air. That's an easy, simple one. And then the next thing is food. So, paleo autoimmune, I think, is a good one. And then we can be very histamine-aware, avocados, pork, making sure meat's not old, citrus, those kinds of things are good to be aware of.
Evan Brand: Yep. And then testing-wise, we obviously want to look at the stool. You and I talked about the histamine-producing bacteria, so we need to investigate, look at the dysbiosis. And it's actually a beautiful thing to see this on paper. So, people that have suffered for a while, 20 years or whatever, they're stuck on and off allergy meds, it's amazing to be able to show them, “Hey, look, you've got six different species of bacteria that are just through the roof.
So, we're going to address that dysbiosis with the help of the test to tell us where we need to look and what we need to use to fix it.” And we do not prescribe drugs, so we're going to hit this from a natural medicine perspective.
We're going to use different natural herbal antimicrobials. There could be parasites as well. That could be the H. pylori, which we may put in its own category. There could be Clostridia. I would say we need to do an OAT test too because now we're going to look at the neurotransmitters and say, “Okay, well, is all this anxiety and irritability coming from the histamine issue, the gut issue, and your skin? Or is it its own brain chemistry problem that we can fix as well?”
Dr. Justin Marchegiani: A hundred percent. Now, you've always talked about the colonized mold from the environment kind of working its way into the gut. I know you use a lot of OAT testing, which I do as well from Great Plains Labs, to assess that higher level of aspergillus or Fusobacterium. And is it colonizing? Speak a little bit more about how that outside environment gets in the gut and then how it grows. And then, can we do gut protocols to knock that down, or do we have to address the outside? Like, how do you address it holistically if it's outside coming in and impacting the gut?
Evan Brand: Yeah, so the two options that can happen for mold toxicity is you can become like a mycotoxin reservoir where you're simply just storing the mold toxin that you've breathed in. So, you're living, working, sleeping in a water-damaged building, you're breathing these mold farts, those are mycotoxins. They get stored in you. But when you do your OAT test, page one, you don't see any overgrowth there, numbers one through nine in the fungal category, if that all looks normal, but we see mycotoxins in the urine, we'll say, “Okay, you just have mold toxicity, but you're not colonized.”
But most of the time, it's both, especially if (you're not storing it in your gut. It's just from the outside coming in, you're not storing it.) Well, it could, (it's not colonized), yeah, it could be stored, but it may not be actively growing, whereas (in your gut), yeah, whereas when you see the active growth, that would be like foreign carbonyl glycine there's like three or four different ones, and say, aspergillus or fusarium. And truthfully, I think this testing still has a long way to go. I think we're going to find the ability to test way more molds because right now, all we can see is aspergillus, which is common, but there are tons of other molds that I think people could be battling, and we're not actually testing for them.
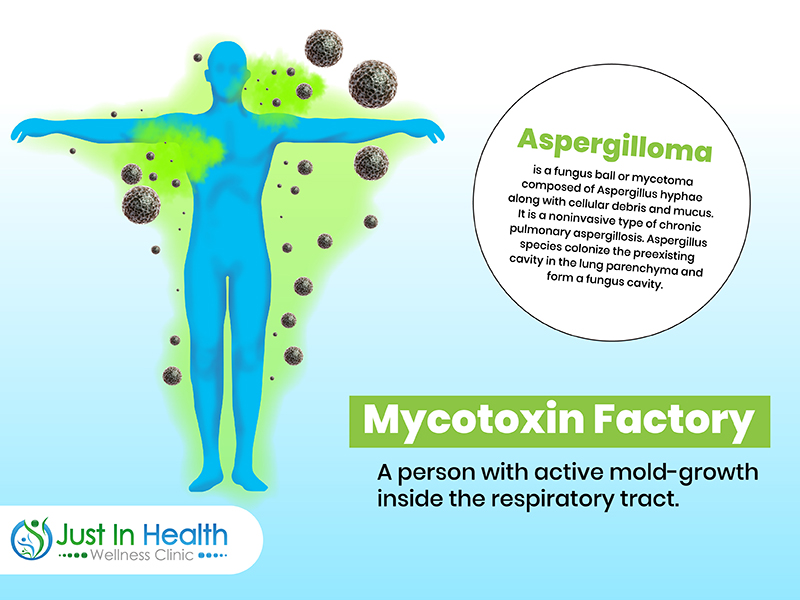
So, testing is not perfect, I will admit, but if we do see the growth, then we'll say, “Hey, you're actually a mold factory, more accurately, a mycotoxin factory. You're now generating mycotoxins from this active growth.” Meaning, if you move out of that moldy house, well, you could take the mold with you. And so, that's where using, to answer your question, that's where we're using, like, the rescue nasal spray is great, but then the same gut protocol will fix that because, as you know, a lot of the herbs that are used for bacteria are also anti-fungal as well. A lot of blends that you and I formulated, we have anti-fungals built into those. So, really, it doesn't change the protocol too much. We're probably hitting several things at once.
We may be killing mold and killing Candida and killing bacteria all in one fell swoop. And if you look into the literature on this, you can get something called an aspergilloma, where you can literally have, like, a ball of mold growing in the lungs. Now, I don't know if that's like nebulized anti-fungals or what. That's a little out of my wheelhouse. I don't know much about lung growth of mold.
But we can say for sure that where we're putting in oral anti-fungals, oral antimicrobials, we look at the OAT, and guess what? The retest looks beautiful. So, we know it's working. And then we match it to other symptoms, and they say, “Hey, look, I don't have sinus anymore. I don't have histamine anymore. I don't have insomnia or depression anymore. It's all cleared up.” So, I think what we're doing is working great.
Dr. Justin Marchegiani: Absolutely. And also, there's, you know, MARCoNS as well, like methicillin-resistant kind of staph coagulates in the nose. And that's where I'll add a drop or two of Betadine iodine because that's shown to be very helpful against methicillin-resistant bugs in the nose, and it's also a biofilm buster as well. And then I'm not sure, I think you do it as well, but we add biofilms to a lot of our protocols, whether it's the ginger tea, whether it's silver, whether it's NAC.
And NAC is great because it can help with glutathione and help with detoxification while it helps with the gut while it also helps improve lung health and breaks up mucus. And then also, like systemic enzymes, whether it's pancreatic enzymes or serrapeptidase or lumbrokinase. Yeah, those are probably the good ones out of the gate.
Evan Brand: I was actually reading about lumbrokinase this morning. Dr. Mercola had emailed about it. He had an article about aspirin and how much it could have saved people from, (oh yeah), you know. (the SIBO) blood clots, (yeah), of course. And so anyway, he talked about how he had a wasp sting, and he decided to go, I think he said he took 15 lumbrokinase, which sounds like too many to me, but he took like 15 lumbrokinase, and somehow, it healed him from the wasp sting because it didn't have enough time to coagulate and the fibrin didn't form. And it was this whole explanation he gave, and I thought that's cool. So even lumbrokinase may help or any of these systemic enzymes may help for bug bites. So, that was kind of neat.
Dr. Justin Marchegiani: Yeah, I like Wobenzym too because it's a pancreatic enzyme at high dose, and these types of things are wonderful on an empty stomach. They can really go in and help with thinning out blood, helping to break down interleukins and cytokines and all these inflammatory compounds that could be in the bloodstream. So, I like that.
Evan Brand: I take a blend every day of enzymes just because everything I've been through, I think I still need it. So, before breakfast, I'll pop a blend with the… Also, it's got a little bit of ginger in there too, and it helps. Yeah, I noticed a difference in my brain too. My mental clarity is better when I'm on the enzymes.
Dr. Justin Marchegiani: Oh yeah, does it help with blood flow across the board, whether it's blood flow to your private parts, your brain, to your muscles, it's going to help with blood flow everywhere, which is great. That's excellent.
Evan Brand: All right, so we hit the… Oh, we hit the stool. Oftentimes, I'm going to run, like, a Lyme co-infection panel as well, just to make sure we turn over all the rocks. I mean, truthfully, blood testing… I know someone like the Shoemaker-trained medical doctors, they'll run blood and they'll look at TGF-beta1 and some of these other, like, mold biotoxin illness blood markers. But, to be honest, it really doesn't change the game plan or protocol for me.
Dr. Justin Marchegiani: Yeah, it doesn't change it much. And then, you know, you can run, like, serum tryptase or, like, you know, whole blood cell like histamine, like maybe those are good if someone has a lot of histamine symptoms and you just want a baseline to see where they're at, so then you can come back and over time, maybe watch it go down. But for me, it doesn't change treatment. So, it's more just a marker of, “Hey, are things improving?” Just an extra yardstick to compare things to. But most of the time, if these tests cost hundreds of dollars, usually the best yardstick is, “Hey, Doc, I'm feeling better.” Right? “I'm feeling better. I'm improving.”
And then, we test the root causes, which are the bacteria, the gut issues, the hormones. Person in the chat says, “Hey, my cortisol is low. I have more issues to.” To a lot of skin stuff. And so, that's why that low cortisol, looking at the adrenals, can be helpful because if cortisol is super low, you may not have that internal cortisol to deal with the inflammation on the skin. So, getting the adrenals looked at and addressing the low cortisol internally is important because if not, they're just going to recommend cortisol on the skin issues.
Evan Brand: Yeah, the adrenal piece is awesome to look at. And one other thing about blood, it's not very fun to go and sit at LabCorp for however long and you have to get poked. I mean, it's not a big deal. Like, I ran blood a few months ago, and it wasn't a big deal, but I thought, “Wow, how inconvenient is it?” I didn't make an appointment. I probably should have, but I sat in the waiting room for like an hour. Luckily, I didn't have anything to do that day, but I just sat there and watched everybody complain. And I looked at all these people, they're all overweight, they all just looked terribly unhealthy. “My doctor sent me in here for this.” And it's like, you feel so bad for these people.
It's hard for me not to want to intervene and talk about organic acids testing. Like, “Hey, I want to just pass out in the waiting room because I'm like, these poor guys, they're getting conventional blood work, they're never going to get to their root cause.” Have you seen that meme online? It shows a person in a casket, and it says, “Your labs are fine” or something like that. They're in the casket, and the doctor's looking at them and says, “Your labs are fine.” So, long story short, yes, blood can be helpful.
If you're looking at cancer markers and you're working with maybe a holistic oncologist and you're tracking CA 125 and 19 and all these other cancer stuff, like, that's not my expertise. But what I will say is that blood can be a tool, but I often find that it's the only tool that's used. And as you know, because you and I've looked at thousands of blood panels, most blood panels suck, and they don't have enough data on them unless we're putting a custom panel together.
Dr. Justin Marchegiani: Yeah, I mean, you can glean some information and say, “Okay, let's run this test over here to get more insight.” Or if you see low vitamin D or you have thyroid issues, those are going to be good for that. It's going to be good, like, you know, homocysteine is a good marker, methylmalonic acid is a good marker. We get it in organic acid testing as well. Some of the coagulation, D-dimer is pretty good. You know, you can get some good insights in anemias or low iron. But yeah, like, it's good to have that plus, okay, why is the iron low? Oh, you have a gut absorption issue.
So, a lot of times, it still requires you to, like, that's the platform to now recommend other things based on that data. (Yeah. For sure, for sure.) Well, that's good. I mean, I think we hit everything pretty well. Anything else you want to highlight before we wrap things up?
Evan Brand: I think we've done a good job. I'll just send people back to the websites if they want further information. If you want to reach out, we do work worldwide. We send these functional labs to your door. You don't have to go sit in the waiting room for an hour. We send the stuff to your home. It's very convenient. These are great tests, and just because it's convenient doesn't mean it's not good. These are the best tests out there. We're looking into 75 biomarkers just on the organic acids alone. You combine that with the stool and potentially with other urine or hormone panels.
We're looking at around 150 different biomarkers—bacteria, viruses, pathogens, parasites, gut inflammation markers, intestinal bleeding markers, gallbladder issues. We can detect fat malabsorption, nutrient deficiencies, amino acid problems, brain chemistry problems. So, it's truly amazing what we've been able to do. And this is far cheaper than I've seen people go to the Amen Clinic and spend three thousand dollars on a spec scan, and they're not happy with the results. So, I'm not saying don't do it. I'm just saying I've seen it, and I like what we do better. That's what I'll say.
(Yeah), and if you want to reach out clinically, you can get help from Dr. J, that's Dr. Justin Marchegiani, at justinhealth.com. He's amazing. Or if you want to go to me, Evan evanbrand.com, we're happy to help you guys. We love what we do. We're really blessed to be able to find answers for you all because it's helped us with our own family, and we love changing lives. So, we'd be happy to help.
Dr. Justin Marchegiani: I love it, and you know, we try to give actionable, real information and try to get real data that actually changes the course of treatment. And then, you were talking about a couple of things. Maybe another good marker to look at for some of these really histamine-sensitive people would even be zonulin, right? It's a gut permeability marker because the more gut permeability you have, the more that immune system could be hyperactive.
But again, that's another marker where it's like, “Well, what do you do with that marker?” It still… You still gotta look upstream and all the things we just mentioned. So, we want to just give you guys real information that's actionable so you guys can get the data and then figure out what the next steps are to really get to the root cause of what's happening.
Evan Brand: Yeah, I mean, if you're having elevated zonulin, maybe that would make you throw in some gut support sooner, like some DGL or some zinc carnosine or something like that. Maybe you throw that in sooner. But at the end of the day, you're going to think, “Okay, well, why? What the heck?” So, now you're back to bugs again or toxins.
Dr. Justin Marchegiani: Gotta get to the root. I totally agree. Well, Evan, great podcast, man. We'll do this again real soon. We'll put links down below where you guys can reach out to us all, and then also, we have review links as well. We'd love to get some reviews here, evanbrand.com/iTunes, justinhealth.com/iTunes. Love the review. Appreciate it, you guys. And make sure you share it with family or friends. We want to be able to get the word out and put the power back in your hands to take control of your health. Thanks, guys. Thanks, Evan.
Evan Brand: Amen. Take care.
Dr. Justin Marchegiani: Peace. Bye
Headsup Health free signup: http://www.justinhealth.com/headsup