
“Does eating more protein wreck your kidneys?”
Short answer: Not in healthy people. The long answer is more interesting—and way more useful. In this guide, you’ll learn what really drives kidney stress (hint: it’s not your grass-fed steak), how insulin resistance and inflammation set the stage, which labs to run to catch problems early, and how to dial in protein for performance and longevity.

This belief mostly comes from research in people who already had kidney disease—then it got generalized to everyone. When you look specifically at healthy adults, higher protein intakes do not harm kidney function.
Bottom line: in people without kidney disease, more protein ≠ kidney damage. If kidney function is already impaired, that’s a different clinical scenario and requires individualized oversight.

Insulin acts on the kidney to increase sodium reabsorption, which can raise blood pressure and increase filtration pressure in the glomeruli (your kidney’s “filters”). Over time, that pressure plus inflammation is a recipe for damage.
Action steps
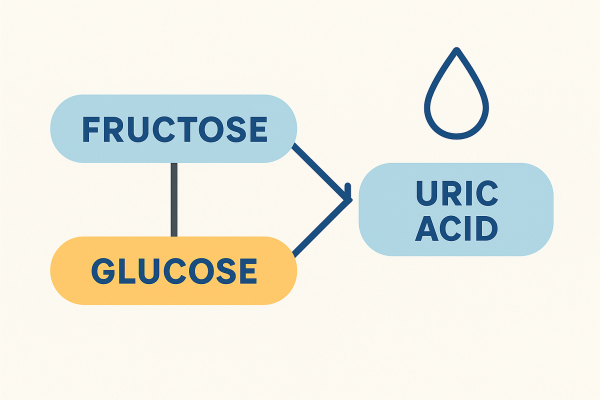
Large loads of added fructose (think high-fructose corn syrup, soda, syrups—not whole fruit) raise uric acid, which is linked to metabolic dysfunction, hypertension, and fatty liver—the same cluster that accelerates kidney disease.
Action steps
Hypertension and chronic low-grade inflammation are core risk factors for CKD progression.
Action steps
Long-term proton-pump inhibitor (PPI) use has been associated with increased CKD risk in several meta-analyses, though findings are mixed and do not prove causation. PPIs may deplete magnesium, alter the microbiome, and raise oxidative stress—all unfriendly to kidneys. Work with your clinician on step-down strategies if appropriate.
Cadmium, lead, mercury, glyphosate, and mycotoxins can create oxidative stress and tubular injury. If exposure is suspected (older housing, occupational exposure, water quality, water-damaged buildings), targeted testing and mitigation matter.
A practical range for most adults is 0.6–1.0 grams per pound of goal body weight (1.3–2.2 g/kg), adjusted for activity, age, and goals. Athletes and heavy lifters may need more; very sedentary individuals can live closer to the low end.
Quality matters. Choose grass-fed/pastured meats, wild fish, eggs, collagen/gelatin for glycine balance, and minimally processed whey or beef isolate if you use powders. Highly processed meats and burnt/charred proteins bring extra oxidative load—keep cooking gentle (slow cookers, sous-vide, light sear).

You don’t have to wait years for a diagnosis. We can spot metabolic and renal stress early and intervene.
Clinical pearl: If your creatinine bounces after a hard lift day, it may reflect muscle breakdown—schedule labs at least 48–72 hours after strenuous training.
Eat this way
Train & move
Supplement (personalized)
Medications
Does hyperfiltration mean harm?
Not necessarily. In healthy kidneys, a higher GFR after a protein-heavy meal is an adaptive response. Reviews in healthy populations show no adverse change in kidney function from higher protein intakes.
Is plant protein “safer”?
Plant-forward patterns are consistently linked to better metabolic health; one large cohort associated higher plant protein with lower CKD risk. Quality omnivorous diets also perform well when ultra-processed foods and sugars are minimized.
If I already have CKD?
Work directly with your clinician. Protein may need individualized adjustment, and electrolytes require careful monitoring. The priority shifts to controlling blood pressure, blood sugar, and inflammation, the dominant drivers of CKD progression.
Devries 2018 (Meta-analysis): High protein does not adversely affect GFR in healthy adults. PubMed. PubMed
Van Elswyk 2018 (Systematic review): Higher protein intakes show normal kidney function in healthy adults; GFR rise is adaptive. Adv Nutr. PubMed+1
Antonio 2016 (1-year trial): ~2.5–3.3 g/kg/day protein no harm to kidney/liver labs in trained men. JISSN. PubMed+1
Insulin & sodium reabsorption: Insulin directly enhances renal sodium reabsorption → higher BP. Classic + updated reviews. PubMed+1
Fructose & uric acid: Mechanistic and translational links to metabolic disease and hypertension. PubMed+1
Hypertension & CKD progression: Strongly intertwined; controlling BP is pivotal. AHA Journals
CKD risk factors (2024 update): Age, HTN, diabetes, obesity, proteinuria, dyslipidemia, environment. PMC
PPI–CKD association (mixed): Meta-analyses show associations; some datasets show no link vs H2RAs. Individualize risk/benefit. PMC+2MDPI+2
Protein in CKD (context): In mild–moderate CKD, higher protein intake associated with lower mortality (observational). JAMA Network
For healthy people, protein isn’t the villain—insulin resistance, hypertension, inflammation, toxins, and poor diet quality are. Eat real food, hit your protein target, train, sleep, and track the right labs so you can course-correct early.
Ready to personalize your plan?
👉 Schedule a complimentary consult at www.justinhealth.com/free-consult and let’s map out your optimal protein target, lab strategy, and step-by-step plan.
====================
====================
IN CASE YOU MISSED IT:
How Mold and Mycotoxins Affect Your Child's Brain Development
Protein Myths Debunked: What Really Damages Your Kidneys with Rob Edwards | Podcast #464