
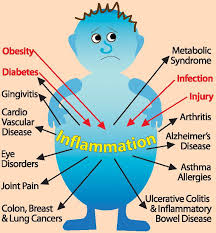
Dr. Justin Marchegiani and Evan Brand go in depth about inflammation in this podcast episode. Learn about the signs and symptoms of inflammation, the supplements you can take to alleviate conditions, and the markers you need to watch our for or test to check for inflammation.
 Also in this interview, discover how you can reduce inflammation via diet and lifestyle changes and how that affects your optimal health. Find out how to prevent inflammation and learn what the conventional treatment methods actually do for inflammation as well as the functional medicine approach that is available for you.
Also in this interview, discover how you can reduce inflammation via diet and lifestyle changes and how that affects your optimal health. Find out how to prevent inflammation and learn what the conventional treatment methods actually do for inflammation as well as the functional medicine approach that is available for you.
In this episode, topics include:
1:48 What is inflammation?
4:57 How to prevent inflammation
8:12 Inflammation markers
8:45 Conventional treatment for inflammation
19:30 Functional medicine approach
![]()
Dr. Justin Marchegiani: Evan Brand, my man! Dr. J here. What’s going on?
Evan Brand: What’s up?
Dr. Justin Marchegiani: It’s just–
Evan Brand: I’m drinking a smoothie.
Dr. Justin Marchegiani: Love it! And it’s Friday. We just had Paleo f(x) last weekend. We missed you down here in Austin.
Evan Brand: I know. I know. Well, I’m glad you had a good time. I heard you did amazing things there. So spreading the word.
Dr. Justin Marchegiani: Spreading the word. I hear you also got some amazing things coming, maybe in the next week?
Evan Brand: Yeah.
Dr. Justin Marchegiani: Want to share with the listeners?
Evan Brand: This baby’s coming soon. I don’t know when. Yeah, people who’ve been listening to my show, but the baby is doing like a week here so Hannah just had some really spicy guacamole. She thought that was gonna throw her into labor.
Dr. Justin Marchegiani: Oh, gosh! So what’s your strategy? Do you guys have a birthing plan? Are you trying to go midwife and—and do a more natural approach?
Evan Brand: Yeah, we got a midwife. We have a doula. So she’s gonna be helping us to basically prevent Hannah from requesting any interventions that may be unnecessary. So we’re doing it at a hospital that’s mainly a birthing hospital that’s focused, like the entire floor is dedicated to only moms–
Dr. Justin Marchegiani: Wow.
Evan Brand: And the recovery room—and the recovery floor is only dedicated to moms that just had babies. So that’s a huge relief for me because I hate hospitals. They freak me out and I would like to stay away from antibiotic-resistance bacterias as much as possible and hospitals are the best place to pick one of those things up. So–
Dr. Justin Marchegiani: Absolutely.
Evan Brand: So yeah, that’s—that’s what’s up with that.
Dr. Justin Marchegiani: Well, best of luck with you and Hannah next week.
Evan Brand: Thank you.
Dr. Justin Marchegiani: It’s gonna be very exciting!
Evan Brand: I know.
Dr. Justin Marchegiani: Very cool. So any other thoughts today? I mean we talked about in the pre-show that we were gonna really touch upon inflation—um, inflation—inflammation!
Evan Brand: We gated on that, too!
Dr. Justin Marchegiani: We gated on that, too. Inflammation is—is basically, inflation is inflammation of the financial industry so to speak.
Evan Brand: Yup.
Dr. Justin Marchegiani: But we’re doing it on the body today. Inflammation, which kinda to give you the whole tenet of that word. Basically your body is going into accelerated breakdown. You’re breaking down faster than your building up. Now in conventional medicine and functional medicine, we have all these different cytokines and TNF-α and interleukins and C-reactive protein, all these different markers that we can test for that tell us that we’re breaking down. But typically pain and brain fog and fatigue and digestive issues and performance issues and mood issues for the most part are always a good sign that you’re inflamed.
Evan Brand: Yeah, so I mean is it really necessary for us to test for inflammation? In my opinion it could be a good thing to check in on–
Dr. Justin Marchegiani: Mmm.
Evan Brand: Don’t you think in terms of blood? But if we just put in the foundations that we’re gonna talk about today? Then we’re gonna be working on restoring that inflammatory cascade that’s happened in the first place.
Dr. Justin Marchegiani: Yeah, it’s nice to be able to quantify because if we see CRP above 1, or fibrinogen above 300 or homocysteine above 8 or 9 or we see, let’s say increasing calprotectin or lactoferrin or various lysozymes or you know, IgA is very, very high and this is some of the gut inflammation markers. That there’s something going on in the gut, something going on in the body and it’s great to be able to provide an intervention whether it’s adrenal, diet, lifestyle, blood sugar and removing of infections and dysbiosis, and see those markers come down. It’s like you’d really know that we did something. It’s tangible.
Evan Brand: What about something simple, too? Like white blood cell count that most people are gonna get on their standard CBC from their doctor if their doctor is not running the biomarkers that actually matter. Can that be helpful, too? Because we’ll see maybe there’s some type of active infection that we’re trying to fight or something like that?
Dr. Justin Marchegiani: Yeah, so like I touched upon that briefly with the IgA which is a kind of like immune antibody that’s like in that white blood cell realm, but like total white blood cell, yeah. If we see it like below 4, that could be a sign of a chronic issue, chronic infection immune issue or if it’s above 7-1/2 or so, that could be an active infection that our body is fighting and again, typically there’s gonna be inflammation as the by-product of that.
Evan Brand: Right. Well said.
Dr. Justin Marchegiani: Cool, man. The big thing is I think off the bat we wanna do our best to reduce inflammation because that’s gonna accelerate aging, right? All these people today are spending all these money the older they get on helping to look younger, right? Well, don’t look to some kinda lotion or potion first, look to things that you can do to reduce inflammation. And that would just start with the diet first, cutting out a lot of the crappy inflammatory foods. Grains are gonna be no. 1, maybe your—your conventional diary right there with it, and then extra refine sugar or excess carbohydrates would be right there behind that as well.
Evan Brand: Yup. Yeah, so I see so many people that try to promote these multilevel marketing schemes of like anti-aging products and—and all of that, but really just reducing this whole process like you’re talking about of glycation, those AGES—
Dr. Justin Marchegiani: Yeah.
Evan Brand: That AGES–
Dr. Justin Marchegiani: Literally AGES.
Evan Brand: They advance—yeah, I mean, if we can stop that whole glycation process but cutting these sugars out then you’re gonna be doing the first step and I would assume that most people listening, they’ve already done the—the diet piece. So you’re all here today for the really geeky stuff that we’ll get into in terms of the next steps.
Dr. Justin Marchegiani: Yes.
Evan Brand: What do you after the diet’s in place? How do you prevent inflammation? Do you think we should touch on adrenals and—and the whole cortisol-cortisone balance, is that worthy for this conversation or shall we go into like the herbs and stuff?
Dr. Justin Marchegiani: I think that’s good. We can just—we can go into some of the adrenal and testing stuff, and I spoke on this on a panel at Paleo f(x) just last weekend with Jack Wolfson. He’s a Paleo cardiologist. Also Nora—help me with her last name—Nora?
Evan Brand: Ged—Gedgaudas.
Dr. Justin Marchegiani: Gedgaudas. Nora Gedgaudas. And then also Lane Sebring, and one more person on the panel as well.
Evan Brand: Oh, man! I bet that was a blast!
Dr. Justin Marchegiani: Yeah, it was really, really good panel. I mean, you know, lots of good talks about inflammation and all the other things that would go along with it, but the first thing is make sure the diet’s in place, right? The diet’s gotta be in place. We checked that off our list. Okay, good. Anti-inflammatory, nutrient-dense, low toxin diet. Got it. Boom!
Evan Brand: Yup.
Dr. Justin Marchegiani: Alright. It’s not too sexy but the diet’s the most important. Good. We got the sleep dialed in. We’re able to heal. We’re able to help restore our body. Alright, we got that piece dialed in. Well, the next is, we have to make sure we’re not throwing toxins into our body. Things that can drive inflammation, toxins whether it’s MSG or various chemicals from just being around toxins which—or you know, poor, you know, water that’s not filtered. Those are all toxins. So we kinda mitigate the toxins coming in. That’s number 1. Number 2, make sure we can break down our foods. If we can’t break down our foods, even healthy foods can have negative effects. Had a lot of patients this week that are—have chronic GI issues and they’re very sensitive to even what we can consider like healthy foods.
Evan Brand: Yup,
Dr. Justin Marchegiani: And they are reacting to it and they shouldn’t be. So we have to make sure we reduce the inflammation with them and be able to make sure they can digest their foods.
Evan Brand: So let me–
Dr. Justin Marchegiani: So be—yeah?
Evan Brand: Let—let me ask you about that.
Dr. Justin Marchegiani: What?
Evan Brand: So our, you know, we’re not talking just infections for these patients. You know, we’re talking about people that just have maybe some malabsorption issues but they don’t have infections. Maybe they just have some gut dysbiosis, right? So if someone gets the all-clear, maybe they don’t have parasites, that doesn’t mean that your gut’s working perfectly. There’s still a lot of other things that we can work on, right?
Dr. Justin Marchegiani: Yeah, if we have like a small intestinal bacterial overgrowth or a dysbiosis, that’s gonna set us up to have an inability to break down food optimally because our hydrochloric acid and enzyme levels will be less, so we gotta make sure that that’s good because if not, that good healthy diet may not be getting into our bloodstream and—and going where it needs to go.
Evan Brand: Right, that makes sense.
Dr. Justin Marchegiani: And that’s important. We gotta be able to break—even healthy foods can have a negative reaction, especially if your gut’s leaky. It’s just a matter of time if you have that routine food that you have every day that you’ll develop a food allergy response to it.
Evan Brand: I’ve got an allergy to walnuts apparently right now. So I’m cut—I had to cut them out and I had some the other day and I had a horrible headache afterwards.
Dr. Justin Marchegiani: Ooh.
Evan Brand: So I was like, “Wow!”
Dr. Justin Marchegiani: Yeah, and it would be from, you know, we’re knocking out some infections with you, you know, I think—what is it? The Three Amigos—Giardia, Crypto, H. pylori.
Evan Brand: I didn’t have H. pylori–
Dr. Justin Marchegiani: Okay.
Evan Brand: Thank goodness.
Dr. Justin Marchegiani: Giardia.
Evan Brand: Just the Crypto-Giardia, which I’m–
Dr. Justin Marchegiani: Double trouble.
Evan Brand: I’m at least 45 days in, so I’m gonna go ahead and run that GI map like we talked about soon and see if it’s—see if I’m free and clear now. I think I may wait another few weeks because I still have some cold hands going on.
Dr. Justin Marchegiani: We’re also gonna do the 401H, too, right? Because–
Evan Brand: Yeah.
Dr. Justin Marchegiani: That’s what picked it up, so we gotta make sure we compare apples to apples.
Evan Brand: Yeah.
Dr. Justin Marchegiani: That’s good. That’s good. So we got the diet piece because we have like gut stuff going on, that’s gonna make it really hard for us to function optimally. Plus I talked about some of those markers we looked at to detect gut inflammation, right? We looked at lysozyme, that’s a marker, an enzyme marker—that if it’s high, it can be a sign of inflammation. We talked about lactoferrin which can go up if inflammation’s present. Also calprotectin can also go up. We can also see very, very high IgA levels or white blood cell levels, and that’s a sign that our—our immune system is fighting something and then you know, all these inflammatory cytokines, right? That I mentioned are like the by-products, you know, the collateral damage from the war going on inside of our body.
Evan Brand: Yeah. Can we spend a couple of minutes talking about the conventional model because we also go–
Dr. Justin Marchegiani: Oh yeah.
Evan Brand: Into the functional model, like we hope that everyone’s going this way, but there is still the conventional model for inflammation and so typically that’s gonna be NSAIDs and I just did my latest video on YouTube the Why Supplements Can Make You Feel Worse video. I talked about NSAIDs and the number is over 10,000 people per year that are dying of regular use of NSAIDs that they’re taking probably that were prescribed from whoever, doctor or physical therapist or whatever, for the inflammation or the pain or the other symptoms they’re having. These people are dying by regular dosage of this stuff. So to me, that’s—that’s the big takeaway from today’s talk together is you know, just encouraging people, “Look, there are other options.” I remember I talked with you one day when I—I don’t know if I had a bad headache or what was going on, maybe headache, anxiety or something back when I was in Texas, and you were like, “Dude, no, the hospital’s not gonna help you. We need to just get some magnesium going.” And so even something like that, maybe that’s not considered anti-inflammatory for that case, but for an example of a headache, someone’d typically gonna go think inflammation. They’re gonna go Advil, Tylenol, ibuprofen, Excedrin, whatever. No, you may be able to do magnesium, maybe some of the turmeric or fish oil, stuff like that.
Dr. Justin Marchegiani: Yeah, yeah. So off the bat, when we look at some of the conventional approaches, the over-the-counter kinda go into 2 phases. You have like the NSAIDs which are like ibuprofen or—or aspirin, those kinda things. And then you have the acetaminophens which are like the Tylenol kind of things.
Evan Brand: Yeah.
Dr. Justin Marchegiani: So acetaminophen goes more to the liver. NSAID goes more to the gut. So NSAIDs can create more gut ulceration issues. The acetaminophen can go more to the liver. So those are kind of the two different angles for the over-the-counters and then you have the more deeper stuff, like the opioids stuff which are gonna be like the OxyContin, Codeine, Percocet, Vicodin, and there’s some that are combined, you know, Percocet’s combined, then you have something like a Midol, which are like caffeine and ibuprofen stuff. Again I just stick to the active ingredients, right? Because there’s like a hundred different—there’s like 20 NSAIDs out there. There’s like 20–
Evan Brand: Right.
Dr. Justin Marchegiani: Acetaminophens. All these different names. So you have your NSAIDs. You have your acetaminophens, and then you have your various opioids to keep it–
Evan Brand: Yeah.
Dr. Justin Marchegiani: Keep it simple.
Evan Brand: And then we see—just today they finally admitted that Prince died of opioids.
Dr. Justin Marchegiani: Yeah.
Evan Brand: So–
Dr. Justin Marchegiani: What was the—
Evan Brand: There you go.
Dr. Justin Marchegiani: I think it was a Fentanyl overdose, wasn’t it?
Evan Brand: Yeah, Fentanyl.
Dr. Justin Marchegiani: Yeah, I mean that’s like—that’s like an anesthetic, I know. So it’s crazy, so all these things, all thy do is block various enzymes to experience pain. So like NSAIDs, they’re gonna—like they’re non-steroidal so they’re gonna help block these—these various cyclooxygenase enzymes–
Evan Brand: So–
Dr. Justin Marchegiani: COX enzymes for short.
Evan Brand: So it’s not actually resolving the issue, it’s just–
Dr. Justin Marchegiani: No.
Evan Brand: Basically changing the way that the body sends the signal to the brain. Is that right?
Dr. Justin Marchegiani: Yeah, so when you have inflammation, your body’s gonna short out a whole bunch of prostaglandins—prostaglandin E2 to be specific and that’s gonna cause that pain sensation and then essentially all you’re doing with an NSAID is your trying to block or inhibit those prostaglandins from being formed. The problem is the upstream action of those prostaglandins being made, that mechanism that’s stimulating those prostaglandins is still happening. You’re just decreasing the prostaglandins actually being synthesized. So in the endi, the mechanism is still there, right?
Evan Brand: Yup.
Dr. Justin Marchegiani: And then the other part is the corticosteroids. Those are like prednisone or like hydrocortisone, right? These are the actual steroids. So you have the non-steroidals, the NSAIDs, right? Then you have the acetaminophen which is like your—your Tylenol, right? And then you have some of the corticosteroids which are like prednisone or cortisone or Cortef, right? These are things that we do to help add extra ability for our hormones to be able to dissolve the inflammation. Now again this is why having healthy adrenal glands is so important because healthy adrenal glands help put out the fire of inflammation, right? Imagine your adrenals is like the fire extinguisher and imagine the fire is like the inflammation in the br—in the body. Now ideally, we don’t wanna be pyromaniacs setting fires in our house every day. But let’s say a little fire happens because of some stress in our lives. We wanna make sure the firefighters can show up and their hoses are full of water so they can douse it out. So imagine the firefighter coming up with empty hoses, that’s like having very weak adrenals. We have a very low amount of stress can essentially burn down our house, so we wanna make sure that we’re not letting fires in our house. Number one, that’s reducing inflammation activities and then number two, we wanna make sure out fire hoses, our adrenals are strong so if fires happen, we can put them out pretty fast.
Evan Brand: Yeah, and you and I do look at some adrenal testing–
Dr. Justin Marchegiani: Yeah.
Evan Brand: That will show the cortisol-cortisone balance. So if you’re listening and you want the general takeaway for that, basically if you’re running from a bear or so your nervous system thinks, you’re gonna be more shifted into that cortisol state and you’re not gonna be shifted towards cortisone. So it’s like you don’t even have the ability to respond to the inflammation, right? It’s kinda like maybe the firemen just took the day off because there’s–
Dr. Justin Marchegiani: Yeah.
Evan Brand: There’s nothing there.
Dr. Justin Marchegiani: Yeah, cortisone’s a little bit more downregulated. It’s a metabolite of cortisol. Cortisol’s more active and then cortisone’s kind of downstream a bit. So we wanna make sure we have the ability to regulate inflammation. So we have it internally by our adrenal glands. We have it diet and lifestyle-wise by not putting crappy foods in and by sleeping and doing the right kinds of exercise and taking time off to meditate or do healthy forms of exercise right? And then we have the ability to look in deeper to chronic infections that could be driving issues. I tell my patients, you could be inflamed. If you’re on a beach relaxing and chilling out and meditating, eating perfect food, but if you have an internal infection, like—like you did with your—your double trouble, your Blasto and Crypto, you may still have symptoms. So we wanna make sure–
Evan Brand: Crypto-Giardia.
Dr. Justin Marchegiani: Crypto-Giardia, yeah.
Evan Brand: Yeah.
Dr. Justin Marchegiani: So we wanna make sure that we have internal inspections, the hidden inflammation under control.
Evan Brand: Yeah, and—and that’s a great point you make sure, so I’m gonna restate it, is if everything seems to be making sense in terms of your—your diet, your lifestyle, like all of that makes sense, you have all that done. You’ve read all the books.
Dr. Justin Marchegiani: Yeah.
Evan Brand: You’ve tried all the diets—98% of people that work with us, they’re struggling. And people we’ve blown away, people that are coming to us in terms of like they’re status where you would think this person has it all figured out because of who they are, but they’re still suffering.
Dr. Justin Marchegiani: Yeah.
Evan Brand: And a lot times we look deeper and it’s like, “Bingo!” There it is! It’s—isn’t it kinda fun? I mean, it’s not that we wish stuff upon people, but when you finally have an answer for someone’s health problems they’ve been suffering for 20-25 years and then you finally find something in the gut, it’s like, “Oh, thank God! We found something!”
Dr. Justin Marchegiani: Exactly. Well, you just gotta know physiology and you gotta know the—the weak links in—in the average person’s physiological chain and the gut and the adrenals and diet and inflammation is definitely one of those common links that breaks in everyone’s chain that, you know, will manifest in different diseases, right? But it’s the same physiology that—that’s breaking though.
Evan Brand: Right, so basically you’re saying it doesn’t really matter if your symptom sounds like it’s over here in the left field with this net that we’re casting. That’s basically gonna be a broad enough but also specific enough net to just identify the body system that is dysfunctioning.
Dr. Justin Marchegiani: Yeah.
Evan Brand: And it doesn’t matter if—if someone else doesn’t have the exact manifestation as you, it’s the same mechanism you’re saying.
Dr. Justin Marchegiani: Yeah, same mechanism. I mean, look at it. Any type of autoimmune condition or massive pain issue, right? What does conventional medicine do? We’re gonna throw a prednisone at it, right? For the most part or corticosteroid.
Evan Brand: What do they wanna do with that? What—what is their actual long-term goal with that? I mean, it just seems very unsustainable.
Dr. Justin Marchegiani: Well, my analogy is this. There’s a pyromaniac in the house that’s lighting fires every single day but we’re not gonna go in and get the pyromaniac out of the house, we’re just gonna continue to douse the house on with water as—as new fires creep up every day.
Evan Brand: Yeah.
Dr. Justin Marchegiani: So Chris Kresser gave an analogy at Paleo f(x), he’s like yeah, you walk around and you got a rock in your shoe and then you start feeling a lot of pain and you start getting a blister and you’re like, “Shoot, I’m just gonna reach for an NSAID or an ibuprofen or a corticosteroid to numb that pain.” But we know the root cause is just take the shoe off and kick the rock out.
Evan Brand: Uh-hmm.
Dr. Justin Marchegiani: Right? So I think it’s important because we have to have like a really good sound philosophy of why we’re doing what we’re doing. Because now the next step is, alright we have natural anti-inflammatory things that we can do as well as on the functional medicine/natural medicine side which are great but we can use these things just like drugs in the sense that we can just use them to cover up symptoms. So again, we always wanna get to the root cause. Dr. George J. Goodheart—get to the highest, you know, get—the highest good is to always get to the root cause. Alright, so always getting to the root cause is gonna be very, very important. Now the reason why even if you forgot getting to the root cause, let’s say you had a little brain fart and you just kinda miss that part, well, at least we’re taking substances that don’t kill 20,000 people a year taken properly.
Evan Brand: Yeah.
Dr. Justin Marchegiani: Some of these pain meds can kill a lot of people, and if you go back 10 years ago to Vioxx, that killed 80,000 people.
Evan Brand: Gosh.
Dr. Justin Marchegiani: These are—these could be some dangerous medications, so yeah, there are a lot of people out there that say, you know, don’t practice natural medicine like an allopath. I get that. I respect it. I’m 100% in agreement, but I rather see someone do that than take a lot of these pain meds chronically and—and die from it.
Evan Brand: Agreed, yeah. And I actually have a few females that I was talking with this week specifically that they’ve been on OxyContin for 10 years.
Dr. Justin Marchegiani: Oh, my God! That’s insane.
Evan Brand: So, you know, in their 60s just trying to come off of this stuff, it’s im—it’s almost impossible. It’s–
Dr. Justin Marchegiani: Yeah.
Evan Brand: Very troubling.
Dr. Justin Marchegiani: And some people they have such a wind up of inflammation that it’s really hard to come off so they have to kind of start making a lot of the diet and lifestyle changes, bring some of the natural stuff in at very high doses and then slowly taper off over time. And then you know, if you’re gonna be on it, too, we can at least do some damage control and add in some milk thistle or Silymarin or liver support to help support the liver if we’re doing high doses of acetaminophen or these things over long periods of time.
Evan Brand: Yeah, that was something I was gonna talk with you about, too, which maybe this is a tangent, maybe not, is when I looked at her organic acids test specifically with the—with all the pain meds in the system, all of the detox measures there on the organics that they were all flagged really high–
Dr. Justin Marchegiani: Big time.
Evan Brand: And what else was on there? There was a couple other liver markers, too, that were just off the charts. So anyway long story short, I don’t—I couldn’t find it specifically but it was crazy to see because you read about how these medications affect the liver, but when you actually see it on a piece of paper and you’re seeing like whoa! This is associated with liver issue, it’s like, “Wow! This is amazing to see.”
Dr. Justin Marchegiani: Yeah.
Evan Brand: This is affecting you—it’s not just something you read on the Internet. Look, there it is in the flesh. It’s–
Dr. Justin Marchegiani: There it is, 100%. I—
Evan Brand: That’s was crazy.
Dr. Justin Marchegiani: I think that’s great. So like with our a functional medicine, non-dogmatic philosophy, right? Alright, I’m gonna go—let’s pretend like there’s been a time in the last year where I maybe drank some alcohol that wasn’t the best, and it maybe gave me a headache the next day. Alright, so what do I do? I wake up. I have a little bit of a headache. Well, I take some magnesium. I rehydrate with a whole bunch of minerals. I eat a good breakfast. I stabilize my blood sugar. My head’s still pounding, well, I may take an ibuprofen, right? That may happen like once a year max. So that’s kinda like triage, right? You’re in the moment. You do a couple of natural things. Your head’s pounding. It’s like, “What the hell?” If I take this ibuprofen, it’ll be gone in a few minutes. Fine, that makes sense. What’s the underlying cause? Well, the underlying cause is not something perpetual in motion. It’s not a chronic issue. It’s an acute thing that happened. You did your best, the triage, a couple of things, it didn’t work. You want relief now. Fine. Not that big of a deal. Alright?
Evan Brand: Yeah.
Dr. Justin Marchegiani: Now, in the end, what did I learn from that? Well, if I drink some questionable alcohol, I’ll bring some charcoal. I’ll bring some extra vitamin C or N-acetyl cysteine or some—some milk thistle, some liver support. Boom! Then we can get—get ahead of that. Sometimes we don’t get ahead of it, and then we’re triaging it, and then that’s where maybe conventional medicine can be great. Also we can pull in there, sometimes Iike I find NSAIDs do work great for headaches, but if we can’t we’ll throw in some boswellia, or we’ll throw in some turmeric or curcumin. We’ll throw in some high dose enzymes on an empty stomach. We’ll throw in the enzymes, probio—let’s see–
Evan Brand: I like Arnica.
Dr. Justin Marchegiani: Oh, Arnica! Some homeopathic can be phenomenal. Homeopathic can be great. White willow bark which is where acetaminophen is extracted from, Devil’s claw, DLPA which is a type of phenylalanine amino acid that has the D and L form. So you have those off the bat. You have the enzymes. You have some turmeric. You have boswellia. You have the—you can even do ginger. You have devil’s claw. You have while willow bark. All those things are great. And I actually just came out with a new curcumin—it’s called Curcumin Supreme. That’s a liposomal curcumin with MCT and sunflower lecithin. Again there’s one in the market right now called Meriva, which is good. It’s a very good one but it’s got phosphatidylcholine from soy, so it’s a liposome, but this one doesn’t have the soy so it’s more sensitive for my autoimmune patients. So I was really happy to be able to formulate that.
Evan Brand: Good job. Yeah, I thought of something else. Oh, I like how you’re getting fancy with the DLPA there coming in with the amino acid route. That’s something I’ve used really successfully, too, for people with chronic pain and they just—they wanna give up and the aminos can be awesome. So I know you’ve got a video. I’ve got a video on aminos. I don’t know if I talked about DLPA. Did you in your video?
Dr. Justin Marchegiani: Maybe. I mean DLPA is a precursor to endorphin, so endorphin takes about 19 amino acids to make and it’s your natural kind of opioids so to speak, helps block pain. It’s a natural antidepressant. And if you have chronic gut issues and low protein absorption then you have a lot of inflammation getting the DLPA at higher levels can really help with the beta endorphin and helping to recharge that.
Evan Brand: So let me ask this. Can we—can we assume and say that if there are some adrenal issues going on, that we may not—it’s kinda like the power plant analogy where everything may be diverted over to cortisol so that we’re gonna have less ability to make optimal amounts of adrenaline-noradrenaline to deal with the pain as well? So it’s like we have an issue with inflammation but do we have an issue with pain as well because we can’t make as many endorphins in adrenal fatigue situations?
Dr. Justin Marchegiani: Yeah, it’s very possible. I mean, we’ll see that on organic acids test. We’ll see very low vanilmandelate levels.
Evan Brand: Uh-hmm.
Dr. Justin Marchegiani: Or we’ll even see very low homovanillate levels which are dopamine and the noradrenaline-adrenaline markers. We’ll see those very depleted.
Evan Brand: Yeah.
Dr. Justin Marchegiani: Because the adrenals are whipping, you know, they’re getting whipped into—into effect to produce more of these anti-inflammatory compounds. But also that, we also tend to see more depleted sex hormones. So our dehydroepiandrosterone pathways, DHEA for short, or andro or testosterone, those pathways start getting robbed and we’re making more stress hormones because the body is hardwired to deal with the inflammation now versus the stress and healing of tomorrow, right? So the analogy is you got some firefighters and you got some carpenters sitting out in front of the house. The house is on fire. Who goes in first?
Evan Brand: Say that again.
Dr. Justin Marchegiani: You got a house that’s sitting on fire, right?
Evan Brand: Uh-hmm.
Dr. Justin Marchegiani: Out in front of the house, there is a carpenter and then the other guy is a firefighter. Who goes in first?
Evan Brand: Hopefully the firefighter.
Dr. Justin Marchegiani: Firefighter, right? That’s our body. It’s just hardwired just like that, right? We wanna deal with the inflammation and stress first, and then repair and heal afterwards. So the firefighter is equivalent to cortisol and our stress hormones. The carpenter is equivalent to DHEA and our sex hormones. So the problem is most people they live with a house on fire.
Evan Brand: Right.
Dr. Justin Marchegiani: So the carpenter just sits on the sidewalk, you know, twiddling his thumbs while the fire—firemen’s in there, just continuing to try to douse the house with a hose that’s running on dry.
Evan Brand: Yup, yup. So basically, we’ve—I felt like we’ve done a good job of zooming in and zooming out. It’s not just one thing. Its—
Dr. Justin Marchegiani: Yeah.
Evan Brand: It—it’s all of this. It’s the hormones. It’s the DHEA. It’s the cortisol. It’s the cortisone.
Dr. Justin Marchegiani: Yeah.
Evan Brand: It’s the leaky gut situation. It’s use of the NSAIDs. I mean, it’s—I think people are—when they hear inflammation, they want one quick fix, but–
Dr. Justin Marchegiani: Yeah.
Evan Brand: There’s not.
Dr. Justin Marchegiani: Yeah.
Evan Brand: We have to get all these systems intact.
Dr. Justin Marchegiani: Yeah, so let’s kind of draw out our action tree. Alright, number one. Whatever your health issue is, let’s make sure we have the root cause of it addressed, right? If it’s a chronic health issue, right? We wanna do the functional medicine work to dig deeper—adrenals, guts, infections, malabsorption, nutrients—that’s the deeper work because we don’t know the root cause is. We know what the root cause is now, right? It’s we had a little bit too much alcohol last night, right? Well, number one, we can go grab the natural anti-inflammatories first, do all the diet and lifestyle stuff. Does it work acutely enough to triage it? Yes? Okay, we’re good. If it doesn’t, we may grab an NSAID. We may grab an NSAID, we may grab a—acetaminophen or Tylenol. Alright, that’s kinda option number two. And then number three, we always wanna have the prevention mindset. If we know that we’re gonna be in a place that we may encounter some certain things, take some extra enzymes, maybe drink some ginger tea, take some charcoal with you, take some NAC, take some extra vitamin C to support your body ahead of time so can kinda prevent it, right? An ounce of prevention is worth a pound of cure, so to speak.
Evan Brand: Yup.
Dr. Justin Marchegiani: So number one, do we have the underlying cause addressed? Number two, is it chronic? And if it’s chronic, you gotta go the functional medicine route. Number three, if it’s chronic let’s try to whittle down some of the natural—let’s try to whittle down the pharmaceuticals with some natural anti-inflammatories. Just do it supervised, so we’re not doing anything rash. And then number three, let’s get to the root cause of why you’re inflamed?
Evan Brand: Yup, great summary there. Yeah, and like I said, we’re assuming everyone has the—the diet piece in there, so if you’re still—let’s say like for my grandpa, I swear this guy I cannot get him off Jif peanut butter with the hydrogenated oils which is inflammation. So you know, we go out to the restaurants, we get exposed those soy bean and other inflammatory oils. So keep that on your radar, too. It’s not just the things you see. If you go get your good steak—your good grass-fed steak somewhere, well, figuring out what they cook that in, too. It’s not that you have to be neurotic about it, but just figuring out—am I getting exposed to inflammatory oils there? It may not be something that’s gonna make or break you, but if you’re trying to be that top 1% of health, like we are and how we want our patients to be, you may have to have that level of microscope put on, you know, those little factors. But I have been trying to get him to like even an organic peanut butter.
Dr. Justin Marchegiani: Better.
Evan Brand: Not—not even off, I mean, I’m trying to even just get him off peanut butter completely.
Dr. Justin Marchegiani: Right.
Evan Brand: And over to almonds or something, but even just getting him off the hydrogenated oils, it is insanely hard. He reads all the books. He reads all the articles I send him. He listens to the podcast. He won’t do it. Grandpa, stop eating Jif peanut butter.
Dr. Justin Marchegiani: I know, I hear you, man. You just gotta grab the low hanging fruit. You only can—you can lead the horse to water but you can’t make it drink, right?
Evan Brand: That’s true.
Dr. Justin Marchegiani: Cool. Well, I just think the big take home is through is if you—you got some pain and inflammation and you’ve done all the things we’ve talked about. Don’t suffer for another day or two if it’s—if it’s something that can go away with one ibuprofen, I don’t think it’s worth suffering. I mean, do your best to—to maximize all of our options, but then if you have to use a—a pharmaceutical acutely like that, well, what the heck? I mean, if it gets you the quality of life back right away and you’re not suffering, I think that’s okay.
Evan Brand: Yeah, I think I’m a little bit more likely to suffer like 48-72 hours and then I’ll resort to it. Like I had some weird like tension headache. We had a bunch of weird storms rolling and my head was just pounding. I just tried to up the vitamin C and magnesium, wait for the storm to pass and then my head got better. So it’s crazy all the environmental influence is they happen on these—on these pain signals, too.
Dr. Justin Marchegiani: Yeah.
Evan Brand: You notice that? Like when the weather’s different, your joints are like, “Ugh!”
Dr. Justin Marchegiani: Oh, yeah, I agree. Yup, they—the nitrogen in the joints I think it—I think when the pressure goes down, the joint pressure goes up. So yeah, that can happen. You can have a lot of that joint pain because of it.
Evan Brand: Yup.
Dr. Justin Marchegiani: I know.
Evan Brand: I know you see that probably a lot when you were doing a lot more hands-on work. You know, you’re hands-on functional applied kinesiology, all of that stuff, that you would see people with pain issues more when the weather was bad.
Dr. Justin Marchegiani: Oh, and I can’t tell you how many people that have chronic back pain and neck pain and my God, they all had terrible diets, and getting the diet dialed in was huge because they just—you know, their fire hoses were dry. They were on empty and they couldn’t put out the fire.
Evan Brand: Yup.
Dr. Justin Marchegiani: So I think it’s important and also building blocks, like you’re getting extra amino acids in there, like collage or a really good clean protein powder I think could be helpful because if people’s guts are screwed up, they can absorb nutrients, so getting some good clean collagen and aminos in there can be very helpful just to provide some easy to absorb building blocks.
Evan Brand: Right.
Dr. Justin Marchegiani: Yeah.
Evan Brand: It’s a great point.
Dr. Justin Marchegiani: And if you wanna touch upon the REM Rehab stuff, I know your book, we’ll give it a little plug—this is the second time today I—I’ve talked about your book.
Evan Brand: Oh, wow. Thank you.
Dr. Justin Marchegiani: I interviewed—I interviewed Kevin Geary this morning here and he plugged it because he was your co-author, which is great.
Evan Brand: Yup.
Dr. Justin Marchegiani: And REM Rehab, all about sleep, getting into the deeper phases of sleep where you heal and reduce inflammation. Did you wanna touch upon that?
Evan Brand: Yeah, I suffered from sleep issues a lot, insomnia and other sleep issues when I was in college working at UPS midnight shift to like 5am, just–
Dr. Justin Marchegiani: Wow.
Evan Brand: Just unbelievable destruction to my hormones. Everything started there. If I were to pick a turning point in my life, that was it. And I wouldn’t be doing this today if I didn’t do that though, and so I wrote that book as a recovery guide—if I wrote that book to myself essentially, and then I talked about some of the diet tweaks that I’ve used and researched, you know, getting in your sulfur amino acids and things like that from your cruciferous vegetables and trying to support your natural GABA production. You know, I kinda hit it on like the neurotransmitter route and then gave some good like basic protocols and things for sleep if it’s—if it’s an issue. Now if I were to re-write that, I would talk more about the gut because I’m finding that regardless of what you’re doing for aminos, it can be a good quick fix and I’m not gonna even plug the name of the supplement but a lot of people are taking this supplement that I don’t really approve of because it’s a proprietary blend and you have–
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: No idea how much melatonin and other stuff’s in there.
Dr. Justin Marchegiani: Oh, I know what it is.
Evan Brand: Yeah, and so I don’t—I don’t recommend that and that—that may be a quick fix for people, but you have to look for gut infections because I was waking up in the middle of the night and I had infections. And when the infections—I—I’m assuming I’m at least 90% better because I’m sleeping so much deeper now. And I wouldn’t have done that with just that—that little magic—magic powder.
Dr. Justin Marchegiani: Yeah, I know I hear you. By the way, I found out—I talked to that person over the weekend who’s—who’s–
Evan Brand: Oh, yeah?
Dr. Justin Marchegiani: Unmentionable product will—will stay unknown. It’s 300mcg of melatonin in that product. So that’s actually pretty good. It’s a good dose–
Evan Brand: Okay.
Dr. Justin Marchegiani: About 1/3 of a milligram.
Evan Brand: Okay, good.
Dr. Justin Marchegiani: Yeah, just so you know. Maybe–
Evan Brand: Alright, I—I’ll change my mind then.
Dr. Justin Marchegiani: Yeah, I’m gonna be having this person on the show sometime soon so it’ll all be more clear then. But one last thing, probiotics can actually help reduce inflammation. I saw a study where it helped reduce cortisol. So I really added in, you know, the 5R program we talked about, right? Removing bad foods, replacing–
Evan Brand: Yeah.
Dr. Justin Marchegiani: Enzymes, acid; repairing the adrenals and gut; removing infections; reinoculation. That third R, that repair R, we’re starting to add in people that have a lot of gut symptoms. We’ll add in the extra specific kinds of probiotics to actually reduce inflammation and it has worked very well.
Evan Brand: Absolutely. It’s a great—a great finisher supplement.
Dr. Justin Marchegiani: People never think about probiotics as being anti-inflammatory.
Evan Brand: That I mean, and that’s when you and I were looking at supplement options for me. That was something, you’re like, “Dude, you have to have the probiotic at night.” Not even necessarily for the reinoculation phase, just the inflammation that’s going on with these parasites. That’s doing some damage and we need to try to reverse it. So that’ s been a really good addition for me and I did wake up, maybe a month ago when I had first started and I had some weird gut stuff going on and what I do, I woke up and I was like, “Oh, I need to take a probiotic,” and I took it and you can literally feel the inflammation in the gut cooling down almost instantly.
Dr. Justin Marchegiani: Isn’t that great?
Evan Brand: Maybe I—maybe I placeboed myself a little bit but it—it still worked. And I know it did.
Dr. Justin Marchegiani: Yeah, oh the thing is, right? You can’t placebo yourself to 20,000 deaths a year from ibuprofen, right?
Evan Brand: I know.
Dr. Justin Marchegiani: So there’s something to what’s happening on the conventional side and there’s something, too, what’s happening on the natural side and then the—the great thing about it is less deleterious side effects that’s for sure.
Evan Brand: Yeah, amen.
Dr. Justin Marchegiani: Well, Evan, I’m gonna give you the final word. Anything else?
Evan Brand: No, that’s it. I think that this was a good overview. If people liked the show, please review it.
Dr. Justin Marchegiani: Review it.
Evan Brand: It’s very helpful. I know we have listeners around the world. It means a lot. I know every time you get the little notification on your phone for apps, please review this app, you hit, “No, Thanks!” Well, don’t hit “No, Thanks!” for us. Review the show, it’s easy, it takes 2 minutes. Go to iTunes on your phone, on your computer, and write that review. It means a lot and it helps us makes sure that we’re not talking to a wall and that you’re getting great feedback and you’re learning the application steps and that we’re helping you to get to the root of any symptoms and your health goals, and just helping you do the things that you—you wanna do in life with the vibrance that everyone needs.
Dr. Justin Marchegiani: No fluff. No BS. And in my opinion, there’s no podcast like it. So give us some feedback so we can continue to do better for everyone.
Evan Brand: Yup.
Dr. Justin Marchegiani: Evan, have a great weekend, man! It’s beautiful here in Austin. Enjoy, Louisville!
Evan Brand: You, too. Take care.
Dr. Justin Marchegiani: And your new baby!
Evan Brand: Yeah, thank you.
Dr. Justin Marchegiani: Take care.
Evan Brand: Bye.
Dr. Justin Marchegiani: Bye.