

By Dr. Justin Marchegiani
Hypothyroidism symptoms can sometimes include low stomach acid and poor digestion. Poor digestion is a major problem today. As nearly 44% of the population experience heart burn monthly and 20% of them experience it weekly. Heart burn is a paradoxical symptom caused by low stomach acid strangely enough, as you would think the problem based on its name, is caused by too much acid. What essentially is happening is the food isn't fully broken down. So it begins to rot (putrefy and ferment) in the stomach and organic acids from the decaying food rise up and burn the unprotected tissue of the esophagus.
The top 2 medications sold in 2014 were a thyroid medication called Synthroid and an acid-blocking medication called Nexium. This doesn't prove that one causes the other, but in my clinical experience, there almost always tends to be a link with poor digestion, low stomach acid, and chronic infection when it comes to hypothyroidism or Hashimoto's.
Low stomach acid is commonly associated with hypothyroidism and or Hashimoto's. Stomach acid or hydrochloric acid (HCL) has a few different roles in the body, one being the first domino of the digestive process. HCL does this by lowering the pH in the stomach. This activates the digestive enzyme pepsin, which breaks down protein. The acidity produced from the stomach acid stimulates the gallbladder to produce bile salts, which are important for fatty acid break down.
If you have chronic digestive or thyroid issues and are looking for answers, click here!
When we look at the common nutritional deficiencies associated with low stomach acid, iron and B12 deficiencies commonly show up. These types of deficiencies are also known as anemias. B12 deficiency is known as a macrocytic anemia because our red blood cells can’t mature properly and are stuck in a larger state. Red blood cells actually get smaller as they mature, so the immature ones stay bigger, hence the prefix “macro.”
Cool fact: The parietal cells in the stomach, which produce intrinsic factor (IF), are the same cells that produce hydrochloric acid (HCL). This is why the HCL and B12 connection is so common. When the parietal cells are injured, it makes sense that everything it produces will no longer be at optimal capacity.
When we are dealing with iron deficiency anemias, these are commonly known as microcytic anemias. Iron is needed to help carry oxygen to the cells in our body. Our thyroid gland needs iron to help make thyroid hormone. And our cells need iron so they can take up oxygen as well. When our red blood cells don’t get enough iron, they become very small, hence the prefix “micro.”
When there is an absence of HCL in our stomach, our food tends to not digest properly. When our food sits in our stomach, it tends to essentially rot. And then various organic acids rise off of it. The maldigestion of these food sources feed various bad bacteria in our gut, and gas is produced as a by-product. The next time you feel gassy after eating, you will at least know what’s happening on the inside.
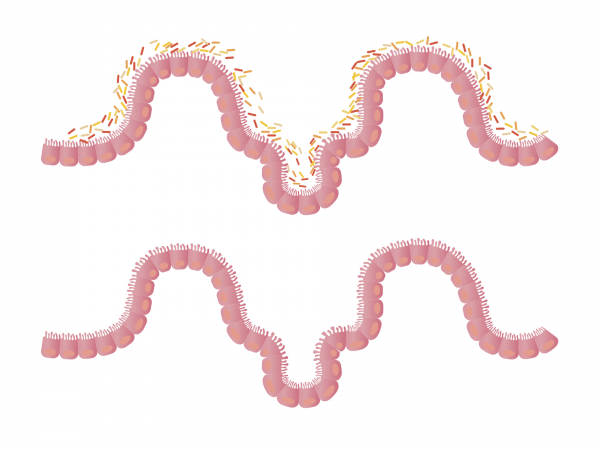
The low amount of HCL and the increase in intra-abdominal pressure cause our esophageal sphincter to stay open. The acids from the rotting food now have the ability to rise up and touch the area of the esophagus that is typically walled off during healthy digestion. This is now the beginning of gastroesophageal reflux disease (GERD). If this area continues to get irritated, over time ulcers will begin to occur along with atrophic gastritis. It is nothing more than irritation of the stomach followed by a thinning of the stomach lining.
Thyroid hormone has an effect on cellular metabolism throughout the entire body, including the gastrointestinal tract. Metabolism in the gastrointestinal tract has an effect on gastric motility. A slower thyroid can cause slower transit times, which can also contribute to dysbiosis or a small intestinal bacterial overgrowth (SIBO) and indigestion.
Lower thyroid function can cause lower gastrin levels, which are needed to stimulate HCL production. When patients are brought up to normal thyroid levels, their HCL levels return.
Low HCL and low thyroid levels can cause dysbiotic levels of bacteria in the intestinal tract. About 20% of T4 (inactive) thyroid hormone is converted to T3 acetic acid (AC) and T3 sulfate (S). The conversion of T3AC and T3S into active T3 requires an enzymes called sulfatase. The only problem is, sulfatase is found only in healthy bacteria.
In essence 20% of your thyroid hormone conversion is dependent on healthy digestion as well as a healthy gut biome. It’s amazing the interconnectedness between your hormonal system and your gut. It makes sense why Nobel Prize-winning physician Dr. Mechnikov is quoted as saying, “Death begins in the colon.”
The bacterial infection H. pylori is a common infection in the United States and is infamous for causing stomach acid. H. pylori also secretes an enzyme called urease. Urease breaks down urea into ammonia, which can have an effect on lowering your HCL levels.
In other words, depending on how much damage is present in the patient’s gastrointestinal tract, it may require outside sources of exogenous HCL and/or use of Swedish bitters to help regain the patient's own HCL productions.
The majority of thyroid conditions diagnosed in this country are Hashimoto's, an autoimmune thyroid condition. This condition is a little different from your primary hypothyroid condition as it’s the patient’s immune system that causes the damage. Giving someone the standard of care treatment, Synthroid, will not stop the autoimmune thyroid destruction.
Research shows a significant correlation with the eradication of H. Pylori and a reduction in thyroid antibodies. It’s as if the H. Pylori is a contributing factor to the autoimmune thyroid condition.
If you are trying to get to the root cause of your thyroid condition, click here for answers!
References:
Duke, J. A. CRC Handbook of Medicinal Herbs. Boca Raton, FL: CRC Press, 1985