
Dr. Justin Marchegiani and Evan Brand dig into a lot of the things that you need to know about SIBO — the causes, lab tests and treatments available for small intestinal bacterial overgrowth.
 Learn to differentiate SIBO from other digestive issues and/or infections when you listen to this podcast interview. Get to know about symptoms and lab tests to confirm SIBO as well as the functional medicine approach that will pave the way to gut healing. Find out the root cause of your gut problems and not just focus on the issue of SIBO so you can get effective treatment immediately.
Learn to differentiate SIBO from other digestive issues and/or infections when you listen to this podcast interview. Get to know about symptoms and lab tests to confirm SIBO as well as the functional medicine approach that will pave the way to gut healing. Find out the root cause of your gut problems and not just focus on the issue of SIBO so you can get effective treatment immediately.
In this episode, topics include:
3:57 What is SIBO?
6:59 Testing for SIBO
10:27 Causes of SIBO
12:13 Autoimmune Paleo Diet/Specific Carbohydrate Diet/Low FODMAP
26:10 Treatment with supplements
![]()
Dr. Justin Marchegiani: Evan Brand, it’s Dr. Justin here, man! Happy little Monday! What’s going on for you?
Evan Brand: Hey, thank you! Well, this baby is coming apparently. That’s what’s coming.
Dr. Justin Marchegiani: It’s exciting. I know we talked about it on Friday. You were getting close, still not quite there yet but you’re almost coming down the hill on this one.
Evan Brand: By the time this show goes out, the baby will be here.
Dr. Justin Marchegiani: Super exciting!
Evan Brand: Yup.
Dr. Justin Marchegiani: And this is gonna be a Paleo baby, right?
Evan Brand: Yes, absolutely.
Dr. Justin Marchegiani: Nice. So do you have a Paleo baby name set up yet?
Evan Brand: Su—Summer.
Dr. Justin Marchegiani: Oh, is that the name?
Evan Brand: Yeah.
Dr. Justin Marchegiani: Oh, awesome! That’s great!
Evan Brand: Yeah.
Dr. Justin Marchegiani: Very cool. I know, if it was like a—a last minute kinda judgment call. That’s cool.
Evan Brand: Thanks, man.
Dr. Justin Marchegiani: Perfect and it—it’s almost, it’s not quite officially summer yet, June 21st, right?
Evan Brand: By the time this show goes out, it probably will be June 21st.
Dr. Justin Marchegiani: It probably will be. Yeah, actually it will be past that. I guess it’ll probably come out in late June. So that’s great. Awesome timing. Good to hear.
Evan Brand: Yup.
Dr. Justin Marchegiani: Any other updates on your end here?
Evan Brand: Everything’s great. Just seemed to be plucking away at any road blocks that have been in my health journey and—and other’s journeys. So I think every week you and I chatting about a new topic is really empowering people. I’m continuing to get good feedbacks, some new 5 star reviews on this show for iTunes, so everybody seems to be liking the direction that we’ve gone with these—with these episodes. So it’s always good to have the feedback.
Dr. Justin Marchegiani: Love it. Love it. Any good treatment cases last week that you wanna share?
Evan Brand: Last week, let’s see. I’ll look at the calendar and that will help me to refresh my brain. Yeah, actually I do have a good one. So a guy is actually a rocket engineer. He builds rockets for shooting up satellites and spaceships–
Dr. Justin Marchegiani: Yup. Uh-hmm.
Evan Brand: Into outer space and his brain is not working as well as it should be.
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: So immediately upon starting to work with him, I got the Neuro Synergy product to him, which is several different brain vitamins and I got an email this morning and that said that his brain is starting to work better. So within less than a week, changes in cognitive function, that’s pretty insane. So the huperzine and some of the other brain-boosting nutrients that I’m using with him is very effective. So I think sometimes we don’t have to wait for people to have their lab test results. We can just immediately throw some nutrients their way that we know they’’ll benefit from that might help them and can’t hurt them, so to give them that motivation because you and I like to get people at least 5-10% better each month and if we can get you started on some nutrients while you’re waiting for your labs, then that’s gonna be great.
Dr. Justin Marchegiani: 100%! Same here with me. I mean, we have lots of autoimmune patients that come in every single week. We make simple dietary changes like transitioning to an autoimmune and/or throwing in a low FODMAP eating plan and we see remarkable changes and then we just add just simple things, like getting extra nutrients in through a good high-quality multivitamin. Getting better digestive support on board there, helping to support the hormones and the adrenals or diagnosing any underlying thyroid imbalances and getting rid of infection. It’s amazing just what type of healing capacity the body has when you just remove those roadblocks.
Evan Brand: Absolutely! My sleep’s been better than it has in probably 5 or 10 years. So who knows how long I had my gut issues going on? Like seriously. Every day I wake up, I’m like, “Wow! I was sleeping deep.” It’s just mind-blowing.
Dr. Justin Marchegiani: Well, you’re gonna need that sleep with this new girl on the way here so–
Evan Brand: Tell me about it!
Dr. Justin Marchegiani: You’re gonna need efficient sleep.
Evan Brand: I know.
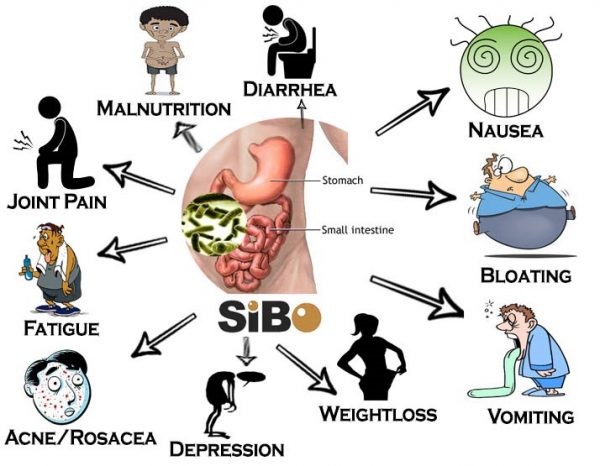
Dr. Justin Marchegiani: Great. Well, we talked pre-show that we were gonna address some topics of SIBO today, and then we’ve kinda interlaced or intermingled SIBO in other topics that we’ve addressed on parasite infections and probiotics and other types of digestive issues, but today this is gonna be a podcast just focused on SIBO and—and what SIBO is essentially and just to kind of give the abbreviation here, SIBO stands for small intestinal bacterial overgrowth and to keep it really simple is that we have a lot of the bacteria from the large intestine kinda creeping its way back into the small intestine. In a nutshell, that is what SIBO is. It’s basically bacteria from the colon kinda being in the wrong spot in the intestinal tract typically making its way back towards the small intestine. I’ve done a lot of videos on this. I know you have done some stuff, too. So go to justinhealth.com or notjustpaleo.com and Google just SIBO and you get a lot more info on this. But essentially we have that ileocecal valve that kind of is the capacitor that restricts entry from the small intestine to the large and it starts to open up and we start to have this bacteria creeping back into the small intestinal tract.
Evan Brand: Yeah, so looking at some of the research, the latest statistic I found here is that in terms of like irritable bowel syndrome, you know, SIBO is one of the most common causes of IBS, so it certainly could have been a factor for me with my IBS struggle. It says here up to 84% of IBS cases have been linked to SIBO. So if you’ve been told by the conventional doctor, if you go in and you have some of the constipation, diarrhea, bloating, abdominal pain, all the other symptoms that can happen. You go to the gastroenterologist that you probably get referred to, they’ll just say you have IBS. It might be SIBO and that’s certainly what I’ve seen and definitely you’ve talked about it all the time. You see it every single week how many people are dealing with this. So it’s—what would you say? 6/10, 7/10 people that are presenting with gut symptoms actually have SIBO?
Dr. Justin Marchegiani: Yeah, I mean a lot of people that are coming in with digestive issues more than likely have SIBO. The question is, is SIBO the root issue? So we know a lot of the SIBO symptoms are abdominal pain, discomfort, bloating, diarrhea, constipation, gas bloating, etc. And a lot of people that have gluten issue or other infections like H. pylori or parasitic infections or fungal overgrowths which may not be considered SIBO per se, but they tend to mimic a lot of those small intestinal bacterial overgrowth symptoms, so we wanna rule those out because I consider the deeper infections upstream issues and I can consider the lot of the SIBO stuff downstream. Now it’s not to say that SIBO isn’t a contributing factor. It’s not to say that we don’t have to address the SIBO because a lot of the herbs that we use to knock out the higher up infections can be sensitive to a lot of the SIBO type of overgrowth that we see anyway. So in other words, SIBO is important. Most of the people we always wanna rule out the upstream stuff first. I typically don’t ever go to your typical SIBO breath test to evaluate SIBO until we’ve ruled out the deeper infections because if we have H. pylori, if we have a parasitic infection like Giardia, Crypto or Blasto, it makes sense that the collateral damage of SIBO, that bacterial overgrowth will be there.
Evan Brand: So you’re saying it’s not even worth it technically if you just go straight to the typical hydrogen-methane test at this point. We need to really look at running the comprehensive stool panels first with people presenting with these symptoms because that’s gonna give us the most bang for our buck in terms of identifying underlying causes and if you go in and treat SIBO but you haven’t removed the infections and people will still struggle, right?
Dr. Justin Marchegiani: I see that a lot. I’ve seen a lot of patients that have come from other functional medicine doctors that just specialize in SIBO–
Evan Brand: Yeah.
Dr. Justin Marchegiani: And have only had their SIBO treated per se and they may use the—the conventional SIBO antibiotics which are like rifaximin or neomycin, a 10- to 14-day kind of dose of that, typically 500 to 1000mg b.i.d., it depends on what the doctor prescribes on that. So I’ve seen that and then they still come in with symptoms and then we’ll test and then they have Blasto—Crypto or Blasto, and H. pylori. So I think SIBO is important to assess and we’ll talk about how we can assess that but we wanna rule out the upstream. I always upstream to downstream.
Evan Brand: Yeah.
Dr. Justin Marchegiani: What could cause the most collateral damage to the least, that’s kind of how I assess things. It’s pretty conservative that way we’re not doing 100 tests at once. You know, we can start with 1 or 2 tests, focus on the gut, cross those off our list and then go downstream to a SIBO assessment. Now there’s typically 2 for the most part. There’s the more invasive sample where they’re going into the intestinal tract via endoscopy, right? Through the mouth down the esophagus and doing some kind of a sample to look at that—get a—a sample of that bacterial issue, that’s one way. That’s like the most, like the gold standard, because then you know, okay, I’m getting this sample of this bacterial overgrowth sample and it’s coming from the small intestine and we know and we can confirm that shouldn’t be there. It’s an overgrowth. That’s like sample #1 or measure #1 but it’s pretty invasive.
Evan Brand: Yeah.
Dr. Justin Marchegiani: Typically don’t do that unless someone’s very, very sick and it’s typically done by the conventional doctor ahead of time. In a less invasive way, it’s what’s called a small intestinal bacterial overgrowth breath test, where they give a sample of lactulose or sometimes if we’re looking at the upper small intestine, the upper stomach I should say, they’ll—they’ll give a sample of glucose, but typically lactulose because it takes about 100-120 minutes, about 2 hours or so to get down into that lower small intestinal tract, you know, by that duodenum and ileum area, that part of the intestine, and then we can see elevation in certain gases, whether it’s elevation in methane, whether it’s an elevation in hydrogen or we’re looking at a—a combination of methane and hydrogen together, and that’s typically what we’re looking at and we’ll see things, a greater than increase in methane above 3, some will say is an issue and could be indicative or SIBO, some say above 15–
Evan Brand: Uh-hmm.
Dr. Justin Marchegiani: Typically if we’re looking at a combination of methane and hydrogen, somewhere between 15-20 is gonna be positive. Again, some of the test will have these ranges on it like if you look at the National College of Naturopathic Medicine, they’ll have their ranges. Commonwealth Labs will have some ranges, too. I think there’s another lab called ARO Labs, their another one that has–
Evan Brand: I don’t know–
Dr. Justin Marchegiani: SIBO as well.
Evan Brand: I don’t know if you saw BioHealth doing SIBO now. They just released it.
Dr. Justin Marchegiani: Oh, I didn’t see that one.
Evan Brand: Last week.
Dr. Justin Marchegiani: Oh, that’s great!
Evan Brand: Yeah.
Dr. Justin Marchegiani: And it’s breath testing?
Evan Brand: Yup.
Dr. Justin Marchegiani: Oh, that’s great. I’ll have to–
Evan Brand: Yeah, I’ll–
Dr. Justin Marchegiani: Subscribe to that test.
Evan Brand: Yeah, I’ll send you—I’ll send you the clinician sheet about it here. And let’s talk about some of the other causes, too. So you talked about parasitic infections, like if there is an infection in the gut, that could definitely cause SIBO because of the damage that’s gonna be done and you talked about the diet a little bit, too, you know, in terms of like patients doing a lot better with a low FODMAP diet. So if we see like a lot of carbs, sugars, fructose, that’s gonna be an issue. If they were on PPIs before. What are those—what are the common brand names of the PPIs? Is it like a Prevacix, what is it called?
Dr. Justin Marchegiani: Yeah, you have Prevacid. You have omniprazole.
Evan Brand: Prevacid.
Dr. Justin Marchegiani: With the generic.
Evan Brand: Yeah.
Dr. Justin Marchegiani: You have Nexium. You have Prilosec.
Evan Brand: Which are all over-the-counter at this point? They almost all used to be prescription. I guess now the patents are up so people can do and destroy their gut with these things by just jumping on a strong PPI like that. Candida, a lot of times if you have candida, you’ll have SIBO at the same time.
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: If you went through antibiotics. Let’s say that you’ve got like bronchitis or you got some type of sickness and the doctor threw you on a round of antibiotics. That can really be a good—a good trigger for SIBO and I’ll see that a lot and that’s one of my intake questions is, have you gone through a round of antibiotics recently? And a lot of people say, “Yes.” And so we don’t necessarily have to go straight into the SIBO test like you say. If we get the stool panel run or the organic acids, so we can see like infections and candida overgrowth, a lot of times the treatment for that is gonna overlap and start working at getting rid of the SIBO in a way, right? If we’re using some of these natural antimicrobials and herbs and say oregano, garlic, things like that, we may knock out the SIBO just as a by-product of getting rid of a parasite or bacterial infection.
Dr. Justin Marchegiani: Exactly. So when we look at that, the fore of the first dietary changes we’ll do is that I always typically start with an autoimmune diet because a lot of the symptoms of inflammation can be a lot of SIBO symptoms. So cutting out things like nuts and seeds, and—and nightshade vegetables and even eggs, just off the bat, get them to a baseline autoimmune kind of diet is—is a good place to start. And then from there what we typically do is we assess. We’ll reevaluate a few weeks later to see how we’re doing. We’ll probably add some hydrochloric acid and enzymes in because a lot of patients that have these issues, they’ll have—they’ll have a history of being on PPIs like I mentioned, these acid-blocking medications. These acid-blocking medications create further deficiencies in nutrients, such as various minerals like magnesium, selenium, zinc, and we need some of these nutrients for healthy thyroid, adrenal relaxation, and even to make hydrochloric acid. So you can see once you have one of these underlying issues, they can tend to compound the problem and make it worse and worse over time. So then people continue to get worse over time and they tend to go back and lean on those medications that cause a problem in the first place. So then you got this rabbit chasing its tail around, and the problem gets worse and worse over time.
Evan Brand: Yup. That makes perfect sense. So just in terms of the diet piece, I often hear of like this Specific Carbohydrate Diet which in a way I would say the autoimmune Paleo diet’s pretty close to the SCD, wouldn’t you?
Dr. Justin Marchegiani: Autoimmune Paleo Diet is pretty close to the SCD, yeah. So the SCD, when we look at the SCD, there’s one out there by Allison Siebecker that’s an SCD and a—a SIBO one, a low FODMAP when that’s combined. So in my member’s area, my patients have access to this where we’ll sometimes give the SCD in conjunction with the low FODMAP so the—the SCD is called the Specific Carbohydrate Diet. And what’s different about the SCD is it’s various phases of introducing foods. Typically foods start off, they’re really simple. It’s just meats and maybe some carrots off the bat. Everything’s peeled and even cooked pretty well or even mashed so there’s no outer coating. It’s low in salicylates, low in phenols. So you have your meats. You have basically your carrots and then the next phase you may start to add in a couple more vegetables and maybe a little bit of apple or pear sauce and then you go up to—to level 2 and level 3 and level 4 and you gradually introduce more and more foods. Now if you’re following a straight SCD or Specific Carbohydrate Diet, that may still have some FODMAPs in it. So we gotta be careful. So we may put a combination of an Autoimmune/SCD and low FODMAP together. It really just depends on what the person’s history is. If they have a—an underlying ulcerative colitis or Crohn’s issue. We typically go autoimmune in conjunction with low FODMAP, in conjunction with kind of a low salicylate, low phenol, SCD approach. Because some foods like potatoes are technically low in FODMAPs.
Evan Brand: Right.
Dr. Justin Marchegiani: Same with tomatoes as well, right? Same with eggs. But people that have autoimmune stuff, they may be sensitive to those things. Even nuts are supposedly okay on a low FODMAP, right? Sometimes, alright, if you look at Allison Siebecker’s they’re considered to be okay, but if you look at other low FODMAP diets, nuts are not acceptable and also nuts are not acceptable if you are on an Autoimmune Diet. So we get a little bit more strict on how we approach things, just because I have, you know, hundreds of data points of patients doing well on this approach. So it’s really tough off a bat. It’s not meant for a forever thing, but it’s meant to just kind of cross our T’s, dot our I’s, find out what foods we’re sensitive to, cut out some of the inflammation and significantly reduce a lot of the bloating and gas and a lot of those constipation and diarrhea, SIBO symptoms as we get the person better.
Evan Brand: Yeah, and lot of people if they’ve suffered long enough, they’re open to that and they’re willing to do that but if—if some people they haven’t gone strict with the—the diet, it may feel like we’re taking a lot of good stuff away from you, but this is gonna help to speed up your process of you getting better because if we’re relying just on one treatment whether it’s the herbs or some of the other botanicals, you can get better but it may take longer. So like Justin’s saying here, if we’re improving the diet and stacking that on top of the good lifestyle, getting the good sleep, all the other factors still are important, that’s just gonna make sure that you get better faster, and that’s the question that we often ask is how quickly do you wanna get better? And that will determine, you know, how deep or how intense we can go with stacking all of these on top of one another, and maintaining a normal life that’s pretty free of symptoms overall.
Dr. Justin Marchegiani: Exactly. Yup, exactly, 100%. So regarding some of the testing I mentioned, the glucose testing, to look more in the upper small intestine—on the upper stomach tract. Lactulose is typically, you know, the—the best one so to speak because of the slow breakdown of the lactulose. Again, if we have some type of gastroparesis or some type of significant motility issue, it may take longer for that lactulose to get down there and that we may see an issue with that being delayed on the breath test. Like if we’re only doing a two-hour breath test, right? Like the Genova one, but it takes 3 hours to get down there, we may miss that infection, right’? So some people will actually have them wait an extra hour than start the test at the first hour in and then we can get a good window of that, so and it’s also if faster motility, then it may go too fast, so you gotta have to kinda weigh those, weight the odds of—of both of those different testing there. And then also I did a whole video on how to do some of these tests, alright, like what the data says and what we’re looking at but I kinda mentioned some of the things, greater than 3 on the methane and 15-20 is—tends to the point that we wanna look at for hydrogen and/or methane. Typically 20 or above combined hydrogen-methane is positive, 15 or above for hydrogen, and again that can change from test to test, so I did a deeper video on that and how to interpret it.
Evan Brand: Great. Yeah, and so it looks like—looks like BioHealth is gonna be a better solution than the Genova, looks like there’s 3—it’s a 3-hour test here with 10 breath samples. So I think this might be the new gold standard for us.
Dr. Justin Marchegiani: Oh, I like that. That’s great. I’m gonna have to order one and get access to that ASAP. Yeah, I see, May 23rd. It just came out. That’s phenomenal.
Evan Brand: Yeah.
Dr. Justin Marchegiani: Very cool. So regarding testing we already talked about kinda my philosophy looking at the upstream infections, that’s important. And there’s a lot of people out there, a few people out there I can think of off the bat that are—are not in favor of adrenal testing. Now I understand where these people are coming from, these clinicians. I don’t necessarily agree, because I think people have significant inflammation on their backs and on their bodies, and they have a very difficult time regulating it. And when we see someone that has decent adrenals but has gut symptoms, that matters versus someone that has very impaired adrenals, and what I mean by impaired, let’s say a flat adrenal rhythm, or let’s say a reverse cortisol rhythm and/or very low depleted sex hormones. Now some of these clinicians are basing these off of symptoms but I can tell you many times that I get surprised every now and then and now that I’m doing the 201 by BioHealth and the newer Dutch testing, you’d be surprised how often you get surprised with some of these people’s clinical presentations. And sometimes when I see that, then I got to the thyroid and it’s really the thyroid that’s really the—the weak link in the chain. So I’m a big fan of looking at the adrenals because it gives me the ability to look at what that patient’s capacity for regulating inflammation and stresses and also gives me a window into their sex hormone outputs so how fast they can heal and also how dysregulated is their cortisol rhythm. Alright, the Whitehall study found that the closer that morning cortisol is to that night time cortisol, an increased risk of cancer even greater than cigarette smoking. So cortisol rhythm to me is important and it also gives patients when they come in with a real crappy rhythm or a very low sex hormones, it gives them a bull’s eye to shoot for. So it really creates a significant level of compliance because that patient knows they got a test in 6 months that they’re studying for so to speak, and by studying I mean going all the diet and lifestyle things and being compliant with the treatment because then we can follow-up and see how we’re doing and then we can have a real specific treatment. So to a lot of those doctors out there, I think they’re—they’re missing the boat a little bit and I think they would get better patient compliance and I think they’d be surprised that some patients are probably slipping through the cracks because their adrenals are terrible and that would allow them to provide a better prognosis on where they’re going based on their patient’s inability to regulate stress and inflammation.
Evan Brand: Absolutely. Yeah, that’s a great point and that ties into the gut. People may think, well, why are you talking about adrenals? But this whole adrenal cascade, this is going to affect the gut, so—which we may have talked about briefly in another episode, if you’re unable to regulate your inflammation because you do have adrenal issues then that’s gonna leave you more susceptible to the gut. So if you’re only focusing on the gut and what a lot of practitioners do, I—I mainly think for marketing purposes is to kind of pigeon-hole themselves into being say a SIBO specialist or a gut specialist but you honestly can’t get people better 100% if you are a specialist. Is that a safe statement to make because if you’re only focusing on SIBO and you’re just killing off all of these bacteria but yet they have wrecked adrenals a leaky gut situation is still there because they have say high cortisol all day, you can’t get someone ultimately better. That seems like they’ll just spin their wheels.
Dr. Justin Marchegiani: Yeah, I think it’s great to be able to market to the public as you specialize in this area, but I think it’s important that you still, you know, flex your holistic muscles that yeah, even though I specialize in here, I still connect in the adrenals. I still connect in the gut.
Evan Brand: Right.
Dr. Justin Marchegiani: I still connect in the detoxification issues along with it, so even though we’re really focused on this one issue, we are not myopically focused where everything else becomes non-existent in our periphery.
Evan Brand: Exactly.
Dr. Justin Marchegiani: So I think–
Evan Brand: That’s well-said.
Dr. Justin Marchegiani: I think that’s really important because that’s where conventional medicine’s kinda gone wrong, where the cardiologist only knows about the heart and doesn’t know about the hormones and vice-versa for the endocrinologist and the gastrointestinal doctor, right? But we know how important all of those things are connected.
Evan Brand: Yup, absolutely. I had another thought and I think I lost it. It was about—oh, just in—in terms of SIBO, you know, I’ve already kind of said this so I may be repeating myself but basically if someone is just throwing themselves on the antibiotics or the herbal antibiotics, you may spin your wheels and you were talking about how the—the importance of adrenal testing even for gut issues. Last week, I had a female in her 60s, I—if I would have guessed, I know you and I kind of put things in our head, “Oh I think this person’s gonna show up like this.” I would have guessed that she was flat-lined with her cortisol, however, she had a sum of over 60. Her cortisol sum was insanely high and her cortisol rhythm was insanely high, yet she had tons of fatigue yet had some anxiety in the evening. So I thought, “Oh, maybe we’d see an elevation in the evening.” No, her cortisol was just off the charts, the highest I’ve ever seen ever. And now I found that out and I wouldn’t have been able to start working on the fatigue if I would have thrown her on something stimulating like licorice, I would have created a disaster for that woman. She would have felt worse. So without that piece, it’s really scary to—to jump on a program.
Dr. Justin Marchegiani: Exactly and the big thing we’re trying to do in functional medicine is we’re trying to use objective lab testing to really drive compliance because patients have been told already that have come and seen us that it’s all on their head and they need something to show, “Hey, this is a window under the hood of what’s happening with your physiology, your hormones, and your biochemistry. It’s real.” And then now from that, we’re gonna re-test in a certain amount of time, so the pressure’s on you to be compliant so then they know “Hey, we’re gonna be making these changes and we’re gonna be re-testing,” so they’re gotta do their part. And then also and make sure that we are—we aren’t guessing, we are assessing. Because I get surprised every now and then. So I think some people are missing the boat on that from a clinical standpoint. I understand why they do it because they’re hyperfocused on—on cost and such. And I get it, if someone, you know, has significant financial issues and they don’t wanna do a certain test, but my issue is you wait 2 or 3 months and they’re not quite feeling where they want to, almost everyone regrets not running that test 2 or 3 months ago, right?
Evan Brand: Yeah.
Dr. Justin Marchegiani: It’s never—I mean maybe you may start getting better and you’re like great, it worked out, but if you don’t feel better in that couple of months, then you’re gonna really wish you did that test because then you have a little more confidence in what direction you’re moving forward with regarding your treatment for your SIBO issues.
Evan Brand: Yeah, and that’s sort of like if you’re buying something really cheaply, like say you just buy a little piece that may fit the job for a tool that you needed at home, but then that screwdriver breaks, now you have to go buy another screwdriver and then that one breaks, and then eventually you’re like, “You know what, I’m gonna buy a screwdriver with a lifetime warranty.” It’s just gonna last you a lot better, but yet you’ve spent double or triple because you’ve been trying to only use an incomplete puzzle I guess is what I’m saying.
Dr. Justin Marchegiani: Yup.
Evan Brand: Like if we try to focus on, “Oh, let’s just look at adrenals,” then that’s what—what I did in the beginning because I was just trying to just prioritize things for people and now I’ve come to the conclusion and you have a long time ago, this conclusion, we really don’t want to just look at this one piece. We really have to try to get this full puzzle upfront with someone because then we’re delaying the success that they get and then they blame us but it’s—we don’t have the data, so we can’t work without the data.
Dr. Justin Marchegiani: Exactly. So I always tell patients, the longer you’ve been sick, the more sick you are and the faster you wanna get better, it’s better to pull a couple more labs out so we have a—a more complete picture. The shorter you’ve been sick, the better you feel, and the less motivated you are to get better, then we can start with just like something like one test.
Evan Brand: Right.
Dr. Justin Marchegiani: But I always tell patients, it’s better to do something over nothing because then we can start moving forward versus you know, sliding backwards.
Evan Brand: Right.
Dr. Justin Marchegiani: So a couple more things on the SIBO, a couple of the herbs that—that I formulated and use. I use a couple in my practice. One is called GI Clear One and one is called GI Clear Six. They each have some various herbs I use that have some high amounts of berberines or Artemisia compounds in there, cloves, Java Brucea, wild indigo, just various herbs that had shown to be very sensitive to killing some of the gut bacterial overgrowth, okay? That’s number one. There is some other ones out. There’s been studies looking at the antibiotics, the Neomycin or the—the rifaximin and rifaximin is the same thing as Xifaxan, FYI. And then the combination of the—the neomycin with the—the herbs. So looking at just the antibiotics and then looking at just the herbs, there’s been some studies showing that herbs actually work better. Now when in doubt, if you’re gonna just say, “Well, I wanna go the antibiotics,” still go with the herbs because the herbs have a really good effect at knocking out biofilms, too, and some of the antibiotics won’t touch the biofilms, that’s number one. And then number two, people need a longer dose of these antibiotics and people that do long-dose antibiotics can wipe out a lot of their beneficial flora so combining it if they are with the anti—with the herbs are gonna be beneficial because herbs are shown to be just better clinically taking it over the long period, safer, less side effects than a lot of the antibiotics would. And you have couple 10,000-year history with these herbs being used by various tribes and cultures to help with infections and parasite stuff and like wormwood and with malaria, and like mastika on the island of Chios in Greece for all kinds of different issues with the H. pylori and other issues. So it’s nice to use the herbs. I’m biased towards the herbs because of their safety, because of their long-term history and because of our ability to use it long-term and the ability to affect things like efflux pumps, which are kind of the bacterial way of bailing water out of sinking ship. So imagine antibiotics coming in and the—the ship bailing, and those antibiotics back into the intestinal tract creating more bacterial overgrowth because it’s knocking out a lot of the good stuff. So those efflux pumps get affected more by the—the herbs and they also affect some of the biofilm, which are like the protective shields that these infections use to protect themselves from getting killed.
Evan Brand: Yeah, I’ve seen a few studies about enteric-coated peppermint oil as well.
Dr. Justin Marchegiani: Yup.
Evan Brand: And I used that when I suffering a lot with IBS. I wasn’t into the herbs, so I didn’t know enough about the herbs at that point. So I was using the peppermint oil and I had great success and that’s something I’ve given to my dad, too. He’s had a lot of issues with his gut and it has been incredibly helpful. It’s hard to find a clear piece of research that says whether you would be able to use the enteric-coated peppermint oil specifically for treatment of SIBO, like if you can knock it out by itself, what do you think? Maybe in a—in a low overgrowth situation, it could give you some antimicrobial benefit but I think you’re probably gonna need a bit more of a well-rounded approach by adding in the herbs on top of that.
Dr. Justin Marchegiani: Yeah, I mean, typically I would never rely just on one herb by itself.
Evan Brand: Yeah.
Dr. Justin Marchegiani: I would do a combination of a couple. If you look at my GI Clear One and GI Clear Six, we do that in those products. In my GI Clear Five, that’s the pure emulsified oil of oregano; we’ll hit that up really hard as well and then we’ll even use my GI Clear Three which is silver and that’s a really good biofilm buster, and then we always like to throw in ginger because there’s a lot of research on ginger busting out biofilms, too. So we do a combination of different things and we’ll even interject the low FODMAP diet and sometimes we’ll even start eating a little bit of FODMAPs while we’re doing the killing because it’s kinda like putting cheese on a mousetrap for the so-called mouse, i.e. the bacteria to come out of hiding. When it comes out—BOOM! We’ll use those herbs and really knock them down to size.
Evan Brand: That’s great! That’s really interesting concept there.
Dr. Justin Marchegiani: And look at your situation, right? You would have what I would consider to have a—be a lot of SIBO symptoms. Like if you went to one of these SIBO docs that are out there, the first thing they would have had you done was SIBO testing–
Evan Brand: Yeah.
Dr. Justin Marchegiani: Without a doubt. But look, what came back on a stool culture, right? We’re talking an actual, you know, under the microscope, you know, stain/culture diagnosis. You came back with Giardia and Crypto, correct?
Evan Brand: Correct.
Dr. Justin Marchegiani: Yup. If you did a breath test, you would have came back and they would have been just all 100% myopically focused on the gases. “Oh, those methane and hydrogen are high, we gotta knock them down.” But if you looked upstream, you’d see you’ve had 2 major infections that would have been missed.
Evan Brand: Yup, I know. And I—I would have suffered. Maybe depending on how heavy hitting the treatment would have been for the SIBO. If it was a very heavy hitting treatment, tons of garlic, tons of the oregano, the berberine–
Dr. Justin Marchegiani: They have may have got it by accident, right?
Evan Brand: Exactly. But I wouldn’t have known and what if I—let’s just say, what if I did the SIBO treatment for a shorter duration than necessary to get rid of the parasites then my symptoms would have come back and then I would have been well, that didn’t work, why not?
Dr. Justin Marchegiani: Right?
Evan Brand: So–
Dr. Justin Marchegiani: Especially a lot of these SIBO infections aren’t known to be as contagious like these parasite infections. These parasite infections can be fecal-oral, can be spread by intimacy wherein not quite as much as with the—the general SIBO stuff, right?
Evan Brand: Yup.
Dr. Justin Marchegiani: Because the SIBO really is a whole bunch of different bacteria that are just overgrown so to speak. So–
Evan Brand: Right.
Dr. Justin Marchegiani: We—we wouldn’t think of that as being like a—a contamination or potential, you know, thing that can be vectored per se, but when we deal with infections, H. pylori, to—kind of be added in there, we have a different perspective on the—you know, the spouses and the partners that could be affected in there and contaminated with.
Evan Brand: Yup. And so I think that’s a pretty good overview. We talked about the testing, getting the full panel run, making sure you’re getting some stool testing run with your practitioner, making sure you’re getting some adrenal testing to see how much is this cortisol issue—how much is that contributing to your leaky gut, making you more susceptible to pick up bacterial and yeast overgrowths and parasite infections. And then we talked about some of the herbs and then combining those for the synergy. We talked about the diet in terms of watching out for the FODMAPs potentially doing like an SCD or an Autoimmune Paleo Diet for the time being then re-introducing things, seeing how you feel. Is that—is that the 4 pillars? Is there any other missing piece?
Dr. Justin Marchegiani: Yeah, for the most part. Let me just go through it at my head. We have the 5R’s. So we’re removing all the bad foods, right? This could be but not limited to autoimmune foods–
Evan Brand: Yeah.
Dr. Justin Marchegiani: SCD, low—low, cutting out the higher phenols and salicylates. Cutting out the FODMAPs and potentially even cutting out histamines. The more messed up someone’s gut is, the more they have to be diligent and vigilant on their diet in the beginning. So some of these things may have to be removed. Next R would be the replacing. Replacing enzymes and acids to really help with the breakdown of these foods. Third R would be repair. Repairing the gut lining and/or adding in, repairing nutrients to reduce inflammation. So we may add in some specific strands of probiotics to help with the inflammation and the repair side. And also the adrenal piece, right? Helping to regulate inflammation better so we can put out the fire in our gut and we also know the adrenals are important for IgA production. Very low cortisol will affect IgA. So the repair involves potential probiotics, potential anti-inflammatory nutrients, and potential adrenal support. Fourth R is removing the infections, anywhere from the parasite to the—to the bacterial issue, to the fungal overgrowth to the SIBO, and the fifth R is gonna be reinoculation where we really focus on the probiotics even through it’s not a forever kind of thing. It still has an effect of receding at least for a month at a time and then the last piece after those 5 R’s are completed are retesting, making sure there’s no lingering infections that come to the surface.
Evan Brand: Nice.
Dr. Justin Marchegiani: That’s–
Evan Brand: Well said.
Dr. Justin Marchegiani: Yeah, that’s the overview.
Evan Brand: And—and I like how you painted out—you painted out the order of operations there and you did not say probiotics first. I think you and I discussed the female patient I had where she went to the naturopath, threw her on like a heavy—heavy dose of the soil-based probiotics and she blew up like a balloon, felt awful, tons of symptoms. Wrong order, wrong treatment.
Dr. Justin Marchegiani: Yeah and also if we’re gonna do specific kind of probiotics, I’m a bigger fan with my sensitive gut patients to use the one called Megaspore.
Evan Brand: Yeah.
Dr. Justin Marchegiani: It’s typically a Bacillus clausii, subtilis, coagulans bacillus kind of spore-like strain. It tends to be more sensitive to people that are what I call probiotic-intolerant. They get a lot of gassiness and bloating and digestive symptoms from probiotics.
Evan Brand: Yeah, she—she felt horrible and I was so glad to finally see in the flesh just because treatment sounds good, you just talked about the 5 R’s, you can’t just go straight to number 5. You have to do 1, 2, 3, 4, 5.
Dr. Justin Marchegiani: Most people wanna go to number 5 or number 4 because it’s sexy, right? Oh, probiotics and this!
Evan Brand: It is.
Dr. Justin Marchegiani: It’s just sexy.
Evan Brand: Yeah.
Dr. Justin Marchegiani: But number 1 off the bat, before they even, we have the 5 R’s, is gonna be get some testing done, right? Ideally, once you’ve—let’s say you tried cutting the FODMAPs out and you’re done AIP, great! If you’re getting results, good. I strongly encourage you at some point to dig in and get some testing done, right? That’s where looking at the body systems would be super helpful, organic acids testing and/or adrenal and/or gut testing will be helpful. The more symptoms, we may dig in to thyroid stuff. That way we get a complete picture. Now the worse thing you wanna be dong is guessing and then having all these things happening where you’re starting to get worse over time and you don’t know and you get—start getting scared and you’re like, “Well, what do I do next?“ Having the testing is super helpful and having a clinician that’s been there a couple thousand times really gives you a lot of confidence because, you know, if I’m climbing Mt. Everest and something happens, I wanna have a—a Sherpa or someone with me that’s—that’s been up that mountain dozens of times that knows the ins and outs.
Evan Brand: Absolutely, yeah. That’s a great point.
Dr. Justin Marchegiani: Any other comments on that? So we have the testing. We talked about the SIBO testing. We talked about the breath testing and just to kinda correlate symptoms, increase in methane gas can typically mean constipation, increase in hydrogen typically means diarrhea. We can have both. We can be alternating. So it’s to be able to coin some of those symptoms, right? Either diarrhea or constipation or some of the gases. It may hold true, it may not. And then we talked about the—the different testing, either the endoscopy sample. We talked about the breath testing. We talked about the actual gut testing as well, looking for the parasites. And then we talked about the periphery testing, either the adrenals or deeper organic acids testing to look downstream.
Evan Brand: Yeah, but say the only thing I would add to that is don’t be alarmed necessarily. This is a good conversation to have with your specific practitioner, but don’t be alarmed if things do get a little bit worse before they get better, especially if there’s like a parasite like I was dealing with. Things got a little bit worse before they got better. So don’t assume that it’s just gonna be–
Dr. Justin Marchegiani: Yes.
Evan Brand: A—a miracle solution. There may be this readjustment period that you’re gonna have to work through, a couple of speed bumps along the way but that can be normal to have an exacerbation of symptoms before they get better. And that’s—and that may be okay–
Dr. Justin Marchegiani: Yeah.
Evan Brand: But you need to talk with your practitioner to make sure.
Dr. Justin Marchegiani: Yeah and a good—some good references on the mainstream for this article here or this podcast would be Dr Pimentel out of the Cedars-Sinai over—over at California, Los Angeles there. Also Allison Siebecker and Dr Sandberg-Lewis out of NCNM, over at National College of Naturopathic Medicine. Those are some good resources and references on the whole SIBO thing here outside of you wanna kind of dig in to nitty-gritty, those are some good places to look.
Evan Brand: Good stuff.
Dr. Justin Marchegiani: Any other questions, Evan? Or comments or concerns?
Evan Brand: Not—not for today.
Dr. Justin Marchegiani: Like it, man! Well, go out and get sick people well and I’ll do the same.
Evan Brand: Amen!
Dr. Justin Marchegiani: Have a good one and best of luck with Summer coming into the world.
Evan Brand: Oh, thank you.
Dr. Justin Marchegiani: Take care, Evan.
Evan Brand: Take care.
Dr. Justin Marchegiani: Bye.
Evan Brand: Bye.