
Urinary tract infections (UTIs) are a common medical problem affecting millions of people worldwide. The primary source for UTIs is presumed to be the gut. That's why in this video, Dr. J and Evan talk about how gut bacteria can contaminate the urethral opening, eventually propagate themselves in the bladder, and cause symptoms of a UTI and possible yeast infection.
They also added that women are significantly more likely to get UTIs than men. It is due to anatomical differences that make it easier for disease-causing bacteria to travel to the urinary bladder after accidental transfer from the bowels. They also discuss the other clinical and evidence-based factors with helpful tests to find the root cause of these issues.

Dr. Justin Marchegiani
In this episode, we cover:
0:00 – Introduction
1:53 – Urinary System
10:54 – Antimicrobials and probiotics
18:55 – UTI and Yeast Infection
Dr. Justin Marchegiani: Excited to be here with Evan Brand. Today, we are gonna be chatting all about the gut connection with urinary tract issues, UTIs and yeast infections. Really excited to dive into this topic. This is the common female topic that we deal with. I mean, men deal with UTIs as well but men have a longer urethra area so it’s harder for men to have UTIs with them. Women have a much shorter urethra so bacteria can make its way up to the urinary tract and blood much faster and easier and so probably more of a female issue but we’re gonna dive in. The physiology is similar between the two so men listening will still get something of it as well. Evan, how are we doing today?
Evan Brand: Hey, doing really well. And so, looks like about 90% of infection in the bladder, 90% of these cases of these infections of bladder, urethra and kidneys, it’s all related to E. coli, which of course E. coli are in your poop and can generally just take route up that way and they can migrate and populate within the urinary tract and so women obviously know these symptoms if they’ve had it but it’s you have to urinate more frequently, it’s painful urination. It could be pressure in the pubic area. It could be fatigue. It could go more severe into kidney injury but most women are usually so miserable before they get to that point that they end up doing some sort of conventional treatment. So, why don’t we just talk about the conventional approach because I think it’s great to highlight what people are doing and then what we’re doing differently that we may argue is a far more sustainable solution without the side effects. Antibiotics are gonna be huge and we’ve got some statistics on this. Antibiotics are prescribed for 33% of women to combat a UTI before the age of 24 but of course these synthetic antimicrobials are not without short- and long-term consequences.
Dr. Justin Marchegiani: I’m gonna just share one thing here on screen just so everyone can see. So, you can see the female anatomy, right here is the urethra, here’s the bladder so you can see a very short distance from the urethra to the bladder. You can see here in the male anatomy, right at a much longer distance to get up here. Obviously in the urinary tract, you’re just typically with the UTI, it’s the bacteria that’s making its way up here, okay, into the urinary tract that’s causing the infection like Evan already mentioned that’s mostly gonna be bacteria, right? Usually on the UTI side, it’s gonna be E. coli there, can be some Pseudomonas, it’s mostly E. coli. And so, it’s really easy for women to get bladder infection because you can see it goes up faster. Again, things like birth control pills we’ll talk about and antibiotics really shift the urinary pH and the intestinal pH which has a major effect on the bladder and the urinary tract and it makes it easier for bacteria to grow that tends to be why women are a little bit more susceptible than that for bladder infection obviously but in general you’re gonna see that with birth control pills because how estrogen affects the pH and then also women when they menstruate, right, just that whole vaginal area right there, sloughing off that endometrial lining. All that blood flow does shift that whole entire are to be way more alkaline because bloods around 7.3 pH so it does shift that whole vaginal tract to be more pH higher on the pH side which can increase other bacterial infections more on the vaginal side but hopefully that helps. Any comments on that, Evan?
Evan Brand: Yeah. It’s totally interesting and this is stuff that maybe you didn’t pay attention to in school and biology class but now in adulthood it’s a lot more important and I think people just don’t even understand the anatomy of it and this is something that according to the research here, 25% of people treated for UTI, they will experience a recurrence 6 – 12 months later. So, I mean, that’s a quarter of these people that now have another UTI and they just go on this merry-go-round. And of course, every time you go on these antibiotics, you’re damaging the mitochondria, you’re damaging your gut microbiome in total, so it’s not just this one thing that you’re doing, it’s the sum to your system and it can really add up.
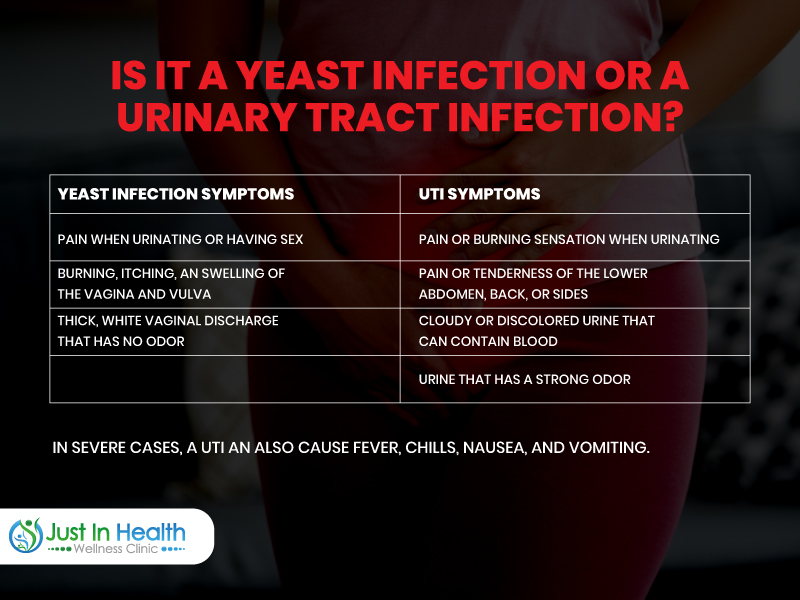
Dr. Justin Marchegiani: Yeah, when we deal with urinary tract issues, I kind of look at, okay, you have yeast issues over here. They’re kind of, they intermingle right and how the different things happen. You have bacterial issues over here, right? So, your UTI issues are primarily bacterial, right, affecting the urinary tract. You can have BV, bacterial vaginosis, that’s another bacterial issue. Usually, Gardnerella bacteria is one that’s affecting the vaginal canal. So, a little bit different, right? Different, you know, same general area, different anatomy per se. You’re gonna have similar sequelae of tissues affecting it, right? The big difference with the BV issue is you’re gonna get the potassium hydroxide odor which is, that’s kind of the fish smell. That’s what the bacteria in the vaginal canal does, it creates that potassium hydroxide that’s the fish odor. You’re not gonna quite get the odor with the UTI but you will have the burning during peeing. So, that’s gonna be the big differentiating factor. Sometimes, more odor on the BV but sometimes you can have none and then of course more pain during urination on the urinary tract issue and then if that continues to be left up that bacteria will eventually continue to go north and eventually hit the bladder as you can see that anatomy pretty short on video here. But, one of the big common issues is I would say like the big three, anytime I look at this problem, they tend to be the same. It’s gonna be a combination of antibiotic use so we’re wiping out a lot of the good flora in our intestinal tract which also affects the vaginal or urinary microbiome and then that affects the beneficial probiotics that actually make hydrogen peroxide like probiotics usually make hydrogen peroxide which is antibacterial. They’ll make different acids, glucuronic acid, they’ll make acidic acid. Different acid acids that actually help keep the microbes in check. They make hydrogen peroxide H202 and it keeps a lot of the bad bugs down. So, the first thing is we have a wiping out of the beneficial flora that also drive yeast overgrowth too so the same thing where it wipes out the good stuff, the beneficial probioflora, the probiotics the Bifidobacter, the Lactobacillus. The different species within the Bifidobacter and Lactobacillus, right? There’s Rudaea, casei, plantarum, lactis, these are all beneficial species, okay, that keeps the bacteria in check but also when you knock down a lot of the good stuff that can also causes this rebound overgrowth and yeast and that’s a lot of doctors today even on the conventional side tend to give an antifungal after an antibiotic in a lot of these female patients because they see a lot of these symptoms happen frequently.
Evan Brand: Wow. And, you’re mentioning the antibiotic that starts this whole cascade and that’s not necessarily the antibiotic to treat an existing UTI and then we’re talking about these recurring UTIs. We’re talking antibiotics for something simple like, I’ve heard of some women going in for a dental cleaning or something just that seems benign and then boom the antibiotic just really had forced them to take another fork in the road with their gut health and of course the vaginal health is affected.

Dr. Justin Marchegiani: Exactly. Now, with urinary tract issues, I mean they’re simple things, right? Sometimes, just after intercourse, after sex, just not peeing. Sometimes that sperm and the semen being up there can kind of create some issues with bacteria so urinating after sex can be very helpful. You’ll see it with younger kids just wiping the wrong direction, right, essentially wiping back to front bringing some of the bacteria in the stool into that urinary vaginal area can be a problem. Sometimes different contraceptive methods like that involve, like a spermicidal intravaginally can sometimes mess up the milieu of flora in the vaginal tract. Having bladder stones or kidney issues can sometimes have problems, going in for a surgical procedure where they put in some of a catheter, you know, those are, you know, gonna be way unlikely but you know just kind of given the gamut of those across the board. And then of course, you know, the antibiotic exposure and I would even say just too much sugar, too much carbohydrate, a lot of bacteria like acellular easy to digest refined processed carbs. So, more carbohydrates, more sugar, more grains, more flours are definitely gonna work, you know, increase those microbes’ kind of having a feeding frenzy if you will.
Evan Brand: And, how can you find this out? Well, there's an easy to do at home test that you can buy for less than 10 bucks. You can do these test strips at home. These urinary test strips and if generally, you see a dark purple, you’ve got a big issue and so it’s something that people should have on hand if you’ve suffered for a while. I know a lot of women; they just hate having to go to the doctor’s office and get tested and then they leave with another antibiotic and then they’re on this merry-go-round. So, we talked about the conventional approach, they really as far as it goes antibiotics
Dr. Justin Marchegiani: So, with the test strips, I think most of them are primarily looking at either immune cell in the urinary tract. I think, a lot of times with yeast or bacteria. They’re looking for, like leukocytes or leukocyte esterase, they’re looking for bacteria or I’m sorry immune cells in there. I know, some of the yeast ones are looking at pH so they’re looking at a more alkaline type of pH. The more alkaline the pH moves from six to seven to neutral, right, neutral is around 7. Into the 7-ish range, that tends to say that okay we have more yeast issues or we’re starting to move back in the direction of bacteria if we’re starting to see some of these leukocytes moving into the urinary tract.
Evan Brand: Yes. It’s kind of an indirect marker, right? You’re looking at those leukocytes and that’s what you would be seeing in terms of like, the light purple, dark purple, extreme purple on the test strips.
Dr. Justin Marchegiani: Yeah. So, they’re looking at the immune system starting to come in there and obviously with a BV issue, bacterial vaginosis. They probably need a swab to see what’s going on there, see if it’s like a Gardnerella or a Pseudomonas or Klebsiella, you know, what the bacterial species is. Now, typically with yeast issues in the urinary tract, I’m sorry with, uh, yeast infections primarily gonna be Candida or Candida subspecies. With BV, it’s primarily Gardnerella and with UTI’s it’s gonna be E. coli, typically.
Evan Brand: Now here is the cool part. Are you ready to talk about some of the transitions you hit on the diet piece of a bit of sugar process things? Maybe we should hit this first and then we’ll talk about, like, the functional strategies that kind of thing. You and I were talking about this before we hit the record that so many people, they want the solution to an issue like this but they haven’t even got the foundation styled in, in regards to their sleep, in regards to stress, proper hydration, nutrient density, lack of antibiotics if possible. Just those foundational pieces, a lot of times, are gonna keep women in a place where they’re not gonna end up with this problem so if you’re just tuning in, somehow you found us and you’ve not been listening for a while and you’re just now hearing us and you’re looking for this magic remedy, you got to make sure you get the foundations in order first because in theory, this should not happen if you’ve got the foundation style then.

Dr. Justin Marchegiani: Correct and so first thing out of the gates is just foundational things like hydrating enough because if you have a UTI issue just having constant good water flow and also you know with some electrolytes in the water that can be very helpful kind of having an antibacterial effect. And just keeping that good water flowing, the solution to pollution is dilution so that can really kind of keeping things flushed down. Obviously, being very careful if you’re having antibiotics. Why did you have the antibiotics? Was it for routine preventative things? Was your diet off and your immune system’s weak and you got sick and you needed it? Why, right? So, you want to look at that and if you had chronic antibiotic use, you know, what does the bacteria in your gut look like because odds are, if your bacteria or yeast imbalances are present in the vaginal tract or the urinary tract, you probably, also have issues in the digestive tract. You may have SIBO, you may have bloating, you may have gas, you may have poor digestion, low enzymes, low acids, H. pylori, parasite infection, you may have to look deeper in the intestinal tract and actually work on knocking down some of those microbes fixing the gut and then really work on repopulating some of the good bacteria after the fact to really work on fixing the gut because you start to fix the gut pH and the gut bacterial milieu that does help improve IgA levels and that does help with the immune system in the vaginal area as well.
Evan Brand: Yeah. Well said. So, if you’re coming in with the UTI, most of the time, there’s gonna be more than just a UTI present. There could be as you mentioned a number of, we have someone coming in and UTI or recurrent UTI is one of their complaints, I can tell you, you and I are gonna wanna run the stool panel and we’re gonna run organic acids because we’re gonna want to look at the whole microbiome and certain things may get missed on the stool and the urine should feel in the gaps like we might find Candida in the urine and it got missed in the stool. So, stool and urine, there are things that your typical doctor and your lab locally is not gonna run. They might run a urine panel but this is not the same urine panel as an organic acid, we’re talking something far more advanced, far more comprehensive whereas the urine panel, locally, is primarily just gonna look for bacteria or maybe leukocytes as you mentioned you might get a positive or a trace or something like that but it’s not a detailed description of what’s going on you mentioned several bacteria too, like Klebsiella and Prevotella, we can identify this on a stool panel. So, that’s why it’s so important to get the data and could we just throw a woman on an herbal UT formula, we could but you know, we want to do our due diligence, we want to do a good work-up on these people too to make sure that we’re not just cut straight to the chase and we skip something huge that we would find on these tests.
Dr. Justin Marchegiani: Right. I mean a lot of the antibiotics they’re gonna be using are gonna be like Bactrim or any of these kinds of, um, Mors, Augmentin’s a big one. Bactrim and Augmentin, those are a couple definitely be very wary of any of the fluoroquinolone families because they have significant side effects regarding tensing tendons and ligaments and mitochondria so be really careful of using fluoroquinolones. Of course, when we work these patients up, we’re doing a really good history so we understand how everything came to fruition regarding the UTI, yeast infection or bacterial vaginosis. We’re trying to understand it, right? Obviously, with certain things like yeast infections, BV, like making sure things are dry in that area. If you’re in a very moist environment keeping things dry helps because yeast and mold love a very moist environment. So, keeping things dry tends to be very helpful. Soaping up some of those areas you’d be very helpful too that you can use a really nice, um, as long as the mucosa is not like really, um, irritable, you can really use a really nice sulfur soap especially in the outside air if there’s anything yeasty on the outside are, anything internally. There are definitely internal things that we can do. So, on the internal side, just getting water in there, maybe helpful using raw cranberry juice, not anything with added sugar but raw organic cranberries, you know, 4 ounces at a time diluted some water is pretty good. You can drink that. That’s gonna have a nice low pH in it, which helps prevent the bacteria from growing. It also helps with some D-mannose in the cranberries. Can also internally do things like different berberines, can be very helpful, that’s excellent boric acids, another excellent compound. You gotta be careful with these by, enlarged by itself because they can be a little bit irritating so you want some nice things that provide some moisture whether it’s aloe or shea butter. There’s different, like moisture compounds that can provide the moisture so you don’t dry out that tissue as well.
Evan Brand: You know, how about some of the suppositories. Have you used those before? I’ve seen some of these like pH suppositories, those have been helpful, also I think it’s integrative, I know Aviva Romm did a talk or an article on it one time. There was a specific probiotic that we had used, I think, it was called pro-flora that we had used, uh, that was supposed to be inserted vaginally and that was like a game changer for BV and some other related issues. So, not only taking oral probiotics but vaginal probiotics as well. That has been a game changer for many women. It’s not something we have to go to a lot but it is a good tool if someone just in bad shape and the conventional strategies failed them or made them worse then something like these vaginal probiotics are helpful. So just to be clear, there’s some strains specifically for vaginal health that are taken orally but then there’s also other blends that you can insert vaginally and the women have reported great success with those.
Dr. Justin Marchegiani: Yeah. You want to make sure the hydration is there, whether it’s aloe or beeswax or shea butter or coconut oil, some of those can be helpful. Again, the antimicrobials that we may use would be the boric acid, some of the neem, some of the different berberines. And again, we may want to also add probiotics in and around there that can be very helpful. In regards to, like yeast issues or, um, UTI issues, you got to be very careful because when you women menstruate, well more with yeast and more bacterial vaginosis because that’s affecting the vaginal canal more. When women menstruate, that blood is like 7.3, right? So, that's very neutral to alkaline. So, when you’re menstruating, you’re taking that acidic pH in the vaginal tract and you’re moving it backup to a more neutral pH when you menstruate so that’s gonna actually make it easier for bacteria and potential yeast to grow and you could have a BV issue or yeast issue that can happen due to your menstruation. So, when you’re already more susceptible in that vaginal area, you know, you gotta, you may actually wanna do a suppository in and around your period too, because that pH is gonna move up and that can start to cause microbes to grow. Some women have to be more careful with that, you know, if they have a chronic yeast or bacterial issue just to make sure it doesn’t come back.
Evan Brand: I want to hit a few more herbs and then I want you to riff on the birth control conversation because I think that’s huge. So, you mentioned berberine and some of the other related herbs. Also, we’ll use the antifungals at the same time. So, you and I have our own custom blends that we use and so we may use something like Pau D’arco, French tarragon, horse tail, olive leaf, things that have antifungal and antimicrobial properties. So, that’s the cool thing about what we do is as you mentioned Backstrom or some of these other conventional strategies. It’s just a big sledgehammer, right? It’s not a targeted tool. It’s one sledgehammer. We don’t know exactly what we’re gonna kill but it’s an antibiotic, were just gonna drop the nuclear bomb into your gut and we’re gonna disturb not only your gut microbiome, we’re gonna negatively affect the production of your nutrients in your gut. We’re gonna negatively affect your mitochondria. We may knock out the UTI but as you saw in the papers, 25% of those UTIs are gonna come back within 6 months to a year and so when we’re coming in with these antimicrobial herbs, also, throwing in antifungal herbs, that’s where the magic really happens because there could be a combination as we talked about. It’s rare to see just UTI, it could be a combination issue meaning there’s some Candida, there’s some bacterial problems, maybe there’s parasites in the gut too. Maybe there’s H. pylori like you mentioned. And so, that’s the fun part is when you take a blend and you’re working people through this protocol. You’re now knocking 4,5,6 issues out all at once in one fell swoop when they originally just came in with the complaint of UTI. When you do the labs, you wanna uncover so much more and that’s where the beauty is.
Dr. Justin Marchegiani: 100%. Here’s one study here looking at the perceptions using contraception birth control pills. So, usually this is like a synthetic estrogen mostly, right, an ethanol, estradiol. I’m looking at the influence on the vaginal microbiota and so really the take home here inside of the gate, the vaginal state was significantly modified hormone administration apparently corrected the alterations uh, but has the potential of being an accurate tool. Where is it? Right here, um, there it is, I’m sorry. Statistically significant association between, this is, um, this is contraception and normal microbiota was observed after three months when the vaginal microbiome was modified at 6 months inflammatory reaction was detected in almost half of the women. So, only seven women but you can, it created an inflammatory state in the vaginal microbiota and then also yeast colonization was increased and it created an inflammatory reaction in three out of seven women and it altered some of the beneficial bacteria in the vaginal area. Now, small study but you can see, you know, three out of seven, it affected this and this is what we see clinically with a lot of our female patients is some of these things can be affected because it’s affecting: one, it’s creation; two, it’s causing yeast to grow impacting some of the good bacteria and how does it do this, it does it mostly via LDH. If you alter someone’s digestive pH, right, let’s say you give them a proton pump inhibitor, you’re gonna have all kinds of digestive issues and maybe even nutrient deficiencies that can affect things long term. Obviously, with birth control pills, there’s other things they do, they can create issues with nutrient absorption or they can cause nutrient deficiencies in areas of B vitamins, folate and also calcium and magnesium. So, we see a lot of women that do birth control pills have a lot of those nutrient problems. So, if you’re on a birth control pill, ideally, it’s better to use something that’s more barrier based or if you want to set it and forget it method, you know, potentially looking at the ParaGard which is a copper IUD, you just have to make sure you can handle the copper. I find if you want to set it or forget that the copper tends to be better than the hormones but ideally, you know, a barrier method it’s not internal all the time. It’s probably better so that just kind of gives you a couple options there.
Evan Brand: Yeah. I’ve heard some stories, some horror stories about the copper ones too. So, like you said it cold be a problem but
Dr. Justin Marchegiani: Not everyone has problems with it. I mean, women that like tend to cramp a lot, they could have, because that cramping, IUD being in that uterus sometimes that can cause pain but it just depends kind of where women are, you know. Some parents may be pushing kids to have a method because they don’t want their kid getting pregnant and maybe they feel like they aren’t responsible enough at maybe 18 or 19 and they set it and forget it method. If you want that, I would recommend doing the ParaGard before you go to a hormonal method.
Evan Brand: Yeah, for sure. And, not to mention too we’re already in a society of so much estrogen dominance and you and I have done podcasts about the impact of gut imbalances in issues with the glucuronidation pathway which is then causing further issues. So, we could see this estrogen problem in a woman who’s not on birth control. You could still see that manifest in this way and so that’s why you’re getting off of the xenoestrogen, you’re cleaning up your makeup. You’re getting rid of plastics. You’re fixing your gut. You’re improving detoxification. All these other functional medicine strategies are directly impacting your ability to beat this situation. So, we know, we always want people to look at the big picture. Don’t just look for the magic, uh, like, berberine, Pau D’ Arco remedy. And there’s a question here in the chat, ‘how many Pau d’ Arco capsules is needed for someone who has Candida in their gut?’. I have no clue because we rarely use it in isolation. We’re always gonna use it in a blend. And I doubt you have just Candida. You’ve probably got other issues too.
Dr. Justin Marchegiani: Yeah. Somewhere when they come in, they could have a combination of a little bit of a bacterial, a yeast issue, UTI thing. That could be a kind of combination of 2 or 3 different things happening. This one may be more predominant. So, we never wanna just go all in on one thing. Again, if someone’s having vaginal issues specifically, there’s gonna be things that we insert intravaginally like some of the boric acid, like some of the neem or the berberines and we’ll probably interchange in some probiotics because part of the big problem is you have to get the bacteria flora in the vaginal area, back up to where it should be because it’s the good bacteria that will help keep the other bad bugs in check through their natural acid and hydrogen peroxide production.
Evan Brand: Well said.
And so, the point I was making is that I don’t want people listening and going okay just give me the freaking remedy. What’s the natural urinary tract remedy? That’s what I’m here for. And we’ve talked about some of those, you know, the mannose, the cranberry, the berberines, the Pau d’ Arcos, the French Tarragon, this whole blend, you know, that may be the solution but what got you here is important. Have you fixed the other issues that have gotten you here. And so, I hope people see the big picture. Sometimes, you and I are happy to just go boom, hit the oregano oil and were happy to just throw out just this natural solution but like you said before we hit the record, you don’t want people skipping out on the low hanging fruit.
Dr. Justin Marchegiani: Exactly. And so, it’s always good to do history. I find the big issue is antibiotics can be a big factor. I also find just some of the low-hanging fruit like the intercourse and hydration can also be a big factor as well. You’ll be surprised. And so, my wife comes to me, she’s like, ‘my friend has this issue, what should I recommend?’. Well, it’s hard, I can’t really recommend a lot of things because I don’t know much about them if eating like crap and they’re not hydrating and they’re drinking lots of soda and they’ve been on lots of antibiotics, you know, I may say, hey, all right, do this [24:34] but that’s gonna be palliative and not fix the whole lead up and how everything went down. And so, the lead up and I call it the timeline history of how we get to this point matters so much because, you know, if not, you were just becoming naturopathic doctors that are using nutrients and herbs like MDs use drugs. Now, again, I think that’s better because a lot of these things are natural, have less side effects but still we want to be holistic and still root cause.
Evan Brand: Yeah. Well said. That’s the problem. There’s a difference between naturopathic approach to this issue and functional medicine approach to this issue. So, I think you made that clear, which is, you go to the naturopath, it’s hey, here’s the oversee, functional medicine is gonna come in and say, ‘okay, well, how did you get to the UTI?’. Oh, you took antibiotics, you’re on birth control for 20 years, you had a sexual partner who had extremely poor microbiome health, maybe there was some issue there, maybe you had multiple partners, maybe one of them had H. pylori. You have low stomach acid. You ended up with dysbiosis, then you got Candida overgrowth, then you drank too much alcohol, you loved to do wine in the evenings. You ate a little too much chocolate, you know, it’s like, that’s the more investigative route and that’s where people need to be thinking. We’ve got friends that are naturopaths, good people, but you just got to go deeper most of the time.
Dr. Justin Marchegiani: Yeah, and a lot of times too, if I'm, if someone has chronic issues, I wanna know more about their gut because the microbiome has such an impact especially with IgA and with the overall immune system. So, if there’s chronic issues in the vaginal area, you have to look up to the intestinal tract. Very important.
Evan Brand: Yeah, and you would say there’s gotta be some link between the low secretory IgA that you and I are seeing on the stool test and what’s going on with the vaginal microbiome too, right? You would assume that’s a system-wide defense shield that’s gonna be affected.
Dr. Justin Marchegiani: Yeah. It’s part of the mucous membrane barrier. So, mucous membranes in the eyes, the mouth, the intestinal tract, the urinary tract, the vaginal canal. So, if we see low IgA issues in the intestinal tract, that barrier is a little bit weaker. Think of the force field, you know, you see star trek, they put, like their force field up, right, so they, so when the Klingons go to shoot them, it kind of bounces off, right? Think of the force field we have in our intestinal tract and our vaginal canal and our urinary canal that kind of protects and so probiotics can help, obviously getting rid of the dysbiotic microbes can help, avoiding a lot of things that create the imbalances to begin with, which would be a lot of the antibiotics or maybe pesticides or GMO foods that produce a lot of antimicrobial compounds too. All those help avoiding those things too.
Evan Brand: You know, what’s happening even in the functional medicine world, is that everything’s becoming isolated. Are you noticing that? Like people are focusing on just the gut. So, it’s like this leaky gut formula, this leaky gut protocol and they’re ignoring the fact that you just mentioned this IgA, this mucosal barrier is kind of a system-wide problem. So, there could be oral, vaginal, gut all at the same time, all related to the same dysfunction of these force fields being down. I think it's just marketing, right? People just want to market that they’re the gut guy, they’re the parasite guy, they’re the Candida guy. I think that’s just a marketing probe but hopefully people are seeing this and of course if they’ve been listening to us for months or years, they’re seeing that this is a system-wide problem, it’s just manifesting in this way.
Dr. Justin Marchegiani: Yeah. In the functional medicine world, a lot of people market to niche areas and symptoms which is fine because a lot of people when they get focused on something, they think they have these issues, they’re going into google or they’re typing that issue. So, for you to be relevant and for that person that has health issues to find you, you do kind of have to market to a symptom but then when you find that person and you talk to them, you wanna make sure that their approach is globally where they look at things holistically and you’re not seeing the gut person that only deals with the gut and they’re not looking at your thyroid or your anemia or your low glutathione. They’re not connecting the dots. So, you got to make sure they’re still able to connect the dots but multiple systems and they’re not just focused on one issue. So, it’s okay for doctors to market to that, you just have to make sure that their philosophy is a holistic philosophy that encompasses everything in there.
Evan Brand: Yeah and holistic spelled w-h-o-l-e a wholistic, the whole thing, the whole body, the whole person, not just holistic as in natural, it’s gonna be the whole piece and I think that’s where I suffered for a long time because I focused on my gut for so long but I was ignoring toxicity issues, I was ignoring dental issues, I was ignoring tick bite infections. So now, oh crap, I see the whole picture and I would miss that if I just dialed in the gut so and that’s what you and I do. We’ve done this over with clients worldwide, we look at the whole picture. If you’re suffering, if you’ve been through the conventional rabbit hole or maybe you’ve been fortunate to avoid the conventional rabbit hole, you don’t want to go down it but you need help, feel free to reach out. Dr. J and I work with people around the world. We can send these labs that we’re talking about stool and urine. These are at home, these are non-invasive. It’s rare that we need to do invasive testing but most of the time it’s at home functional medicine tests can be sent to your door, you do them, you send them back to the lab. We get the results. We jump on a call. We run you through them. We interpret those. We make a protocol for you and get you better and get you off the merry-go-round. So, if you need help, feel free to reach out, Dr. J is at justinhealth.com and me, evanbrand.com and you can reach out, book a call with us, we’d love to talk with you, help you, find and fix the root causes if you just have UTIs and you think that’s all it is, maybe you’re right but maybe not, either way, we’re gonna help you get to the bottom of it.
Dr. Justin Marchegiani: Very good. Excellent. So, for women that are listening and kind of want to recap here, first thing, make sure your diet is right, keep in the process refined sugar, grains, flours out, makes a huge difference. Omega-6, seed oils, in general, should be reduced as well. Hydration, make sure hydration is good, clean and filtered water, um, you know, good mineral water, especially if you have more health issues, more minerals in there is gonna be better. Next thing out of the gate, you know, urinate after intercourse, those kinds of foundational things. If you have chronic gut issues, definitely, get your gut looked at. If you’re on hormone, if you’re on birth control pills, definitely get your hormones looked at and figure out why you’re on them. Most women aren’t even on hormone or birth control pills for birth prevention. They’re on it for off-label issues like acne or headaches or lots of PMS and so most women could totally get off it because they’re not even using birth control pills for the original intention. They’re for off-label use and so that would require looking deeper at the hormones. Next, you can get tested, you can do either a, um, a MONISTAT test to look for yeast, you can get those at the drugstore, you can do one of the strip tests to look for leukocyte esterase or I think it’s nitrites in the urine for more of the UTI issues and of course, if you have a lot more of the odor-like, uh, issues, you can get a vaginal swab from your OB or your primary to rule out any of the BV issues as well, again, similar solutions, you know, some maybe more internal in regards to what we recommend, some maybe more internal like with swallowing pills so maybe internally, intravaginally and of course the more chronic the issue is, the more we have to really support the vaginal microbiome with the right beneficial bacteria getting in there internally as well. And then, of course, just keeping up with a lot of the menstruation because that can really affect a lot of the, um, the bacterial issues and yeast issues in the vaginal canal because it’s gonna shift that pH from very acidic to more neutral to alkaline at that time of the month when you menstruate. So, hopefully, that’s a good kind of crash course, out of the gates and kind of you guys understand kind of our spitball kind of philosophy and how we look at the whole history and really connect the dots and we have our little toolbox of all these things but we just got to make sure it’s catered to the history.
Evan Brand: And alcohol too, I think, we briefly mentioned it but alcohols got to go. It’s just, it’s not gonna help you. It’s going to promote all sorts of issues. It’s gonna aggravate the immune system. It’s gonna affect your IgA levels. It may promote dysbiosis and it may promote more yeast problems and so I’ve heard many stories where a woman’s like, oh yeah we went to Napa Valley and we drank wine and ate chocolate and salami and cheese all weekend and now I had a flare up. It’s like, well, yeah, duh, I mean, that’s incredibly damaging. Everything that you’ve done, you binged on wine all weekend so I think wine kind of gets like this people think that they’re not drinking alcohol. Somehow, they think they’re getting off the hook. Oh, it’s just wine, like, it’s so socially cool, it’s like coffee. It’s like coffee and wine, like wine is so accepted into the culture but it can be a big problem, I tell you. Some of those California women, the ones in San Francisco, like, it’s part of the culture here. I had one woman argue with me that she didn’t want to get off alcohol. I said, well, what if it’s gonna help your gut. She’s like, well maybe I’ll consider it. So, sometimes as practitioners, we’re having to bargain with people and try to make trades and make healthy swaps, we’ll swap it for this and try this and what if you do a binder afterwards. So, sometimes, you gotta work with people, they’re not just in a vacuum. We got to work with them and help educate them so that they’re more dedicated to the lifestyle changes but I just want to mention alcohol because I think a lot of people, don’t even consider the impact it has on the gut but then on this flora.
Dr. Justin Marchegiani: Yeah. A couple things with alcohol, number one it’s diuretic so it will increase the frequent urination and kind of make you more dehydrated so good hydration helps prevent a lot of that bacteria from growing. Number two, out of the gates, you know, it may be necessary out of the gates for the first month so as you get things under wrap. There’re also healthier versions of alcohol. I mean, you can always get, like a Cosmo martini that has the fresh lime juice in there and cranberry juice. Just make sure it’s, like not the cranberry with sugar or the lime with sugar. Make sure, it’s fresh lime or actual juice cranberries with, like a nice Tito’s vodka, I mean, Tito’s vodka is, um, it is charcoal filter, right? So, it’s gonna be really clean and you can get some nice cranberry and lime in there that should be almost be beneficial in a way, obviously, you know, keep it, you know, a drink or two maybe once or twice a week max but once you better that maybe a good option to add things back in and just stay away from a lot of the sugary stuff and of course the glutinous drinks and you’ll be in a lot better position.
Evan Brand: Yeah. It’s a funny thing you have to mention. There’s got to be real cranberries because most of the time you go to a bar, it’s like that. It’s garbage. The heart or it’s the high fructose corn syrup concentrate.
Dr. Justin Marchegiani: Yeah. So, worst case, you can always just do a fresh lime squeezed in there and see if they have anything that’s just a pure, you know, extract and that’s a much way to do it. Of course, dry or white wines and you know just a good Tito’s vodka is always great with just the lime in and of itself. That’s an easy way to do it and keep the sugar and junk down but also keep a nice acidic pH there which is helpful for the vaginal area.
Evan Brand: Yeah. We’ll hope, as you mentioned, no I think we covered It so if you need help, we mentioned the links here Dr. J, that’s Justin at justinhealth.com. You can reach out for consult worldwide. Me at evanbrand.com, either way, we’re here to help you guys. We love what we do. We have a blast and it’s fun to educate people. It’s fun to empower people and take back your health and it’s possible. Whatever you’re dealing with it’s possible to make progress so just keep your head up. Stay motivated. Don’t always run straight to that antibiotic if there’s another way. You may try another solution. If you’ve been doing this for a decade now and you’re still battling it, you’re not out of the woods yet, it’s time to look deeper.
Dr. Justin Marchegiani: Excellent. Great chat, Evan. Everyone, have an awesome week. We’ll talk soon. Take care of you all.
Evan Brand: Take care, now.
Dr. Justin Marchegiani: Bye now. Peace.
Evan Brand: Bye-bye