
In this video, Dr. J and Evan stress the importance of what you eat and how it impacts the rest of your body. However, what you might not realize is how your food is digested in your body, and when it gets inflamed and leaky, how do you fix it?
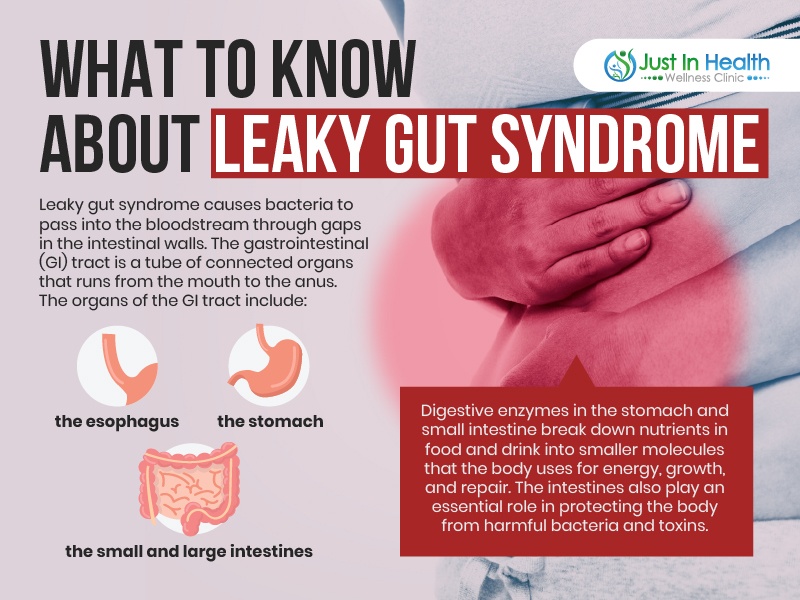
A lack of digestive enzymes can cause leaky gut syndrome—another unfortunate result of chronic inflammation in the digestive system. Many culprits cause leaky gut, including stress, medications, poor food choices or quality, alcohol, cigarettes, and even hormone changes.

Dr. Justin Marchegiani
In this episode, we cover:
0:00 – Introduction
1:08 – Poor Gut Health Connection to Virus.
4:31 – What is the role of bile movement and production?
11:16 – The influence of gut michrobiota on Inflammation and Insulin Resistance
19:29 – General recommendations on carbohydrates and for a healthier gut
Dr. Justin Marchegiani: Hi! Dr. J here in the house with Evan Brand. Today, we’re gonna be talking about the signs and solutions of gut inflammation and gut permeability or leaky gut for short. Really exciting topic. We see it a lot in our patients every single day. Evan, how are we doing today man?
Evan Brand: Hey. I’m doing really well. I can’t remember if we covered this on the podcast or not, this specific study but there was a paper that came out all about leaky gut and worsen outcomes with the virus and so people could put in the, you know, what virus in PubMed and leaky gut and we’re finding that a lot of people with leaky gut that’s actually one of the precursors and that’s what’s leading to worse outcomes so this is more important, It’s always important but this is more important now because we know that there’s a massive link and I’ll actually pull this up here and I’ll show you this, American Society for Microbiology, they did this. Did we talk about this yet or not?
Dr. Justin Marchegiani: Let’s talk about it. Let’s go ahead.
Evan Brand: This particular paper. Let’s bring it up there.
Dr. Justin Marchegiani: Let me check here. Oh yeah. Let me add it on. Go ahead.
Evan Brand: Yeah. So, there we go. So, poor gut health is connected to severe blank, new research shows and long story short, you can go into this microbiology article but long story short they actually show a picture too. Let me see if I can get to that picture. Here we go. That was the picture. I think, we already showed this picture but forgive me and people listening on audio. Basically, we’re just showing that viral particles with a leaky gut are gonna be able to get into the circulation and that’s gonna increase your inflammatory response so the real goal of today is making sure that your gut is in good shape because therefore you’re not gonna have leakage into your circulation. You’re gonna be far far better if you have that healthy gut barrier. So, that was really kind of the spark notes of that but that’s like a 19 pages paper that you can dive into and many people I think have thought of leaky gut as kind of trendy topic that only people like you and I talk about but this is finally, actually getting into the mainstream. So, I hope gastroenterologists are gonna realize the importance of addressing the gut and I hope they actually start taking it more seriously. Right now, it’s just antibiotics that’s really the only thing that gastroenterologists do for gut, right? I mean steroids maybe and immune modulating drugs in the case of like, ulcerative colitis and Crohn’s but beyond that there’s not really much leaky gut conversation going on.
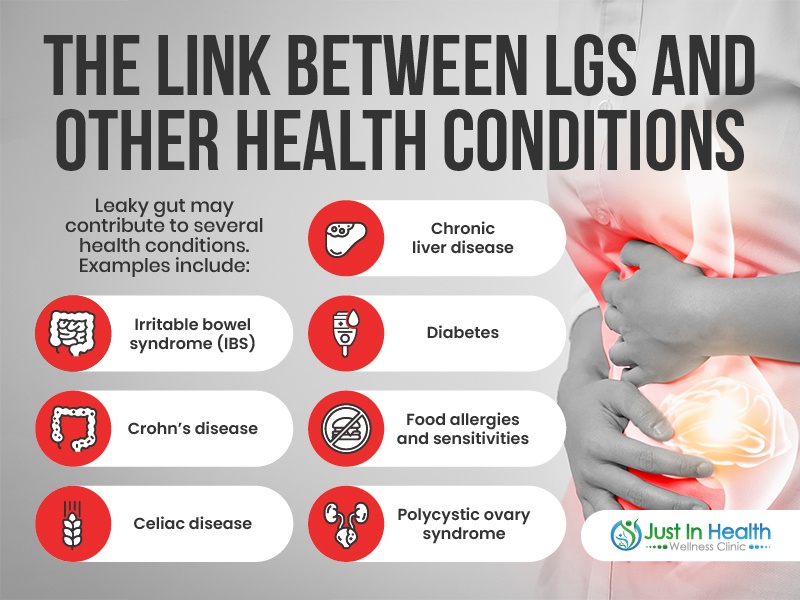
Dr. Justin Marchegiani: No. There’s not and again, really, a leaky gut has an effect, right? Or we’ll call it gut permeability, right? If you go on PubMed, a leaky gut is like a slung. If you want to really find it, you want to look at, you know, gastrointestinal permeability, right? These are gonna be the big things, it’s the tight junctions, the epithelial cells and the small intestine, they start to come apart like my fingers here interlocked like I’m saying a prayer, they come apart and then you can see lipopolysaccharides undigested food particulate can slip out. So, this is, um, this is part of the major, major mechanism. Now, with gut permeability, it’s an effect not a cause so I always tell patients, we don’t go in and treat leaky gut, we treat the corresponding vectors of inflammation that drive gut permeability so that could be food allergens, that could be immune stressors like virus, parasites, small intestinal bacterial overgrowth, general dysbiosis, poor digestion, antibiotic exposure, creating rebound overgrowth, fungal overgrowth, you know, just poor digestion, lots of stress, increased sympathetic tone and adrenal stress, that’s shutting down the digestive system and making gut permeability more probable. So, these are the big vectors so we always wanna draw a line. What’s the root cause and what’s the effect and gut permeability is in the effect not necessarily a cause.
Evan Brand: Yeah. I’ve seen a lot of, even advertisements now on social media for all these leaky gut healing formulas and that kind of stuff and it always has the word heal involved but you could take as much glutamine and whatever else you want. You could go into an elemental diet and all of that. It’s not gonna get rid of these big root causes and certainly for me, I tried some gut support but ultimately it was resolving my parasite infections. That was the most important thing for me and so, you can test for this. This is not an uncommon situation; you and I personally and clinically see parasites every single week. So, when you hear this idea of like, oh, it’s a third world country problem, you haven’t traveled to Mexico or anything like that. That’s just crap, I see it all the time and I had them and I was not out of the country and I had multiple parasite infections and then that affects your bowel flow, right? Can we talk about the bowel for a minute, what’s the role there, because you and I talked about how you have to have adequate bile to act as sort of a natural antimicrobial but how is this happening. What do you think are the big driving factors for why bile production is just not good?
Dr. Justin Marchegiani: Well, first off, we look at the domino rally of digestion. The first thing that has to happen is good, nice aesthetic pH in the stomach. So, we need adequate HCl in the stomach, hydrochloric acid that lowers the pH and again, lower pH tends to have an antimicrobial effect, right? So, if we have to bring the pH down a little bit, that makes it harder for bugs to grow and that pH is also responsible for activating a lot of proteolytic enzymes in our stomach so if we have a good pH, we activate our enzymes, that starts the digestive cascade, we make it harder for bugs to grow and then once all that kind that mixed up food and enzymes and acids and all the stuff in our stomach is all mixed up. That’s called chyme, C-H-Y-M-E, that gets released into our small intestine, our pancreas then produces a bunch of bicarbonate to bring that pH back up to around neutral but that pH being nice and acidic, it triggers bicarbonate and then it also triggers cholecystokinin production, CCK, which then causes the gallbladder to contract so then you get a whole bunch of bile that comes out, you get a bunch of bicarbonate that comes out of the pancreas but then you’re also gonna get a bunch of lipase and proteolytic enzymes, trypsin, chymotrypsin lipase, lipolytic enzymes is coming out of the pancreas as well. So then, you bring the pH back up, you add the fat digestive enzymes, the proteolytic enzymes and then you also stimulate that bile production which then emulsifies that fat. Think of emulsification as you have a nice greasy pan where you cook some bacon on, right? Throw under water, you feel the fat on the pan, throw some dawn soap on there, it emulsifies it. It breaks that up so then you can get it all out the intestinal tract and be able to absorb it, carry on, mycells and be able to use it for lipid bilayer, hair, skin, nail, energy all that stuff. Prostaglandins.
Evan Brand: Yeah. Well said. And though bile is produced by your liver but it’s stored in your gallbladder so people that have had their gallbladders removed which is a very common surgery, a lot of surgeons are very happy to remove gallbladders, I think in many cases, they may have been saved with fixing these other upstream issues but, well, once it’s gone, it’s gone. So, people listening that have no gallbladder, you have to take that into consideration. There was a study here in 2018, it was in the annals of gastroenterology, it found that poor bile flow can contribute to the development of inflammatory bowel disease. So, you’re really setting yourself up and find all the time with people clinically when they come in, they’ve had gallbladder removal, we see a lot of issues, we see massive bacterial overgrowth problems in these people and I think that’s partly due to not having enough bile being stored anymore like you and I have talked about it before, I think you said it was a 10x concentration in the gallbladder, is that right?
Dr. Justin Marchegiani: 10 to 15x. Yeah.
Evan Brand: So, you’re missing out on that when you have just liver production, you don’t have that storage facility. I mean you have some but just nowhere near what you would have had if you had your gallbladder. So, please. Try to save your gallbladder. You got to fix these upstream infections because that’s gonna be and get off proton pump inhibitors with the help of your doctor if you can because we know that, that suppression of stomach acid is gonna lead to the overgrowth which then fuels these downstream issues to not happen the domino effect, it literally gets stopped or prevented by the PPIs.
Dr. Justin Marchegiani: 100%. And so, we need good, think of bile, it’s an emulsifier, it breaks down fat, it’s also an antimicrobial and so we create antimicrobial environments by having good, nice, low pH by having good enzyme and acid levels that also helps and then also by having good bile output and plus the longer that food sits there and rots and putrefies because we are not breaking it down into its constituent parts, right? Then it’s gonna create future petrification, fermentation, and rancidification. Essentially proteins and fats and carbs are rotting, right? Then you can get gas and bloating and that just creates this incredible breeding ground for bugs to grow. It’s like you can have this beautiful home that you take care of but if you leave the garbage in there like, a week too long it’s gonna get like, stinky and then you’re gonna get a whole bunch of bugs attracted to it, right? Same kind of thing in our microbiome so it’s really important that we stay on top of, you know, those good health practices.
Evan Brand: Let’s hit the symptoms and signs and symptoms because people know most of the gut ones but there are some that you and I find clinically that maybe people wouldn’t think are a gut symptom, right? It might not manifest outside of that so we can cover the stuff like unusual color texture, smell, messy poops, you have floating stool. You have maybe alternating diarrhea, constipation, bloating, gut pain. But, what about like, skin issues and what about anxiety and depression and hormonal imbalances and brain fog. I mean, you and I have seen, we lost count how many times we’ve seen cases where we simply just fix the gut and all the sudden, this depression is lifted. I had one client named Miranda, who she had been depressed for, she said quote 20 plus years, all we did is do a gut protocol. I gave her no antidepressant herbs. We simply just did a gut protocol and when we did a six-week follow-up, she said her depression was 90% better and when she said 90% better, she didn’t even sound too excited and I said, are you realizing what you just said to me. You’ve been depressed for over 20 years and you’re 90% less depressed in six weeks of doing a gut protocol like do you realize how profound that is and she goes oh yeah, I guess that is amazing. Thank you. And, I think people, they get so used to feeling a certain way that when the clouds lift. They’re almost not even ready for it but depression, anxiety, I would put at the top of the list for mental health issues connected to these gut inflammation problems, I will tell you. And, you and I discussed this I remember calling you one-night years ago is probably like coming up on be six, seven years ago was like 2014, 2015 and I was like man, I’m having like a panic episode or something and this was when I was living down in Austin and it was H. pylori. It was driving that because as soon as I cleared the H. pylori, all those weird episodes of panic completely disappeared and I’ve seen that more than just the n equals one, me, I’ve seen it many, many times. So, if you have anxiety problems, you go to the psychiatrist. They’re not going to suggest you have gut infections but that’s something you need to be thinking about.
Dr. Justin Marchegiani: 100%. Yep. 110% for sure. Anything else you want to add in that topic?
Evan Brand: If you’ve got mental health issues, look in the gut maybe even look in the gut before you look in the brain. Now, obviously, we’re gonna be doing organic acid testing and other things to look at neurotransmitters so we’re gonna check out dopamine, serotonin. We’re gonna look at what’s called quinolinic acid so we can look for actual brain inflammation or brain toxicity related to gut infections like sometimes Clostridia, we’ll see will drive up the quinolinic acid markers but we still have to fix the gut. So, if you have a family member, they’re anxious, they’re depressed, they’re fatigued. We’ve seen a massive link between chronic fatigue and gut infection. So, there’s another big one that people may not recognize, the gastro doc may not suggest your chronic fatigue is from a gut infection but it certainly can be skin issues as well. My skin was a wreck years ago. I had major acne even though my diet was clean. It was my gut.
Dr. Justin Marchegiani: Totally. I also wanna highlight one other kind of variable here. I think it’s really important. I’m gonna pull this on screen here. I think this is really interesting. So, an interesting abstract here and it’s looking at the influences on the gut microbiome on inflammation and insulin resistance so this is interesting because we talk about insulin resistance, right? Consuming too much carbohydrate and refined sugar. All carbohydrates get broken down typically into glucose, fructose or a combination of the two, right? And so, the more sugar that gets released into our bloodstream that gets broken down whether from refined sugar, sucrose which is fructose in glucose, high fructose corn syrup is fructose in glucose 55, 45 concentration and then of course we have starches which get primarily broken down into glucose and then we have fruit which is more on the fructose side. These things all have an impact on our blood sugar and the more insulin resistant we become, we, it drives inflammation. It’s hard to utilize these fuel resources and these fuel sources to get deposited in our fat because our muscles don’t have the ability to store it. our liver loses the ability to store it. We don’t have the activity level. We don’t have the mitochondria stimulation to burn it so we store it as fat. Now, this article is interesting. It talks about obesity as the main condition that’s correlated with the appearance of insulin resistance. Think of this as when your cells get numb to insulin. Now, this is on screen here. People that are looking if you’ve got mental health issues on the audio version, we’ll put the link below for the whole video. Whole bacteria, their byproducts and metabolites undergo increased translocation through the gut epithelium. Translocate, let me give you the translation on that. Here’s your gut. Leaky gut happens, right? Where it talks about gut permeability and things start to translocate meaning move from the inside of the gut back into the bloodstream, right? So, it translocates through the gut epithelium into circulation due to the degradation of tight junctions. This is a leaky gut, right? Here. And it increases intestinal permeability that culminates in inflammation and insulin resistance. So, what this says is the inflammation caused by gut permeability caused by gut permeability caused by lack of enzymes, bile, food allergens, all the gut microbiome issues can actually drive inflammation and insulin resistance. Now, it makes it harder for your mitochondria to generate fuel because you’re not able to get that fuel into your cell and you start to become more of a sugar burner. It’s very difficult to burn fat when you have high levels of insulin, Very, very difficult. So, several strategies focusing on modulation of the gut microbiome using antibiotics, again, we would use antimicrobial herbs, probiotics and probiotic fibers are being experimentally used to um, in order to reduce intestinal permeability, increase the production of short chain fatty acids. Guess what, things like butyric acid, medium chain triglycerides. Those are all very helpful. And again, this helps promote insulin sensitivity and counteracts the inflammation. So, really, really important here. This study, influence of gut microbiome on subclinical inflammation here and this is the 2000, see what’s the study, 2013 study so we’ve known this stuff out for a long time here that the gut microbiome plays a major role on your blood sugar, blood sugar handling and if you’re a diabetic or someone with insulin problems, you need to be looking at the gut. Yeah. look at the diet, look at, you know, getting your diet and your macros in order, make sure your food quality is good and then look at really getting the microbiome dialed in to really help. That could be a missing piece of the puzzle for people that have really changed their diet but not quite gotten the metabolic benefits of losing weight yet.
Evan Brand: Wow. That’s a good point. You know, when I think back, when I had gut infections, my blood sugar was definitely not as good. I mean, 2 to 3 hours is as far as I could go without having to eat a meal. Now, I could fast all morning and not eat till 1 pm and I’m perfectly fine. I think there is an adrenal component too. I think I’m in a lot better place with that but I can tell you that certainly after mixing my gut, my blood sugar and blood stability is much better. So, I think you’re onto something with that paper and how people that even have gone paleo or animal based or keto. That still has issues with blood sugar regulation. That could be a sign of gut issues and I think even If diet dialed in in some cases what like you’re showing here, there could still be issues with the blood sugar. So, sometimes, it’s portrayed as like just fix your diet and everything else falls into place but you have to consider these other factors and also, I’ll throw in at the, you know, 11th hour here, mycotoxins, we know that mold toxins significantly affect the gut barrier and create a leaky gut. They damage the mitochondria, and we know that certain mycotoxins promote the overgrowth of bacteria like Clostridia and Candida. In fact, the lab will tell you that on paper, for example mycophenolic acid, it's a very common mycotoxin that we see that comes from water damaged buildings. You breathe that in, that’ll then affect the gut and allow the overgrowth. So, if you’re just treating the antimicrobial herbs or fungal herbs and you’ve missed this giant mold exposure that can still affect the gut, still affect the brain and people won’t get fully better. So, that’s really the beauty of what we do is we try to work through all these puzzle pieces and help you because you could have this guy who says everything is gut and you go all the way down this gut rabbit hole and not get fully better or you go all the way down this insulin resistance rabbit hole and you still miss the smoking gun. You got the leaking dishwasher and your whole kitchen cabinetry. We had a woman in Texas last week, her dishwasher apparently leaking for years. Her entire kitchen has to be replaced now. She’s looking at 25k, just to replace her whole kitchen and she’s been to 10 doctors, 10 practitioners and nobody’s figured it out and I’m not trying to toot my own but I’ll just say I kept suspecting something because she said that she would always feel weird while she was washing dishes at her sink. She would get a little bit of a headache, feel a little bit sick to her stomach, said, ‘huh, is it possible that something’s leaking?' and then boom brought in the remediator and they found it. There was a leaking dishwasher black mold everywhere.
Dr. Justin Marchegiani: Yeah. Mold plays a major role in stressing out the immune system. It can create gut permeability within itself and then obviously drives the insulin problems. And also, people that eat this type of diet, I mean, it’s natural when you have microbiome issues to create a bunch of sugar because these foods are from an evolutionary standpoint, things that had a lot of sugar in it ended up having a lot of nutrients in it, right? Oh, a bunch of berries, some honey, right? And they were very rare in society. It was hard to find a lot of these things. Even fruit, you know, back then, tended to be a lot more sour and bitter and we’ve kind of hybridized and you know selectively grown fruits that tend to be sweeter and more, uh, and more plump and luscious now they taste. And so, we have sweeter fruits today and so it’s natural for people to want to crave all the crap that feeds the bad bugs because the bugs are producing chemicals to make you crave these foods. So, you have to be educated and understand that these foods, even though you’re craving them, you need to like not listen to those cravings sometimes and really shift your gut in it. If it shifts your macronutrients in a way to starve out some of these bugs, it can make a big difference.
Evan Brand: Yeah. Well said. I mean, a lot of fruits hybridize now too as you mentioned to be sweeter, so like a strawberry. I’ve seen strawberries as big as my hand sometimes, like, ‘God’, you know wild strawberries, they’re tiny. I mean they’re like the size of a fingernail, if you’ve ever seen wild strawberries out in the yard, very tiny and definitely not anywhere as sweet as the other ones. So, when you hear people talk about fruit, like our modern fruit, like you said it’s not really, it’s more like candy with some, it’s like natural candy as opposed to the more ancient fruits so If I can find like some heirloom apples and that kind of stuff, I’m totally into it.
Dr. Justin Marchegiani: Exactly. And you know, my general recommendation with carbohydrates, just make sure you earn it, make sure you’re not in a place where you’re inactive and try to get some activity because sugar goes three directions: gets stored in the liver and muscle, okay, so, if you’re working out, you’re always draining that muscle every day, you have a storage reservoir for it a little bit in the liver; It goes to fat or it stays in the bloodstream and gets burned up by the mitochondria essentially. It gets burnt up mitochondria-wise by the muscles etc. So, it’s gonna go either stored, burnt, you know, it'll stay in the bloodstream but burnt up by the muscles of mitochondria or it gets converted to fat. So, if you’re doing things that allow you to utilize the glucose in that bloodstream, not as big of a deal, but that’s what you really have to look at what activity level is and you have to work with your functional medicine doctor about dialing in those macros and some people they need to starve out certain macros especially the fermentable carbohydrates and a lot of the inflammatory foods especially grains, legumes, dairy. Those things are really, can be, drive a lot of inflammation and that can keep your sympathetic nervous system and your immune system on high alert which just drains a lot of energy from you. Food allergens can make you fat and they can drain energy from you. Yeah. Seeds too. You know, I cut out almond seeds, nut seeds. Yep, even some eggs too for sure.
Evan Brand: I cut out eggs for her while greens, I mean, some people are way overdoing it on the leafy greens. I can’t tell you the last time I ate a salad. I don’t really care. I don’t do leafy greens. I used to but, you know, I see way too many people doing these like kale smoothies. I had a lady doing like a pound of kale a day. Oxalates were off the chart. We know those affect the gut barrier too so there are downsides to plants.
Dr. Justin Marchegiani: Yeah. I mean, it’s all about, you know, how you tolerate it, can you eat and feel good afterwards, how does your stool look? Do you see a bunch of undigested particulates? If so, you may want to work on just chewing your food up more. Taking some enzymes. See if that helps or sauteed it a little bit and see if that moves a needle. Again, there’s almost always a way, we can adjust things so it works but everyone’s a little different.
Evan Brand: If you need further help, you can reach out to Dr. Justin at his website, justinhealth.com. Now, we do worldwide consultations, phone, facetime, skype, whatever it can connect to, we do it. Lab tests are sent around the world. It’s awesome we have distributors to work with. We can get these things to your door. We sign off on it and get you rolling so we can investigate and look deeper. So, justinhealth and then for me Evan Brand, it’s evanbrand.com. You can reach out and we’re both happy to help you. We love what we do. We’re very blessed for the opportunity to be in the trenches. We’re always improving our own health. We work on our families, our children. We work on everybody around us. We’re always trying to improve them and to be able to do it clinically too is just great. We learn so much from you all and we like to be the shining light in a world of darkness where people have been to countless practitioners and the stuff that to you and I is just common everyday conversation, functional medicine stuff. This stuff to some people is like wow why has nobody ever mentioned that to me before. And for us, it’s like, oh yeah uh-uh, we do it with everyone. So, we look forward to helping you uncover your root causes if you have gut inflammation, what’s going on. There’s something under it so don’t give up, keep pushing forward and please reach out if you need help. We’d love to help you.
Dr. Justin Marchegiani: Yeah. Evanbrand.com, work at Evan. Dr. J, justinhealth.com, works with me. We are here with you guys. And, put your comments down below. Let us know the different things that you guys are applying, what’s working, what’s not and if you get overwhelmed listening to this. Try to take at least one action item out of it. I would say action items from a supplement standpoint. We’ll put our recommended supplements down below. We have different hydrochloric acid and enzyme support products that we’ll put down below for links. That’s always low hanging fruit. Again, diet wise, you know, a good autoimmune, lower fodmap diet can really be a good starting point and I would say for liver gallbladder, you know, we have our different formulas. I have one called liver supreme and again some of the hallmark nutrients in these products are gonna be bile, phosphatidylcholine, taurine, some products will have things like Tudca, which can be very helpful for biliary flow. Beetroot can be really helpful. if I didn’t mention Ox Biles. These are all maybe some milk thistle, very supportive for liver, gallbladder function, liver-gallbladder flow. So, very beneficial, we’ll put the links down below so if you guys enjoy the information and you wanna take action feel free to take a look at some of those links and support the show by grabbing some of those products and Evan will have his links down below as well. Anything else, Evan, you wanna add?

Evan Brand: I think, I said, we give people the links. Make sure you subscribe to the podcast if you’re listening on apple that’s probably where most people find us if you’re looking up. Justin’s show, make sure you subscribe there or my show, Evan Brand. We don’t care how you’re listening, you know, obviously we cross pollinate. We put these on each other so make sure you’re subscribed to both of them so you don’t miss it and we appreciate it. give us a review too. I think we should probably do a giveaway. I know some people giveaways so we can give away a book or you know free supplement or something but, in the meantime, give us a five star review on apple, we would love it. That’s how we stay up in the rankings so that we can actually share true functional medicine education to the masses because right now there’s still a lot of people that are in the top charts just theory. They’re not clinicians. They’re not in the trenches every day, all day, I mean we look at an exhaustive amount of lab testing that helps us to really dial the stuff we’re saying in. We then sprinkle in some studies and we stay up on the research but you could keep your head in the research all day and totally miss what actually works and it’s all about what actually gets people the results. So, keep that in mind and make sure you subscribe. Give us a review on Apple, we’ll love you forever. Thank you.
Dr. Justin Marchegiani: 110% All the links will be below for you guys. Alright, thanks a lot. Evan, great chat with you man. Have a good one. Bye everyone.
Evan Brand: You too, take it easy. Bye-bye.
https://justinhealth.libsyn.com/signs-and-solution-for-gut-inflammation-and-leaky-gut-podcast-351