
By Dr. Justin Marchegiani
Iodine and Hashimotos thyroiditis are two very controversial yet very popular areas of discussion in regards to the treatment of hypothyroidism. Most people who hear of someone suffering from low thyroid symptoms will think of iodine as the first magical solution. Iodine is an essential nutrient needed for thyroid-hormone synthesis, so it's understandable that these inferences would be drawn. There are people in the United States that suffer from iodine deficiency because of poor nutrition, and some might live in certain parts of the world (like the goiter belt in the United States) where iodine is deficient in the soil. Most people aren't aware that the majority of thyroid issues are an an autoimmune disease called Hashimotos thyroiditis.
There's one problem: when iodine is given in high amounts in the presence of inadequate amounts of selenium, inflammation can occur. Selenium is also needed to activate thyroid hormone from T4 (inactive) to T3 (active). Most patients I see, even when given Synthroid, the standard-of-care treatment, have a difficult time converting it into T3. The scientific literature also supports that the majority of thyroid conditions are autoimmune in nature, making the necessity of selenium even more important.
Too much iodine can cause a condition known as the Wolff–Chaikoff effect, which, in effect, causes short-term hypothyroidism. This is a process where too much iodine is given and the thyroid gland responds by shutting down thyroid hormone production for up to 10 days. During this time, the thyroid gland uses an escape mechanism in which more iodine accumulates in the blood by blocking its transport into the thyroid tissue via the sodium-iodide symporter (NIS). By blocking the thyroid gland's uptake of iodine, the body has time to urinate out the extra iodine.
On the other side of the fence, we see another effect known as the Jod-Basedow phenomenon in which patients with a goiter (low iodine causes an enlarged thyroid gland) who are given too much iodine will go into a hyperthyroid state.
So you can see that it gets a little confusing regarding iodine and its effects on the average person. On one side of the coin, you may get a hyperthyroid effect; on the other, you may get a hypothyroid effect.
I strongly recommend you see your functional-medicine doctor before taking large amounts of iodine. If you want to get your thyroid assessed, please click here!
When iodine is used, it should always be used in smaller amounts, tapering up to a higher dose. There are doctors who are famous for using higher amounts of iodine to treat thyroid disorders. Dr. Brownstein for instance. Even when treating Hashimoto's, he has made comments referencing that using iodine early on is akin to throwing gasoline on the fire. I am also aware that he typically uses selenium, magnesium, zinc, vitamin C, and sea salt in conjunction with iodine. As you can see, iodine is never used alone.
Using a combination of iodine and iodide is always best. There are solutions on the market, such as Lugols or Iosol, that contain the proper balance of iodine to iodide. When iodine is given in supplement form, it's primarily taken up by the breast tissues, prostate, uterus, and ovarian tissues. I always give a solution that contains both iodine and iodide.
Below is some technical scientific jargon, but as long as you understand the three key steps I share below, you will have a good grasp of what's going on in your thyroid gland.
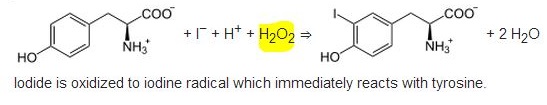
The key thing to focus on in the picture above is that when thyroid hormone is made, hydrogen peroxide (H2O2) is pumped out as a by-product of the reaction. Hydrogen peroxide can be very inflammatory and can even call some B-cell lymphocytes to the scene. The B cells are there to help clean the inflammation yet can cause more inflammation as the hydrogen peroxide accumulates.
You can think of selenium, the main ingredient to glutathione peroxidase, as the water that is needed to put out the fire in the thyroid tissue. Without selenium, thyroid will continue to burn and the immune system will continue to call more antibodies to the scene, including thyroid peroxidase antibodies (TPOAb) and TBG ab, to fight the good fight. Over time, through collateral damage, the thyroid will burn a slow death. Typically, in about 8–10 years, you will start seeing thyroid symptoms during autoimmunity.
For most patients, as they've probably already experienced, their doctor won't have too many answers outside of a Synthroid prescription. You have already read this above, but in the video as well, you will see that Synthroid does nothing to address the underlying inflammation and autoimmunity that is occurring. It also doesn't address any of the key nutrients that would be necessary to help put the fire out.
Selenomethionine (selenium) has been shown to reduce thyroid antibodies in as little as three months! Selenium is an essential nutrient that every thyroid patient needs to be supplemented with. Not all patients may need iodine initially; you may be accidentally waking a sleeping dragon if iodine is given.
If you are suffering from and autoimmune thyroid condition, click here for answers!
References:
Chapter 48, “SYNTHESIS OF THYROID HORMONES” in: Walter F., PhD. Boron (2003). Medical Physiology: A Cellular And Molecular Approach. Elsevier/Saunders. p. 1300.