
By Dr. Justin Marchegiani, DC, IFMCP
Did you know that nearly 80% of your immune system resides in your gut? That’s right—your gastrointestinal tract isn’t just responsible for digestion. It also plays a pivotal role in defending your body against infections, chronic inflammation, and autoimmune conditions.
In this article, we’ll explore how gut health directly impacts immune strength, the role of GALT and MALT, and how nutrient absorption, leaky gut, and functional medicine testing are key to building robust immune defenses.
👉 Click here to schedule a free consult with Dr. J and take control of your immune health.
Your immune system is most concentrated in your gut, specifically in areas known as GALT (Gut-Associated Lymphoid Tissue) and MALT (Mucosa-Associated Lymphoid Tissue). These immune structures monitor what enters the body through your digestive tract, ensuring pathogens are identified, tagged, and destroyed.
But when your gut is under constant stress—from processed foods, gluten, sugar, or infections—it can weaken your immune system’s efficiency. Over time, this stress can deplete nutrients, disrupt gut lining integrity, and lead to chronic inflammation or autoimmune disease.

GALT is essentially your immune surveillance system in the intestines. It comes into contact with food, bacteria, viruses, and toxins daily. If your diet is full of inflammatory triggers—like gluten, refined sugar, processed dairy, and vegetable oils—your immune system will be constantly overactive, chasing down food particles instead of fighting actual threats.
Following a whole-food, anti-inflammatory diet—like a paleo or autoimmune paleo (AIP) template—is a powerful first step in reducing gut and immune stress.
MALT is where immune cells such as T, B, and macrophages reside. When pathogens or antigens are detected in the gut, MALT activates an immune response, including releasing antibodies and natural killer cells.
If your gut is overloaded with infections (bacterial, fungal, parasitic), the immune system becomes overburdened and fatigued. It’s not that your immune system is weak—it’s that it’s distracted and overwhelmed.
This is why gut infections often correlate with frequent colds, chronic fatigue, and food sensitivities.
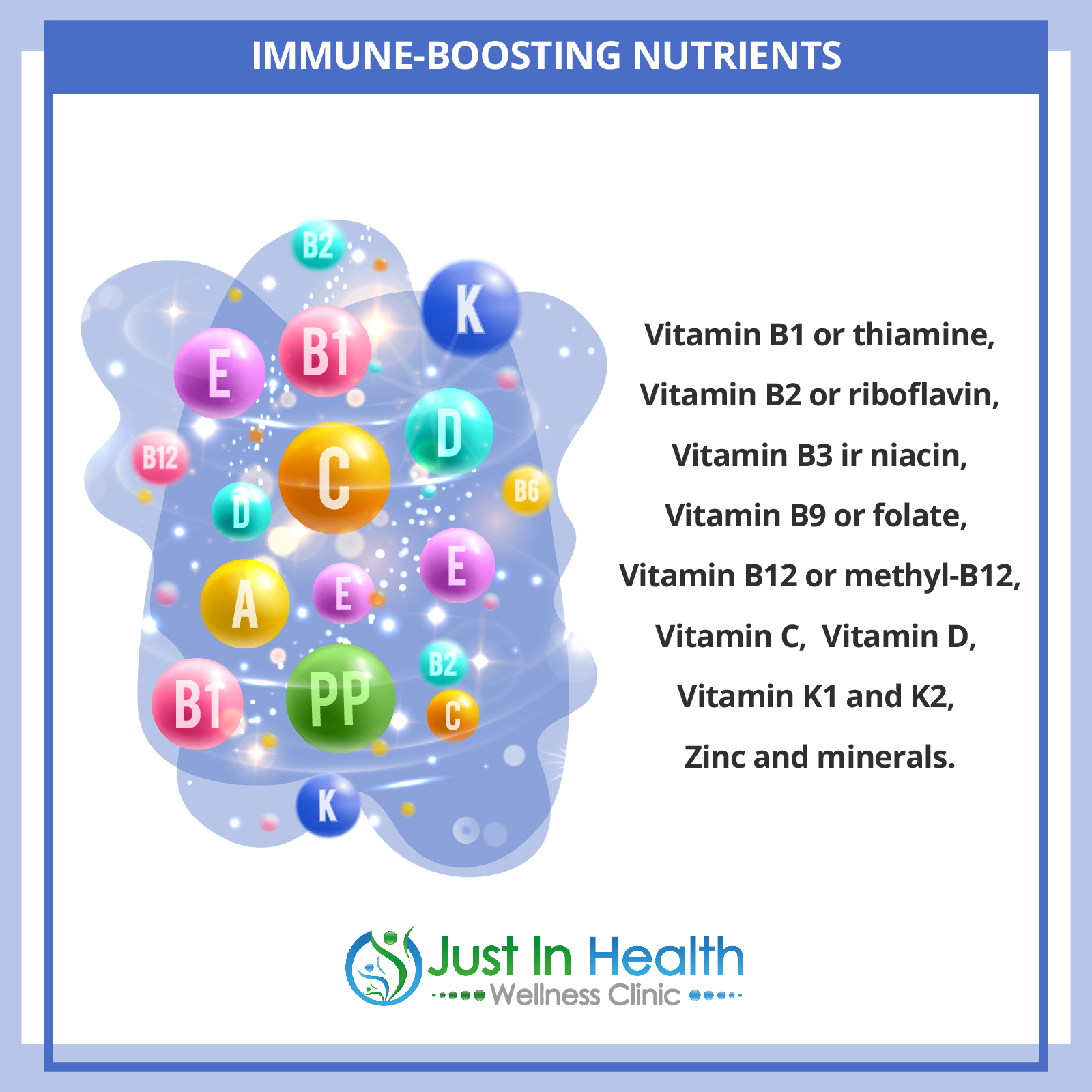
In the small intestine, finger-like structures called microvilli absorb nutrients. These structures also help maintain immune health by ensuring you absorb vital nutrients such as:
B Vitamins (B1, B2, B3, B9, B12): Support immune cell energy production and DNA repair.
Butyric Acid (Butyrate): A short-chain fatty acid that supports colon health and inhibits harmful bacteria.
Vitamin C & D: Powerful immune boosters, but only effective if absorption is optimal.
Vitamin K1 & K2: Support calcium metabolism and vascular health.
Zinc: Essential for T-cell production and antiviral defense.
Magnesium, Selenium, and other trace minerals are required for enzyme and immune function and often depend on healthy stomach acid levels.
Without proper gut function, these nutrients cannot be absorbed efficiently—even if you take supplements.
Think of your immune system like a parking attendant in a busy city. When a suspicious vehicle (virus or pathogen) arrives, it’s “tagged” with an antibody—a marker telling other immune cells, such as T cells or natural killer cells, to return and destroy it.
This tagging system relies on IgA antibodies produced in the gut-associated lymphoid tissue. If the gut is inflamed or leaky, antibody production is impaired, leading to a sluggish or overreactive immune response.

One of the most common causes of immune dysfunction is leaky gut syndrome, also known as intestinal permeability.
When the tight junctions between gut cells loosen due to inflammation, undigested food particles, bacteria, and toxins escape into the bloodstream. This activates a full-blown immune response that can lead to autoimmune diseases like Hashimoto’s, rheumatoid arthritis, psoriasis, or multiple sclerosis.
According to Dr. Alessio Fasano at Harvard, a leaky gut is a critical trigger in developing autoimmune diseases.
If you’re struggling with recurrent infections, fatigue, food sensitivities, or autoimmune conditions, it’s time to go beyond surface-level solutions.
At Just In Health, we use advanced functional medicine lab testing to uncover the root causes of immune dysregulation:
Comprehensive Stool Testing (e.g., GI-MAP): Assesses parasites, H. pylori, dysbiosis, and inflammation markers.
Organic Acids Test (OAT): Measures nutrient status, oxidative stress, and microbial imbalances.
DUTCH Hormone Test: Evaluates cortisol, sex hormones, and adrenal function—all crucial to immune resilience.
Zonulin and Intestinal Permeability Markers: Detect early-stage leaky gut and mucosal barrier breakdown.
To build a stronger immune system:
✅ Clean up your diet by removing processed and inflammatory foods
✅ Support your gut with nourishing, anti-inflammatory whole foods
✅ Address underlying infections and gut imbalances
✅ Test, don’t guess—use functional labs to uncover what’s weakening your gut
✅ Absorb key nutrients that fuel your immune system
If you're struggling with a weak immune system, frequent infections, or autoimmune symptoms, the answer could lie in your gut.
👉 Click here to schedule a free consultation with Dr. Justin Marchegiani
Let’s get to the root cause and build a personalized plan to restore your gut and immune health from the inside out.
🔬 References
Fasano A. (2012). Zonulin and its regulation of intestinal barrier function: The biological door to inflammation, autoimmunity, and cancer.
Physiological Reviews, 91(1), 151–175.
https://pubmed.ncbi.nlm.nih.gov/21248165/
Dr. Alessio Fasano discusses the link between gut permeability (leaky gut) and autoimmune disease.
Gill H. S., & Prasad J. (2008). Probiotics, immunomodulation, and health benefits.
Advances in Experimental Medicine and Biology, 606, 423–454.
https://pubmed.ncbi.nlm.nih.gov/18183936/
Explains how the gut microbiota influences immune response and supports immune homeostasis.
Belkaid Y., & Hand T. W. (2014). Role of the microbiota in immunity and inflammation.
Cell, 157(1), 121–141.
https://pubmed.ncbi.nlm.nih.gov/24679531/
Covers the impact of gut bacteria on the immune system and inflammatory conditions.
Macpherson A. J., & Harris N. L. (2004). Interactions between commensal intestinal bacteria and the immune system.
Nature Reviews Immunology, 4(6), 478–485.
https://pubmed.ncbi.nlm.nih.gov/15173836/
Describes how gut-associated lymphoid tissue (GALT) interacts with microbiota and shapes immune function.
Rooks M. G., & Garrett W. S. (2016). Gut microbiota, metabolites and host immunity.
Nature Reviews Immunology, 16(6), 341–352.
https://pubmed.ncbi.nlm.nih.gov/27231050/
Highlights the role of short-chain fatty acids like butyrate in immune regulation.
Valdes A. M., et al. (2018). Role of the gut microbiota in nutrition and health.
BMJ, 361, k2179.
https://www.bmj.com/content/361/bmj.k2179
Discusses nutrient synthesis (e.g., B vitamins, vitamin K) by gut bacteria and their impact on immunity.
Kau A. L., et al. (2011). Human nutrition, the gut microbiome and the immune system.
Nature, 474(7351), 327–336.
https://pubmed.ncbi.nlm.nih.gov/21677749/
Explores the dynamic interactions between dietary intake, gut flora, and immune function.
====================
Recommended Products
====================
Recommended Lab Tests