
Parasitic infections are a big problem in tropical and subtropical regions of the world. In this video, Dr. J and Evan will share how to handle these cases. One of these is giardiasis that may cause diarrhea, gas, upset stomach, greasy stools, and dehydration; cryptosporidiosis, which may cause stomach cramps, stomach pain, nausea, vomiting, dehydration, weight loss, and fever; toxoplasmosis may cause flu-like symptoms, including swollen lymph nodes and muscle aches or pains that can last for over a month.

Dr. Justin Marchegiani
In this episode, we cover:
0:05 Parasites and Thyroid Issues
8:05 Conventional Medicines on Parasites
12:50 Thyroid Symptoms
16:54 Adrenals as Natural Inflammatory
19:55 Gut Healing Protocols
Dr. Justin Marchegiani: Hey there, it's Dr. Justin Marchegiani. I'm with Evan Brand, Evan, how are we doing today? My friend?
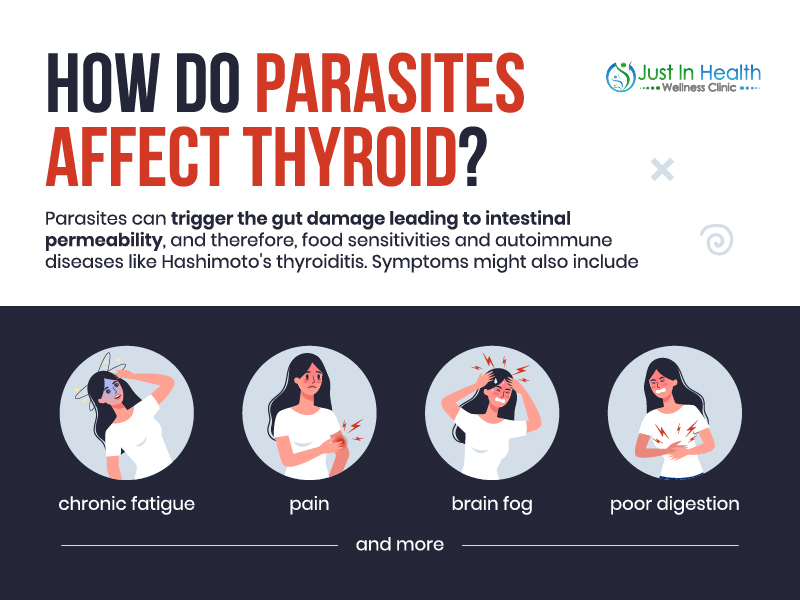
Evan Brand: I'm doing well. I'm excited to dive into this, you thought of the idea of parasites and thyroid issues? And I said, Well, that's easy, because we've seen hundreds and hundreds of cases at this point where thyroid issues magically get better or even resolve themselves just by fixing infections. Now, I will I will say that, you know, even though the title of this is parasites and thyroid, I would argue other infections are probably going to be happening at the same time. It's rare that you and I, when we're doing functional stool testing, it's rare that you and I find just a parasite, right? Like, we're probably going to find some Candida, we're probably going to find some cebo type stuff, maybe some CFO issues, maybe some worms, maybe some gut inflammation, but parasites can be a really big catalyst for thyroid issues.
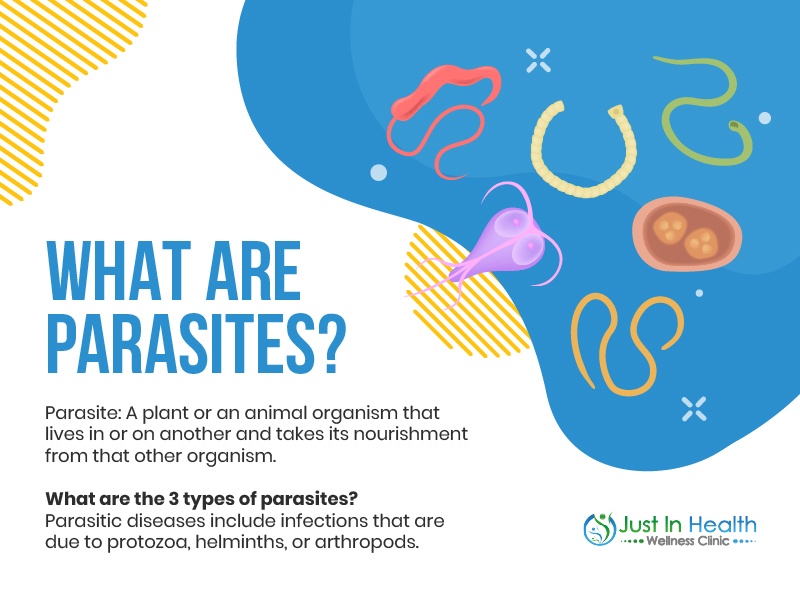
Dr. Justin Marchegiani: 100%. So we talk about these topics, you know, in a lot of different ways, so we try to nuance it a little bit. So if you've heard topics on parasite infections before from our podcast, we'll try to make it a little bit different for you. So you get a little bit of a different perspective on this. So parasites are really a big deal. Gut infections is general and you can kind of lump in SIBO and Candida with this as well. Parasites can be a little bit more severe. Right, we have blasto, e, histo, Giardia, Cryptosporidium, any of the immediate miba infections, d fragilis. penta trichomonas, hominess. Trying to think of some other ones here, we have different worm infections, right. And these can all create inflammation in the body. But more importantly, besides inflammation, they can create gut permeability. And when the guts more permeable, we can have more immune stress, right, the more the immune system is stressed, because 80% of the immune systems in the malt, and the golf, right malt is the mucosal associated lymphoid tissue that's in the stomach. I'm sorry, that that's in the small intestine and the golf, that's the gastric associated lymphoid tissue that's in the stomach. And we have immune cells in these tissues. And the more stressed they are, the more gut permeability we have due to infections, that can really exacerbate the immune system. And they can wind it up so to speak. And the more wound up the immune system is that can facilitate an autoimmune attack. And that means your immune system starts making B cell or antibodies to the thyroid, and you may make things like TPO antibodies, which may affect the enzyme that helps bind that thyroid together, thyroid peroxidase. And that can affect the thyroid. And you may make thyroid globulin antibodies, which work on the extra cellular protein on the thyroid, and that can attack that. And so when you start damaging and beating up the thyroid due to autoimmune attacks, that can impair thyroid function and thyroid hormone binding. And a lot of that can start with the immune system. And the biggest trigger for that can be a gut infection.
Evan Brand: So let's roleplay a little bit if you don't mind. So, you know, I'm Joey, and I go down to the the local gastroenterology clinic and I tell him that I saw this guy named Dr. Justin on the internet and he told me that, you know, blast over crypto or God may be causing my thyroid issues and the gastro doctor says no, you live in America, you know, not gonna happen. What do you say to that guy?
Dr. Justin Marchegiani: Well, that's kind of the the big thinking with a lot of conventional doctors is, hey, these parasite infections only happen in third world countries. And so it's a big deal in third world countries. It's like one of the number of top five causes of death in third world countries partly because you get amoebic dysentery, massive diarrhea, electrolyte depletion, cardiac arrest, or some kind of hyponatremia symptom, because you have massive diarrhea. Now here, you go to an ER, they put you on an IV, they flooded with antibiotics, and more than likely, you're gonna be fine, right? You may have side effects later, that's a whole different podcast, but you'll be fine. The problem is, we kind of look at parasite infections having this acute symptomology that results from the infection. And a lot of times, that may not be the case, you may be in this kind of functional asymptomatic place where you don't have over diarrhea, you don't have over constipation. You know, you may have some but not a ton. And then a lot of times it's just enough where they kind of throw the IBS diagnosis at you, they may run a scope they may not see anything, they may run a stool test not using the best technology so they may miss whatever's there. Now, if you have a serious infection, there technology, you know, basic stool antigen looking under a microscope, they'll probably catch it. But if it's there's not a lot of bolus of that parasitic material, they may miss it and that's where some of the DNA technology maybe a little bit better for picking up parasites. So this is why they may miss it, number one, number two, you may have kind of these subclinical symptoms that may get lumped into the category of IBS, which is a diagnosis of exclusion, meaning they ruled out krones all sort of colitis, right? They ruled out bowel impaction acid reflux, all these other inflammatory issues, ulcers, right? And now, okay, all the serious stuff is ruled out. So they just say, okay, we're going to just call it IBS. And then they're going to just give you some medications to control whatever symptoms you have going on, whether it's antispasmodics acid blockers, whether it's um, constipation, medic medicate medication like laxatives, or bloating, medication, etc, gas x, that's all they're gonna do after that. And we know with functional medicine world, a lot of parasite infections can actually cause energy and mood issues. And so this is totally over their heads in conventional medicine world, because now they're used to connecting gut infection to gut symptoms. It's like an A, it's like a one to one relationship. Right? Now you start going three dimensional here, when you start talking about gut infections, exacerbating your thyroid, causing an autoimmune attack, and now you have anxiety and heart palpitations in in fatigue and depression all throughout the day. Now what? And then now if those symptoms happen, you're more than likely going to be prescribed a anti depressant or medication to treat those symptoms. So you're kind of getting this really big cascade of symptoms that don't quite match up with the conventional mindset.
Evan Brand: Yeah, and it blows their mind and then they get overwhelmed, and then they'll dismiss you and then they may send you off to the psychiatrist. And they say, Well, you know, I don't really help with anxiety. I'm focused on the gut portion of this. Luckily, you know, what we do as practitioners we come in and we're not neurologists and gastroenterologist and endocrinologist and, you know, kidney experts, but we've had enough experience to where we can actually address each piece of this spiderweb. I mean, you you eloquently described it here, you've got the GI complaint that most people think about, they think, okay, if I have parasites, I've got to have diarrhea, I've got to have stomach pain, not necessarily. We've seen hundreds of people where they're just a little bit tired. And maybe once every few weeks, they have kind of a cyclical gut issue. Right? So for me, it was definitely, it was definitely like a cyclical pattern. And I was trying to track it down to the diet. I thought, okay, you know, is it dairy? So then we got off dairy and then we like, reintroduce grass fed dairy without Okay, is it that Okay, what about the grains is the grains? No, it was the infections, but they had a cyclical pattern. So when you start bringing stuff up like that, you'll literally you just lose the ear of the the conventional practitioner. So back to the thyroid piece, or you mentioned like the immune cells, you mentioned the immune stress. Now, we're also going to be looking at blood for this right? So you would suggest if we are seeing a lot of these hyper hypo symptoms, yes, we're going to run some DNA stool testing. But we're also going to want to look at blood too, because we may find some other answers there. Now, I would argue, and I'm guessing you may agree with me that the blood is going to be more of looking at the effect, not necessarily the cause. Meaning if you look at the gut infections, that's more of a cause. But we may see the TPO antibodies, you may see the tg antibodies, you may sit, we may see like a high reverse t three. But but that doesn't necessarily change the game plan, right? Because you still have to go to the gut to fix the parasites that caused the high reverse t three in the first place.
Dr. Justin Marchegiani: Correct. So how conventional medicine looks at things right may not pick some of these things up. So let's say they're even looking in the thyroid, let's say they're kind of let's say they're entertaining. And let's say you listen to this podcast, you go in, and they're testing your gut, and you're like, Hey, can you also look at my thyroid, too, they may not even run these markers, as they typically run just TSH, and maybe if you're lucky, you can get a T for free your total. That's it. Now, if your TSH is overly high, then it'll get picked up. But what is overly high, you know, maybe greater than four and a half to five. But it can take a long time for the TSH to go that high. Like TSH doesn't just go high like that, in the snap of your fingers, it takes a lot of years, maybe even decade to get to that level. So if you have high TSH, you can just guarantee that that issues been going on for a long time. So that's pretty much how you know if it's a if it's been going on for a while. And then now you have the downstream t four and T three that need to be looked at and T three is very important because T three gets converted from t four. So t four is your inactive thyroid hormone. T three is your active thyroid hormone. We almost never test this T three number. And a lot of times we can have a conversion issue. So your T four may be adequate. And then we have a drop in T three. So t three is not at an equal par In regards to the percentile of the reference range. And then we definitely know antibodies aren't tested. That's really tough. And partly because they don't do anything because of it because treating a thyroid autoimmune condition with conventional medicine standards. They use high dose prednisone and immunosuppressive medications, those medications for a thyroid issue that would actually cause more side effects than the thyroid issue itself. So they tend to stay away from treating a thyroid issue. So they don't really do any tests to reveal that it's there. If it's autoimmune, so you kind of get stuck in no man's land.
Evan Brand: Oh god, that's a great point. That's what I was gonna say. I mean, it just frustrates me where you and I will have you know, new patients come and they'll send us bloodwork and we'll look at these, you know endocrinologist that may have even extra credentials, but yet their their thyroid panel is still more generic than what you and I are running. And it just infuriates me, because these people, they're spending so much money, they're traveling to Mayo Clinic and whatever else, and they're still not even getting what you and I would consider basic or foundational screening, it's really frustrating.
Dr. Justin Marchegiani: Yeah, it's a combination of two things. It's a combination of one they're not aware, because they've kind of been like handcuffed, like, Oh, we can't do anything about it anyway. So they kind of feel a little bit handcuffed and defeated. And then number two, they don't want to piss off the insurance company. Because if they're ordering via the insurance company, they don't want the insurance company kicking them out of network for doing unnecessary testing, right? So you get in this position where you're like, crap, well, how do I how do I handle this? How do I navigate as a doctor? And so we exist in the world of cash medicine, so we can do what we want and do what we recommend and need, what the patient needs. And we don't have to worry about some insurance company dictating what we can do for the patient. The problem with insurance is they can't they get in the middle. And they're basically imagine someone getting in between you and your doctor and questioning everything you're doing and saying, well, you probably don't need that. So well. Let me talk to the patient about that. And see if the patient thinks we need it or not. I'm going to make a recommendation most of the time the patient's like, yeah, that totally makes sense. Let's do it. But imagine that insurance company stepping in between you and saying, Well, I don't know about that. So we have that advantage in on the functional medicine side not going through insurance, because we can give the patient exactly what they need.
Evan Brand: Yeah, great point. Yeah, I mean, the question my grandfather, for years, I would push him, Hey, I really want you to get full thyroid panel, I really want you to get vitamin D, and then the doctor would immediately push back, well, vitamin D is not going to be covered. Are you okay with that? You know, and then of course, it always ended up being covered. So it was this weird, like in between land where you feel like you're not getting the proper care that you need, because they're fearful, you know, the doctors are fearing that they're going to go, like you said out of the network, or kind of out of their normal bounds of training. And then also, like you mentioned, that would illuminate any deficiencies they have in their treatment model, because if all of a sudden, they run TPO antibodies, and you do the follow up, and they've never looked at TPO antibodies, they don't have a clue to say, Hey, why don't we do a DNA stool test? Let's go look at these infections in your gut. Now I'm connecting the dots here, you're having anxiety, heart palpitations, you've got elevated TPO antibodies, and you're having cyclical diarrhea, Hmm, I don't know what the heck to do. Here is your thyroid medication. Here's your Synthroid, or whatever. And then here is maybe, like you said, an IBS type drug. And that's it. So let's get back more to the action steps. I think we've done a great job of kind of illuminating, how does this happen? But first step, when somebody comes in and you see thyroid, you see gut issues. You mentioned DNA stool test, are you going to run blood immediately? Or is that more of like a downstream effect? So you don't worry about it up front?
Dr. Justin Marchegiani: You mean blood for the thyroid?
Evan Brand: Yes. Like, are you going to do thyroid panel at the same time as a stool? Or are you going to just focus on the gut?
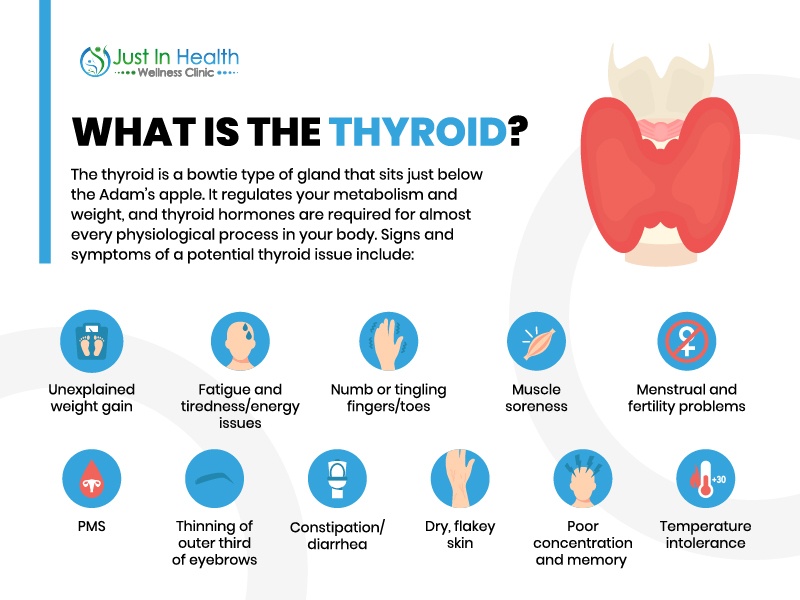
Dr. Justin Marchegiani: Only if I see over thyroid symptoms, if there's any family history, because a lot of times thyroid can overlap with adrenals. So I always look at the adrenals. First before thyroid unless we see a lot of hair loss, a lot of cool hands, a lot of cool feed stuff, a lot of weak fingernails, if we see a lot of low thyroid symptoms, that I'm going to take a look at it. Now most people they've already done some digging around their thyroid before they come see me. So usually, there's some labs that have already been run that I can look at. And if not, then if we have those issues, then we're either going to one, just go after the adrenals month one if we don't have any overt symptoms, and see how we do. And then if we're not having improvements out of the gates in regards to temperature, energy, those kind of things, then we do it. If we see that temperature and energy is a big deal out of the gates and we know cold hands cold feet hair loss, we can quantify that maybe with some basil, temperature testing, and we know it, then we'll probably just rule out that low thyroid out of the gates just to make sure so it just kind of depends where patients are coming in from. And of course, if it's family history that that's we're going to really dive into that. And because autoimmunity affects women five times more than men, if it's a female patient, I'm a lot more on point with it. And if we have history of it, sister, aunt, uncle, mom, dad, whatever, then we're going to be looking even more closely. But if I'm on the fence, usually I'll just have patients do some basil, temperature testing with a really good digital thermometer. And we use the protocol in the members area, which is, you know, testing armpit axillary area and 97.8 to 98, two in the morning, or 98 to 98 six for the mouth. And we'll just kind of test that we'll do three, three temperatures test in the morning before you get up and move around. And we'll just kind of get a window of how good that temperature is or not.
Evan Brand: So if you're on that low end, did you say 97.8 was at your low end?
Dr. Justin Marchegiani: That's armpit axillary, same thing. So when you're nine to 98, six for the mouth oral.
Evan Brand: Okay. So if you're at that very low end, is that still okay? Or you start to get concerned in that 97.8 level.
Dr. Justin Marchegiani: It would depend it would depend where the patient is if they have thyroid symptoms, I'd be more I start to get more concerned when they're going below 97. Mm hmm. You know, also, I'm always I'm always in 97, like, I'm 97.8 all the time, and I'm thinking, well, crap, you know what, why am I not 98. But that isn't that big of a deal. Like I'm getting a little more concerned, I'm below 97. But with women, you got to be careful because women's temperature can dip right before oscillation and then peak as going through regulation. So if you grab that temperature, right before isolation, it could look a little bit artificially low. But also, if you grab it right in and after ovulation, it could be artificially high. So as a female, you know, the best time of the cycle to test is part of that first five or six days?
Yeah, okay, that's good information, you know, what's it want to first aid, you bleed so that first five or six days, from bleeding onward.
Evan Brand: It's a little bit of a tangent, but I'll just mention it because you're on temperature. So apparently, Lyme spy repeats affect the hypothalamus, which affects body temperature. So I've used temperature as well as kind of an investigation tool. And as we've treated people with Lyme issues, sounds like maybe the hypothalamus starts working more efficiently. And then boom, temperature regulation gets better, because that was a big issue for me, where, you know, I had major issue with the cold. And we'd always look at thyroid, we knew, you know, you know, my my gut story with parasite infection. So I would look at thyroid, and I would never see any issues, I was always perfectly in the functional ranges. So there are some other pieces to this puzzle. But I want to hit on the adrenal piece, too. That was interesting. So you had brought up like this adrenal thyroid connection to and that's going to be tied into the gut, right, you're going to see potential adrenal issues because of the immune stress based on the gut stress. So it could go gut affecting adrenals. And then adrenal is affecting thyroid, right? It might not just be gut thyroid, you're saying the missing link in between those two is adrenals.
Dr. Justin Marchegiani: It can be because the adrenals are your natural anti inflammatory. So if you have a lot of inflammation in the body, from a infection, your adrenals are going to be spitting out cortisol, natural corticosteroids to help with that inflammation and stress. So like conventional medicine, a lot of times we'll do prednisone, right? That's like a really strong steroid. Well, your body has its own natural steroids it would use so of course, if you're whipping that tired horse, that can be something that gets affected. And then of course, when your immune system starts getting overly stimulated from infections from now, maybe an increased chance of food allergens, because now your guts more permeable, undigested food particles can kind of make their way into the bloodstream and create more immune stress because now your immune system sees foods floating around the bloodstream and digested that shouldn't be there. And so then now, you know, your, your immune is maybe tagging those proteins. And we know the surface proteins on gluten, for instance, maybe dairy, those the surface proteins look very similar to the thyroid, so your body can actually start mistakenly attacking thyroid tissue because those proteins look kind of similar.
Evan Brand: And yeah, and I just want to clarify this issue is going to be more common. It's going to happen more frequently, when there are gut issues disrupting the immune regulation, correct. It's not like in every person, dairies magically going to trigger thyroid antibodies, you're saying in these gut compromised people that may have infections because of the intestinal permeability being increased? Now there's more antigen getting in to the bloodstream and then boom.
Dr. Justin Marchegiani: Yeah, I mean, it's gonna be heightened more with an infection, because like, imagine the infection is like already kind of cracking the door open and your gut lining a little bit more. But let's say you didn't have an infection. It's possible certain food allergies could be enough to crack that door as well. Right. Okay. But either way, let's say you are sensitive and you have food allergy issues, and you have an infection now, it's a double whammy, instead of that door being cracked open. Now it's wide open, right? Yes, that makes makes that makes perfect sense. Yeah, for me, I mean, I used to do really, really poorly with dairy now really high quality dairy, I can get away with a little bit because I've healed my gut so much. So for me, I saw it. And it depends, right? Because not all dairy is created equal. So butter, fats and high fat dairy is usually different than dairy that has more casein, right? casein based areas tend to be like, more cheese or milks, right fat based areas and they'll be like ghee, butter, maybe heavy cream. So casein tends to be the more allergenic portion of the dairy. And then, of course, we have lactose and lactose is the sugar portion of the dairy. So lactose, it's more of an intolerance. And you just get more digestive disruptions where casein could be more of that immune stimulant. So things like people that have dairy intolerances, still may be able to tolerate ghee or butter. Because Because it's not, it's pretty low in casein much higher in the fat. Fats tend to be more neutral for people tend to be able to tolerate good fats, especially saturated fats because they're, they're not easily oxidized.
Evan Brand: Yes, yes. Well said that's a great point. So what about the influence of the gut healing protocols that we implement, and thyroid because people are hearing parasites, so they're thinking, kill, kill, kill. And that definitely is part of it. And you and I've seen where just by eradicating infections, we've seen multiple things happen, which is pretty cool. So number one will see that the Secretory IgA, which is a marker, we look at on stool testing secretory, IGA will come up just as a side effect of clearing out infections. And that already indicates, hey, look, we're starting to get on the healing path before we even did a quote healing protocol. And then we'll see thyroid antibodies come down sometimes hundreds, sometimes 1000s of points, just by clearing the infections out. Okay, so that's really like boom, clear infections out. But what about the gut healing phase? What are you seeing there? Are you seeing that that's the, you know, the secret sauce, where thyroid really comes down in the gut healing phase? Are you finding, you know, if you had a pie chart, are you saying killing is doing most of the work for leaving the stress on the thyroid? Is it the gut healing phase? is there is there one that's a bigger importance than the other?
Dr. Justin Marchegiani: Depends on how acute the infection is, but we're doing so many things at once. Like, this is the question I get, like, what's causing What? And it's like, it's very difficult to know that because what's the most important number in a combination to your safe log? what's the what's the most important ingredient in the recipe your mom makes, right? Well, it's a combination, everything, right. And so when you're dealing with an infection, I'm very rarely coming in there and practicing Acute Care Medicine where we're just going after an infection where we're changing the diet, we're decreasing inflammation by having a healthy anti inflammatory kind of paleo template, we're improving digestion, that in its own right starts to improve nutrient absorption, we may add in some extra nutrients as well, that are easily bioavailable. So then we can get those in our bloodstream and start utilizing the metabolically. Obviously, the thyroid needs some zinc, it needs some selenium, it needs some iodine. Of course, we don't want to ever go overly high with iodine because that can actually increase autoimmune attack, but a couple 100 micrograms, as long as there's not an acute attack may be fine. And then of course, we're working on supporting hormones, right, we working on maybe supporting thyroid, if the thyroid is depleted, meaning you've had a decade or so autoimmune attacks, you may need some thyroid hormone, depending on how much that that thyroid been beaten down. If the thyroid still functioning, well, then just doing a lot of the good nutritional strategies may be enough to help it do what it's what it needs to do. And then we're coming in down the road going after the infections a little bit later. Now we're an antibiotic kind of focus generation, right? It's like, Oh, I have an infection, you have this antibiotic, antibiotic antibiotic. So that's kind of translated to people wanting to kill whatever they have right away. Now, if it's an acute infection, you went to Mexico, you ate something like you just got diarrhea, and you're having like a dozen VMs a day, right. And it just diarrhea, that we may have to handle that differently than like a chronic infection that's been happening over the long run. So I always put infections in two different groups, acute or chronic. And then we always still have to work on doing all the foundational things. If it's acute, it may be a lot more compressed over a couple of days versus a month or two, if it's a more chronic issue, and regarding how we start going after the gut.
Evan Brand: Yeah, and the adrenal is maybe less important to deal with right away, if it's a really bad, acute thing. It just depends upon like, Hey, I'm great, I'm great, I'm great, boom, I'm going to the bathroom a dozen times a day, it's not good. My tummy feels like crap. If it's that kind of an acute thing, and you were relatively okay ahead of time, then we're going to look at that differently than a chronic infection. I love the analogy, what is the what's the most important, you know, numeral to your to your safe code? Because I know the answer to the question I asked you, which was like, what's a bigger deal here? Is it clear in the infections? Is it you know, healing the gut? Is it reducing food allergens? And I asked that just because I'm just playing devil's advocate, because that's what clients and patients always ask, you know, when we're working with them, they're like, Okay, well, you know, what's my biggest priority right now? It's like, I'm all of it. So it may sound a little overwhelming. But as we're taking small steps with the diet, the lifestyle, we're getting you to bed sooner, we're helping with adaptogenic herbs to support the adrenals where, you know, let's say you're in between jobs, you're moving house, I mean, there's lifestyle stuff that's important. You know, that's, that's affecting your hormones, which is affecting your sleep, which is affecting your gut and your recovery. And so we're factoring in all of this at the same time, so rarely in a vacuum. Are we just coming in, like you said, and just boom, here's your random microbials. Have a nice day. That's very rare situation, right?
Dr. Justin Marchegiani: I mean, like, let's say, you're healthy, right? You go down to Mexico, you pick up crypto, and then you just start having really a lot of diarrhea, we may handle you a lot differently. But like a lot of people that come in and I see usually there's a combination of maybe some kind of a food allergy issue happening in the background. So then we clean that out, that maybe helps a third and then maybe they've really had poor digestion for a while like you know inadequate HDL or enzyme levels, that starts to help maybe a third or a quarter. And then that starts to modulate and calm down the immune system. So now the immune system kind of can relax a little bit, maybe that's 10% 20%. And that we have, we're getting access to maybe more Selenium or more zinc in our diet now. And that starts to help modulate the immune response, maybe that nourishes thyroid conversion, and then let's say the infection, right, let's say that's the last 20%. So it could be a combination of certain things, you know, 10%, here, 20% there, 30%. There, and it just adds up. And so in the end, it's hard to know exactly which one's going to be the winner, right? And sometimes it's equally spread out. That's why if we just do the things that we know, we need to do on our checklist, our chance of results, good results is going to be much higher.
Evan Brand: Absolutely. Well, I'm out of time. So I don't know if you have a lot more to say if so I'll just leave but if you don't, then let's wrap it up together.
Dr. Justin Marchegiani: That sounds great. I think let's wrap it up here to reach out to Evan head over to EvanBrand.com again, Evan and I are available for consultation worldwide, which is excellent in today's day and age. And then myself, Dr. J over at JustinHealth.com. We're happy to help you out and work deeper on any thyroid issue. Gut issue infection issue where we can kind of dive in deeper and get to the root cause make sure you put your comments below and subscribe and share the episode with friends and family. We really appreciate it.
Evan Brand: Absolutely. Yes, sharing is caring and there's probably someone in your family or your life that has a thyroid issue. So please give this to them. Hopefully, even if they have to listen to it two, three times. Hopefully it helps guide them in the right direction to heal to recover to live life fully. So take care.
Dr. Justin Marchegiani: Awesome and have a good one man. Bye
https://justinhealth.libsyn.com/can-parasites-cause-thyroid-problems-podcast-316