
The AIP diet is an elimination and reintroduction protocol which aims to reduce inflammation in the gut, heal the gastrointestinal tract and in turn, reduce overall systemic inflammation. It is a diet targeted specifically at autoimmune diseases. We have Dr. J and Evan chatting about the benefits of this diet and how it can bring our body to a healthier state.
One of the biggest benefits of the AIP diet is its ability to alleviate inflammation, which is key to reducing symptoms of autoimmune conditions and promoting better health. Eliminating a few specific foods from the diet and filling up on nutrient-dense whole foods instead can have a powerful effect when it comes to inflammation.
Check out the podcast below for more info!

Dr. Justin Marchegiani
In this episode, we cover:
0:42 What is Autoimmune Paleo
8:14 How is it Beneficial
21:18 How to’s in Food Sensitivity Issues
26:22 How Paleo Helps in AIP
31:03 Goal of Decreasing Immune Stress
Dr. Justin Marchegiani: We are live. It's Dr. J in the house. Evan, how you doing today man?
Evan Brand: Doing well, let's dive in. Let's have some fun. We're going to talk all about autoimmune paleo, which is the template that we push a lot of people towards, not because we're some dogmatic attached to our cards kind of people, but because we like results. We like clinical success. We like people to get better. We like people to reverse their health issues. We like people to take back their health, we like people to get off their medications when their doctor allows them to. And autoimmune paleo is by far the best template you and I've ever implemented clinically, which has given us those various types of success. So where should we start?
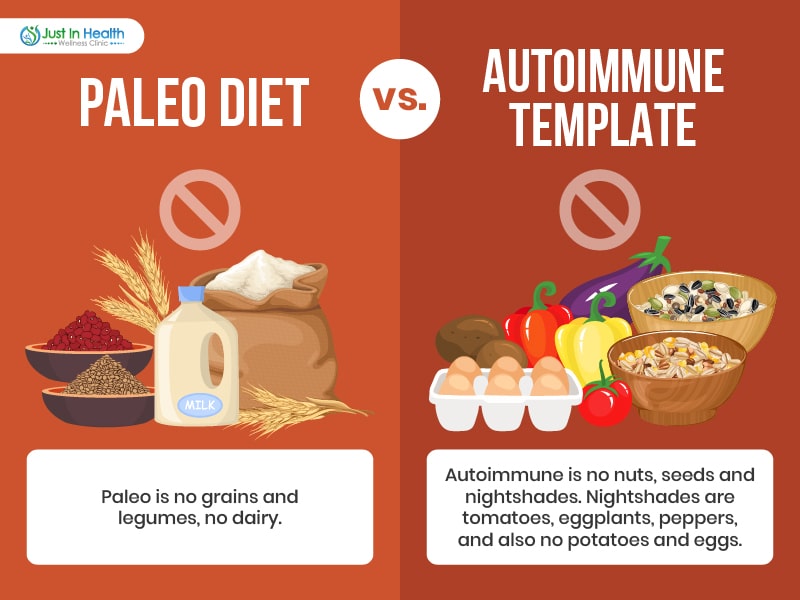
Dr. Justin Marchegiani: Yeah, so off the bat, what is autoimmune paleo, so it's a good starting point. It may not be good for everyone out of the gates, it just for me, it depends, right? I see a lot of patients that are sick and then have done a lot of things. And this is like the next logical step. If people were coming in to see me and they already have, let's just say have a really kind of crappy kind of standard American diet. I may just start out with a Paleo Diet out of the gate. So we have paleo right that's like no grains, legumes, dairy and then like kind of butter maybe like acceptable within that range that and then obviously no legumes, grains, so no grains, legumes or dairy, butter, acceptable meat, acceptable vegetables, non starchy veggies, and then of course, good healthy fats, right, not seeds, dairy based fats, animal fats are all acceptable. Okay, and then we have paleo I call it paleo 2.0, which is the equivalent to an autoimmune paleo template. And you notice how we use the word diets not. We use the word template, not diet. I don't like the word diet, because diet is it's very inflexible. This is what you eat, where a template gives you the ability to adjust things. So I like the flexibility within the description template. So an autoimmune template versus the Paleo template. paleo is no grains and legumes, no dairy. autoimmune is no nuts, seeds, nightshades nightshades, being tomatoes, potatoes, eggplants, peppers, and eggs. And so within that, that template, we're still going to be having healthy proteins, healthy fats from animal products, fats that are not seated dairy free, but healthy animal products, other fats like olive avocado, and palm and coconut are all great. And then carbohydrates, from fruits from vegetables, minus the tomatoes, potatoes, eggplants, peppers, and we can adjust the macros accordingly, proteins, fats, and carbs. So that's kind of a good first step out of the gate. So paleo, and then paleo 2.0, which is going to be on one and paleo and these are all paleo template, autoimmune template out of the gates.
Evan Brand: Yeah. And people don't necessarily need to get stuck on the 2.0 the AIP forever. Okay, so this is not a podcast to say, look, everybody needs to do this. As Justin mentioned earlier, you know, we're working with a lot of people clinically who've been to 510 20 practitioners before us, they've been on every diet under the sun, they've done every treatment under the sun, whether it's natural pathi, homeopathy, functional medicine, doctors, conventional doctors, they've already been through the wringer. So in our patient population, it's a bit more skewed towards the autoimmune because of the type of people we're seeing. Now occasionally, we'll get people in that are just Healthy People that want to feel better, or athletes and those people are not as compromised. And so for those, maybe we're just standard paleo, and there's a lot more flexibility. So just want to make that distinction because I don't want your average person who doesn't really have any major concerns thinking they need to go, you know, stick with AIP for life.
Dr. Justin Marchegiani: 100%. Now, what if you don't have an autoimmune diet? What if you don't have an autoimmune disease? Should you do an autoimmune template? Well, here's the deal, autoimmune template, really, the goal is you're cutting out any food that has a higher chance of being hyper allergenic, right, there's a lot of data on these different studies with nuts or seeds, that they can they have one anti nutrients in them, right oxalates phytase, either they affect protein digestion, mineral absorption, and they can be irritating on the gut lining. So there's a lot of hyper allergenicity increased immune activity. So the and then they also have maybe potentially more omega six fatty acids that can drive down more of the pro inflammatory pathway. So the goal is that we're trying to reduce some of these anti nutrients that have a negative impact on the gut lining. And the number two, we're trying to increase nutrient density. Alright, so we're choosing foods that are higher and better fats, right? fats that are polyunsaturated fats that are more polyunsaturated, they can be damaged and they can be oxidized, right so animal fats, coconut oil, saturated fats, not so much. And and then just the just the gut permeability aspect. So we see nuts and seeds fit that criteria. Eggs potentially even though eggs are awesome and so nutrient dense with a good vitamin A and fat soluble vitamins and cholesterol in the yolk, especially, they're amazing. So sometimes those compounds can be a little bit more allergenic. So can the nightshades with the alpha solonian compound and they're in the saponins. They can be a little bit More irritating on the guts get into the joints create inflammation. So it depends. The goal is really that it's just a nutrient dense, anti inflammatory and then low in toxins, but more importantly, plant toxins, anti nutrients.
Evan Brand: Yeah, well said and the reason you're bringing up the lectins. And some of these other compounds of these foods are because they're going to contribute to increased intestinal permeability. So when you're talking with anyone, whether it's rheumatoid arthritis or some other autoimmune disease, there's always a domino that has to fall which is that the gut is leaky, this increased intestinal permeability has to take place. Now we've gone into the details of why that can happen from the infection perspective, low stomach acid, food fermenting in the gut, bacterial overgrowth, parasites, emotional stress, overtraining, we've tried to hit a lot of these different variables that can go into the leaky gut. But you can also have all the lifestyle infection piece dialed in, but if you're eating, let's just say, you're doing salsa on your, you know, cassava flour, tortillas and your grass fed ground beef, but you're just doing, I don't know corn chips and salsa all the time with it, it's possible that a lot of those lectins like you may get from your nightshades like your tomatoes and peppers. Those can irritate the gut lining contribute to that leaky gut and then that's going to increase your autoimmune risk. Or if you're already autoimmune, it may potentially flare you up depending on what's going on.
Dr. Justin Marchegiani: Absolutely, there's one study that came out looking at people that have potential autoimmune genetics, they have the likelihood to make 10 times more IGA antibodies against certain foods than healthier foods. And in this one study, it's called food intolerance and patients with a manifest autoimmunity with manifest autoimmunity observational study, in the Journal of autoimmune review, they talk about that the IGG level for specific foods were higher in the patient control group and the control group. So if these people that had autoimmunity they had more antibodies, and what they found was they saw a significant increase level and IGG. That's a type of antibody that's produced. And most doctors only look at IGE, which is anaphylaxis type of allergy response, immune response. And that's like you need the epi pen for that right and so this is kind of IGG there are other types of responses that aren't even in that IGG IGA, IGM IGE category, and so IGG isn't the be all end all by the way. But they found that casein cow's milk weekly and wider the eggs, rice, even some nuts and what and walnuts and almonds tend to have more of a allergenic idg response. They found no antibody reaction with vegetables and fish and meat products. They seem to be very immunoglobulin neutral. Guess what we do with an autoimmune template or a paleo template, we're cutting most of those foods out. Obviously, with autoimmune, we're focusing cutting the eggs out and the nuts and the seeds out to that's it's about decreasing the immune response. People that have a lot of autoimmunity, their immune system is sucking up lots of energy and lots of resources, because it's responding to all this food in a negative way. And so the goal is we're just trying to calm down the immune system. And then those foods aren't there. We don't have the gut permeability. Therefore the the body can use those resources better versus having the immune system hyper responding.
Evan Brand: Yeah, well said. Now, one other point to why would this be beneficial to do or to go down this rabbit hole and as I mentioned, maybe not forever, right? Maybe temporarily, we pull out eggs for me, I pulled out eggs for a long time when I had gut bugs. I had an Louise on the podcast and we talked all about gallbladder and eggs and how there's a big factor there where eggs can irritate the gut, you know, just based on the gallbladder issues. And so I pulled them out and now I can tolerate eggs, no problem duck eggs, I tried experimenting with those for a while some argue duck eggs are a little easier. quail eggs I played with those a little bit. You know, I can't say that I've noticed a huge difference among the different types of eggs. But I think it's a cool experiment when you try to get into the reintroduction phase where you're going back to paleo 1.0 and adding eggs and things back in nuts. For me, same thing, I used to get really, really bad headaches from walnuts, so I cut those out for a while. If I do a little bit of those, I'm okay. So the good news is your body can calm down. And that's one thing that this diet will help you do is it'll help you to identify your trigger foods. Because if you're just eating a bunch of different stuff, and your diet is too varied, and if you're not tracking it, you don't have a clue. If you go and you have a salad, where you've got walnuts and pecans and cranberries, and tomatoes and whatever on your salad, you're not going to have a clue what's irritating you but if you go AIP for a bit, now you're going to know hey, you know what, as soon as I add it back in those tomatoes, boom, my joints hurt. And then you'll have a much, much more clear path. So if anything else, it's more helpful to use the journal plus reintroduce foods and it can be amazing. That's how you really figure out what you tolerate what you don't.
Dr. Justin Marchegiani: Yeah, I tell patients you don't really know how dirty you get until you get really clean. Right, once you're really clean, and then you get dirty, you're like, Okay, I get it. I'm dirty right now, right? What does that mean? We want a clean baseline. So what's the clean baseline? In my analogy, the clean showers the baseline. And in regards to the food, that's the autoimmune diet, the autoimmune diet is the clean shower, it's getting really clean. So then when we start to one, maximize the diet, usually people are going to see benefit within a within a couple of weeks, and or a month, and I always like patients to kind of plateau, some or plateau within three, four weeks, where they may see a lot of improvement and joint pain or energy or brain fog. And then it's like, Okay, good. Now they're kind of like running out of steam in regards to their initial jump and improvement. So I want patients to typically be on the diet for four weeks and the plateau for at least one week before they do any reintroduction, some autoimmune patients, they continue to see significant improvement week after week, and it may last a couple of months. So patients that are like that, I'm a little bit more strict on what they're under reintroduction. Now, it's usually not that big of a deal. Because if you get those kind of results, those results speak for themselves, and they really motivate you a ton. So it's not like twisting an arm to get someone to follow that diet longer, because the results are guiding us that we're on the right track. So I tell my patients, if you're gambling and you're on a streak playing poker, or blackjack, I'm not going to pull you off the table. Right? I'm going to let that streak roll a little bit. Same thing with the diet. So if you have a lot of success coming out of the gates, I'm gonna let it roll. I'm gonna let you plateau. And then we have a specific reintroduction protocol, and how we add foods back and I'll go into that in a minute.
Evan Brand: Yeah, well said and, you know, there's not a lot of money involved with this, meaning you can't really make money just by getting people to eat meats and veggies. So the problem is, there's not too many studies. Now I don't know if you want to pull it up, but I just sent you one in the chat. For those watching on video, they may be able to see this. It's a PubMed study here. It was in the inflammatory bowel disease journal 2017. As I mentioned, there's not much money in this right. So it's probably going to be few and far between clinical trials on autoimmune diets because there's no drug involved and Big Pharma isn't going to pay some random guy to do a diet trial. Right. But anyway, this was a study on patients with Irritable Bowel Disease. And they did it for six weeks, followed by five week maintenance. And it just goes into the results here it talks about significantly improving people with ulcerative colitis, and significantly improving Crohn's disease. C reactive protein, they said didn't change much. But the calprotectin, which is a marker we measure on the stool panel, it improved from 471, which is high was to 112 at week 11. And also Wow, those that did drop. I mean, that's a lot. I mean, you're talking hundreds of points, just put died alone. And then it says here among those with follow up endoscopy at week 11. improvements were also noted in a simple endoscopic score for Crohn's disease and a Mayo endoscopy sub score. So we're not obviously running that we're not doing scopes on people, we're running stool panels. But I've seen the same thing. I had a guy who had calprotectin above 1000, it was insane. He had pan colitis where it was the whole colon and you know, pretty much the whole intestinal tract was involved. It was pretty sad. But just with now, technically, in his case, we didn't do just diet, we did a lot of really, really potent aloe extract. But I mean, we were able to get calprotectin down hundreds and hundreds of points within a few weeks. So there's the proof.
Dr. Justin Marchegiani: 100% those are all excellent points. So a couple people in the chat here Andrew Hill wrote in that we got to be careful with tapioca because it's a similar cassava similar to latex and yeah, if you're a sensitive person, we may want to even cut that out for a few weeks before we add that in. Technically that may be allowed, right cassava yuca, tapioca. And that same kind of family. I think it's the same thing. There's different names, but that may be something we want to work on excluding others may just be some of the spices, you know, like pepper, some of the nuts or seeds or spices that are something that you don't eat, but it's more of a topical kind of thing on the food. Got to be careful over that if you're really sensitive, usually foods going to have a dose dependency. So the more of that food you eat, the more the immune reaction will be exacerbated due to its we keep an eye on those things for sure. Riley wrote in that we know basically one of the no take on the food sensitivity test, when does a food sensitivity test become beneficial? So my issue with food sensitivity tests, is most of them come back with some level of autoimmune foods on there for people. Okay, that's number one. So I always look at test, does it change the treatment? So most are going to have some of these foods on there, number one, number two, if it doesn't have those foods on there, would a patient still benefit from cutting those foods out? That's the important question, because your immune system may be responding in a way outside of a typical IGA G or IGA test. There are other tests out there that look at like the MRT or the Alliance akt look at other type of T cell intermediary responses, which could be it. But I still know people that run these tests and they have patients that test perfect for gluten. And then now you're in this conundrum is do you allow your patient to eat gluten now because the test says gluten is fine, because we know there may be an immune response happening in the body outside of what's being tested. So that's why I don't like it because you can give a lot of false sense of security that you can eat gluten or other grains. Number two, I've seen benefits cutting those foods out, even when it says it's fine. So for me, it doesn't change what I'm doing enough for the value for the cost. And I'd rather use that money on another lab or a stool test or supplementation that's going to be more root cause supportive.
Evan Brand: Well said, I'm going to take that as my soundbite. So anytime somebody says, Evan, why won't you run a food sensitivity test dummy? I'm going to say, Well, my good friend, Dr. Justin said it better than me, and then I'm going to play them your little soundbite you just did because it was it was so good. But I agree. And that's exactly what what I do is I just tell them, Look, save your money. Let's go AIP. And then let's do reintroductions plus you journal. And we find that that's going to be far better. I mean, when you look at gluten, for example, I have seen people where it does show up as that it's going to be okay. However, they know when they eat it, they don't feel as good. They feel a little brain fog, they feel bloated. And that didn't show up on paper. So then they're confused. And then the husband goes, See, I told you you're crazy, eat a pizza, and then you just get yourself in trouble again.

Dr. Justin Marchegiani: So yes, now where food allergy tests may be helpful. It doesn't quite fit into the patients that I see is if a parent is trying to help a child and or a family member who is totally on is totally uncompliant and resistant to doing anything. And if we can get some lab data saying to avoid these foods, that may help with leverage, but most people are coming to see us they're they're investing a lot to work with us. So they're pretty darn compliant. If we say don't do that, let's save you some money. They just typically listen to us. Yeah, well, number two is if you're already at a great, great super high level of health, and you want to see if there's any maybe weird foods there, then that may be helpful to look and see if any other foods that are there. The problem is if it says don't eat raspberries, and then you eat blueberries, what's the chance that blueberries and now on the list next month? Right? That's where it becomes this like whack a mole where you're like, wow, like one and the other one pops up over here. And you're like, crap.
Evan Brand: That's a very good point. Yeah, the compliance and the leverage. I mean, that's the reason that we do some of the testing in regards to the infections too, because somebody will say, Hey, I feel like I've got this, I want you to just give me a parasite protocol. I think I've got parasites with you know, you and I've covered this before people come in, and they have this idea of what they think's wrong with them. And we, they just want us to pursue that rabbit hole with them. So we'll come in and we'll use the data first look on the paper. You know what, actually, no, we think this is a bigger priority over here. And then we circle back. So yeah, that's that's a great point.
Dr. Justin Marchegiani: Absolutely. So I think it's, uh, you know, we want to always look at you know, the root cause why you're sensitive to these foods, of course, you want to be fixing the gut that's gonna be ideal. Whether it's SIBO or H. pylori of bacterial issues, you want to work to the six hours because patients have a chance of having increased risk of food allergens when the food's not broken down properly. So adequate levels of enzymes and acids chewing your food masticating your food Well, not overly hydrating when you eat adequate enzymes, adequate acids are all very helpful at being able to break down the food again, if you love it, rotate it. If you're eating beef every single day over and over again, your chances of a beef allergy goes up right but you saw the study I just mentioned earlier, that study showed much less chance of animal products and vegetables causing an allergen right so that we cut out the big foods that are going to be the highest risk. Now. Outside of that there's a reintroduction plan that I infuse with my patients when it's time. So we add each food back in over a two to three day period. So we'll start with egg yolks before eggs ghee before butter, one not one seed one Nightshade at a time. And typically a very small amount of food on day one, a little bit more on day two. And if we have no negative symptoms, then usually we're good we can go to the next food if we're on the fence, we can have a day three where we eat a larger amount of food because the response tends to be dose dependent small amount of bad food for you. Small amount of symptoms, larger amount of food, larger amount of symptoms and then if you stair step the dose up usually the symptoms go up as well. So if you're on the fence, it gives you that ability to be confident that you're sensitive or not. And we go right down the list.
Evan Brand: Yeah, so give me a little bit of concrete like view how would that look? So today's Monday when we're recording so let's say you want to add back in almonds for me you're gonna have me do what have you?
Dr. Justin Marchegiani: Yeah, so let's just start in the right order. So egg yolks before eggs, so I may go and I may poach one egg, poach it, it comes up. I'm keeping the yolk a little bit soft. Why I don't want to oxidize it. I trim away the egg white egg white tends to be more allergenic, feed it to my dog, have the yolk How do I feel? That's a good if I do. Okay, let's do two yolks tomorrow. Trimming away. Good. Excellent, great. Awesome. Very good. Next day we're going to add in the full egg. Now we're going to do a little omelet, right, but we're not going to overly, we're not going to overly cook up the egg yolk, the egg white, I'm sorry, we'll keep it so it's, you know, the whole eggs blended but it's going to be a little bit more wet because we don't want to overly oxidize the cholesterol on the proteins that are in there. Right? oxidized cholesterol and protein tend to be more hyper allergenic higher immune response. And then if we're good there, then we go to gi waggy. Keys, clarified butter, less lactose, less casein, right? The casein and lactose have the biggest problem. If you can tolerate ghee Great, now we go to butter The next day, same kind of stairstep so my sensitive patients can handle ghee can't handle butter. So we always want to start with the least allergenic to the most. So if we can handle one egg yolk but not the egg, guess what we at least have an egg yolk in our diet. If we handle the egg, the GI but not the butter we at least have some of that good butterfat clarified gi back in our diet. So we always go least to most, where if we did it the other way around. You wouldn't have been able to add the food back in.
Evan Brand: Yeah, that's great. Okay, and then when do you bring in some of the nuts, the seeds? How do you do those any particular order you found better or worse.
Dr. Justin Marchegiani: So I would just start with like, if you're gonna do almonds, you could just do one or two almonds, right? And IDN sprouted is a little bit better, right where it's soaked, and that can deactivate some of the anti nutrients, the lectins, the phytates, right, the oxalates. So you can do a couple of almonds, maybe one teaspoon or tablespoon almond butter. And the next day you can double or triple that dose. See how you feel if you're okay, that's a good sign. But of course, deactivating some of the anti nutrients can be helpful too. And then the next day, let's say pecans are in your routine. Try pecans, try pistachios or walnuts. And again, if if you're not eating those foods on the reg, it's not that big of a deal, right? Just try to choose the nuts or seeds that are more on the regular things that you're doing more on a daily routine.
Evan Brand: And of course we want to make sure these are organic. We want to make sure these are fresh. I advise keeping your nuts in the freezer like I keep my pecans in the freezer. And they taste so good frozen to like I'll take pecans out of the freezer do a little bit of maple syrup. Oh my god, you talk about delicious.
Dr. Justin Marchegiani: Oh totally. Yep. 100%. Now here's the other deal too. So then we have let's say you're able to get nuts or seeds or nightshades or eggs back in right you get everything back in. Do we ever allow grains now I always just tell patient it depends on how significant a patient is. If we know someone has diagnosed autoimmune condition I always try to stay more on the grain free side I hate the word gluten free because you can be gluten free and eat lots of process rights and oats and corn and that could be a problem right? Because the problem means are are the umbrella the problem? You know umbrella gluten is one prolamin under that umbrella, right? The most common one is the wheat, barley and rye that gliadin prolamin. Then you have horizen in which is rice, you have a vignette which is oh right you have seen what you have seen which is corn. So these are still like brothers and sisters of the Glee and protein. So just like someone you may see someone, a brother or sibling, and you may be like, Oh, you must be so and so you look just like him as a family resemblance. Well, your immune system has that same kind of resemblance with other proteins that are cousins and brothers and sisters of gliadin. And so your immune response can be triggered. Also, there's a lot of data in the non celiac gluten sensitivity research that grains, even if you're not allergenic to them can still increased gut permeability. And the more you increase gut permeability, the greater chance you have of creating more inflammation or triggering autoimmunity. Now, what does that mean? Does that mean never eat grains? It just means my general recommendation is always try to be grain free if you can have a substitute. If you're relatively healthy, good health and you have no autoimmunity. Could you eat some grains that have gluten here, they're probably you could probably get away with it, you know, and it probably wouldn't be that big of a deal. I wouldn't recommend it being a staple because those foods, they're still inflammatory. They still have a lot of nutrient blockers in there. And they still aren't nutrient dense. So I still much rather, I'd much rather see someone have some white potato over a bunch of wheat, right potato is actually pretty nutrient dense and has a lot of potassium in there and a lot of good minerals. I rather have someone do that over over gluten. Complete gluten full, if you will, grains, but it all depends where you're at, the healthier you are, the more versatility and adaptation you have, the more unhealthy you have or the more diagnostic autoimmunity you have, you really want to be careful. A lot of times it's just not worth it. Some people they eat some gluten, they're inflamed for a week, it takes them days to get back on the wagon. So it depends upon how long it takes you to get back on the wagon. And if you have a known thyroid issue, there's some data saying that autoimmune response can last for weeks and even months so it's just not worth it depending on the damage that may occur. Dude after the fact.
Evan Brand: Yep. Well said and yeah, he's talking about like the gluten cross reactivity issue. So like, for a while, you know, I had a lot of people doing corn because they thought, Okay, I'm gonna, I'm gonna be okay. But turns out they weren't. Okay. So in a lot of cases, yeah, we do remove the corn if I do a much rather see
Dr. Justin Marchegiani: much rather see cassava or you could chips over anything with corn or anything else like that. So that's much better like this yet they brands pretty darn good. Or just a really good white potato chip like the boulders make a good one with avocado or coconut oil that's really good fat. On the potato side.
Evan Brand: I've noticed the same thing. Yeah, potato for some reason, even though it's still potentially cross reactive. I've noticed it is better tolerated than corn for most people. So that's good. Maybe it's just a lower count or maybe a slightly different compound in there.
Dr. Justin Marchegiani: Exactly. And I use a lot of root vegetable chips. So I'll do like a lot of turnips, rutabaga, or sweet potato, like a lot of root vegetable, like grain free type of stuff. And that tends to be pretty good. But the nice thing is, once you kind of work through that autoimmune template, you should get a lot of confidence in what you can or can't handle. And then once you're at a high level, if you're if you're going off the reservation too much, you'll start to feel it. And that usually gives you a pretty good idea that you're probably doing too much for you. So our goal is to get you feel really clean. And then once you're really clean, it's kind of easy to notice when you're getting dirty.
Evan Brand: Yep, yep, well said. And the whole point of this is what well, it's to give you relief is to get you to feel better is to get your brain to work better your joints to feel better your sleep to be better your food reactions, your gut, your, your everything. I mean, the skin, the brain, I mean, this literally can affect every body system here. So we really want to focus on what's the end goal. It's not just tweaking this just to tweak it make this like an obsessive OCD type thing because it can get a little crazy. No, it's to get you to feel better. And then while we get you to feel better, we're working behind the scenes on these other root causes. Because it's very unlikely that someone became sensitive to all these foods just out of nowhere, right? There's something that triggered it. And Okay, so we're getting you simmering, okay, we got your diet, just you Okay, we got that pillar of the house in now, while that's sitting there, simmering. Let's work back here. We're going to work on this, this this over here, and then boom, now we go back to this diet. Good job, you've been holding steady. Okay, now let's bring normal quote normal things back in and then people tolerate him. So that's kind of the whole rationale. That's kind of our mindset behind this whole thing. When we're working clinically. It's not just the dietician, approach. Here's the diet have a good life? It's okay, well, why did you have to go to this level of specificity in the first place? And that's the real question.
Dr. Justin Marchegiani: Exactly. And also, people want to start having more grains on the regular, I would say make sure your health is really great and stable. And I'd also say if you wanted to be more certain, run an HLA dq test for gluten sensitivity, if you have to or ate on there, you definitely want to avoid the gluten, one or three is going to be a little bit less. And then I think four is the only true genotype that is not gluten sensitive, you could still have other problems with the anti nutrients that are in there, or the higher amounts of fermentable carbohydrate, but that'd be my one test that would say just to really know that make sure there's not a genetic issue. If you're going to put it in there and more in the regular for me, my big cheats are going to happen. If I go out for sushi, I may have a couple of rolls. But usually I like the Alaskan roll that has like a lot of salmon, and a lot of avocado, and then there'll be a little bit of white rice. So when I typically cheat, it's going to be getting some white rice for sushi. And but I typically use coconut aminos and a soy free soy sauce and MCT oil and I'll typically do extra enzymes and extra charcoal during those meals to mitigate the inflammatory response. So it's a kind of couple of little tricks that I kind of do. If not for me, I just I just feel too good. I don't want to have a setback. So there's enough substitutes for me where I can engage in that substitute still feel really good and not have a problem?
Evan Brand: Yep, they are. Well said.
Dr. Justin Marchegiani: Anything else you want to add Evans? Oh, one more thing. I wanted to say. What if autoimmune paleo is not enough? What does that mean? So some patients they may have to do carnivore, they may have to do a variation of an autoimmune paleo, low fodmap SCD template where we're cutting out fermentable, carbohydrates, even some of these really good fermented foods. Or we may have to be cutting out foods that are high in salicylates and females, that may have a little bit higher amount of anti nutrients that, you know, things that could be on the vegetable side, right, or fodmaps, like broccoli, and let's say onions and garlic, things that are have good benefits, we may have to cut out other foods. And again, we see a lot of patients that come in that have done a lot and that are very sick or have a lot of gut inflammation, we may have to go to that extreme. We may even have to do an elemental diet or a carnivore diet. So everyone's a little bit different and they come in from different places. But if an autoimmune diet does not work for you, there's other things that we need to work on it. You'd really want to work with that practitioner at that point, because your health issues are a lot more nuanced.
Evan Brand: Yeah. And hopefully you're not hopefully you're not to that level. But just know that if you've done this and you're still suffering The number one, there's probably underlying triggers you haven't identified yet things that are really aggravating your immune system or the gut. So we need to try to find those triggers. And then number two, you can tweak this thing even more to get you stable, the whole thing, the whole goal is to get you stable. So we can work on root causes here. So it's not just diet and done, just remember that.
Dr. Justin Marchegiani: 100%. And also, what's the goal of this diet, right, I always tell patients, what's the goal is that we don't have like a goal in mind. Most people, when they make a diet change, they kind of just go to this place in their hand, like it's forever. And they kind of have like a little mini funeral, like how I miss my potatoes, my, or my seeds, they kind of have this really this kind of state of mourning, where it's really sad and they're depressed, I always tell my patients, the goal is to one first, increase your nutrient density in your diet, number two, to decrease inflammation overall, right, and then three, to decrease a lot of the toxins, whether those toxins or plant based toxins, whether those toxins are you're not eating organic, and you're getting pesticides, and chemical toxins, all those things are valid. And the goal of that is that now decreases the immune system stress, and that the immune system stress starts to go down. There's less autoimmunity, there's less inflammation in the body. And that kind of starts creating this snowball effect where your body can start to heal as we start addressing infections, supporting the adrenals addressing nutrient deficiencies, calming down the immune response by addressing infections and using probiotics and other nutrients on that side of the fence.
Evan Brand: Yeah, you made a great point, which is the emotional piece. So we could do a whole part two podcast on this if people want. We're going into the whole rationale scientific part of that. But if you've got a woman who is addicted to her cookies, you've got to work through the emotional stuff, too, right? So we could come in with all these rational, very scientific studies and things you have gone into, right? It sounds really attractive and really scientific. But then you got the emotional bubbles popping up. And people are going Oh, no, but what about this? And what about Thanksgiving? And what about this and my family and I love to do go eat the popcorn at the movies, you know? And so then the emotional piece is hard. So you have to work through that with people. And we do we have those conversations. So on the face of it, it sounds all easy, right? It's like, okay, just boom, boom, boom, boom, boom, you're great. But then, once you actually sit down at the plate, and you've got that fork there, then the emotional stuff comes up. It's the the husband or wife making fun of you for your choices. I mean, that's a common one. It's if there's a divorced family, it's the child going to the other part of the family, where the other family member doesn't believe in this and say, This is all quackery. And then they come home after eating pizza all weekend, and then they're in an autoimmune flare, or you go over to the parents house. And, you know, they think it's a joke. So they still try to serve you bread and butter, you know. So there are some things you have to work through on the family emotional side, but you know, it's definitely something that's, that's possible. Everybody can do it.
Dr. Justin Marchegiani: Yeah, where I see it a lot, you know, well, meaning grandparents that feed their kids cookies, their grandkids, cookies, you know, or like, they want to spoil them a little bit. That can be really tough, too. But yeah, you got to get everyone on the same page. And in general, you got to have a plan. And if you're having a lot of cravings, most of those cravings, a lot of the protein orphans, which are like opiate like compounds in grains and dairy hit that same opiate receptors. So those foods can have a lot of addictive qualities to it. And a lot of people they're used to operating on a blood sugar rollercoaster, so their blood sugar goes up and down, up and down. Because not enough good protein or fat in the meal or they're not, they're going too long between meals. So really working out the blood sugar. A lot of times if someone switches from a standard American diet to an autoimmune diet, the two big mistakes they make is one, they're not getting enough calories from their autoimmune diet, therefore, they're chronically hungry, which creates cravings. So you have to make sure you're getting enough calories or nutrients. The second thing is they may go to low carb for them. So if someone's needs a little bit more carbs, and they're at a relatively more healthy way, they may come in go really to low carb, and that may cause more cravings too. So you may have to just add in some good, healthy, safe starches to fill that carb void if those carbs are a good place for you. My default set is always lower carb, higher fat, and then kind of work through that over time, because most people have more insulin resistance and going lower carb out of the gates helps resolve a lot of that.
Evan Brand: Good points. Good point. Yeah. And the gluteal morphin stew. I don't know if you said I think it said the other thing that
Dr. Justin Marchegiani: Yeah, the protein orphans are gluteal morphemes. These are like the opiate like products like that are in gluten or the KCM orphans in the dairy.
Evan Brand: Yeah. So when people say oh my god, I'm addicted to my whatever, they're not joking. You literally are and there can be some sort of a withdrawal from it. And then also from the neuro transmitter perspective, that's something we're going to look at on organic acids testing. So if we see for example, whether it's low endorphins, low dopamine, low serotonin, we may come in with specific amino acids to try to repair and rebuild. And that can be a good let's call it a nutritional support band aid for the brain chemistry, which is causing the underlying craving in the first place. So rather than say, hey, go from the gluten cookie to the grain free cookie, it's okay. Yeah, maybe you do that. But we're also going to give you a little bit of some DLP a or trip the fan or something to help the brain because the brain is involved with this too. This is not just the gut, the brains involved too. So we're, we're thinking about all these variables as we go. It's kind of a moving, it's like, I don't know, maybe a good NASCAR analogy, you know, it's like the, the guys are coming on and changing all the tires and we're doing that in every category. So it's the brain, it's the gut, it's the immunity it's the adrenals we're we're simultaneously working on all of these pieces and then boom, you succeed you feel better. So I think we should wrap it up if you're ready too.
Dr. Justin Marchegiani: I think we can't man that we did a great job kind of outlining everything this will be a good reference for my patients as well that you know, just kind of want more intel on the autoimmune side. If you're listening to this and you want to dive in deeper and you're feeling a little bit overwhelmed with some of the diet changes out of the gates definitely reach out to myself for Evan, EvanBrand.comand there's a little link there where you can click the schedule or myself Dr. J. At JustinHealth.com we're happy to help you. We have experienced doing this for over a decade with thousands of patients. And if you're ready to take that next step, we're here to help you all if not just utilize all this free information and just kind of execute on it and make yourself healthier. We really appreciate it.
Evan Brand: Yeah, if you're a do it yourselfer, that's fine. But for me, and you and many others, it's better to have a guide, it's better to have the data test don't guess get the information, know what you're up against. So you can figure out and when we say test, don't guess we're talking the root cause stuff. We may not run a food panel out of the gate, but we're gonna run a gut panel out of the gate figure out what infections could be causing these issues in the first place. So thanks for tuning in. We appreciate you guys and we'll be in touch.
Dr. Justin Marchegiani: Put your comments down below. Let me know your success on an autoimmune diet. Really want to know and thanks for sharing. You guys. Have a good one. Take care of y'all.
https://justinhealth.libsyn.com/autoimmune-protocol-the-paleo-way-podcast-312