
Abdominal discomfort can be frustrating and even debilitating. With so many potential causes, identifying the root of the problem can be challenging. Whether it’s indigestion, acid reflux, or a bacterial imbalance, understanding your symptoms is the first step toward relief.
This comprehensive guide explores the most common causes of abdominal discomfort, their symptoms, and holistic solutions from a functional medicine perspective. By addressing the root causes, you can take proactive steps to improve your digestive health and overall well-being.
Pain on the left side of the abdomen is often related to stomach issues, but pancreatic conditions can sometimes mimic stomach discomfort. While stomach issues are generally linked to digestion, pancreatic disorders such as pancreatitis or pancreatic cancer require urgent medical attention.
Understanding the difference between these conditions is essential for proper diagnosis. Stomach-related issues often involve bloating, acid reflux, and mild to moderate pain, while pancreatic problems may present with severe pain radiating to the back, unexplained weight loss, and jaundice. Seeking medical evaluation is crucial if symptoms persist or worsen.
Dyspepsia, commonly known as indigestion, is discomfort in the upper abdomen that often occurs after meals. Symptoms include bloating, nausea, and a burning sensation.
Low stomach acid (hypochlorhydria) is a common cause of indigestion. Many people mistakenly believe heartburn is due to excess stomach acid, but low acid levels can contribute to poor digestion, acid reflux, and bacterial overgrowth.
Simple ways to support digestion include consuming bitter foods to stimulate acid production, avoiding excess water intake during meals, and incorporating apple cider vinegar before meals.
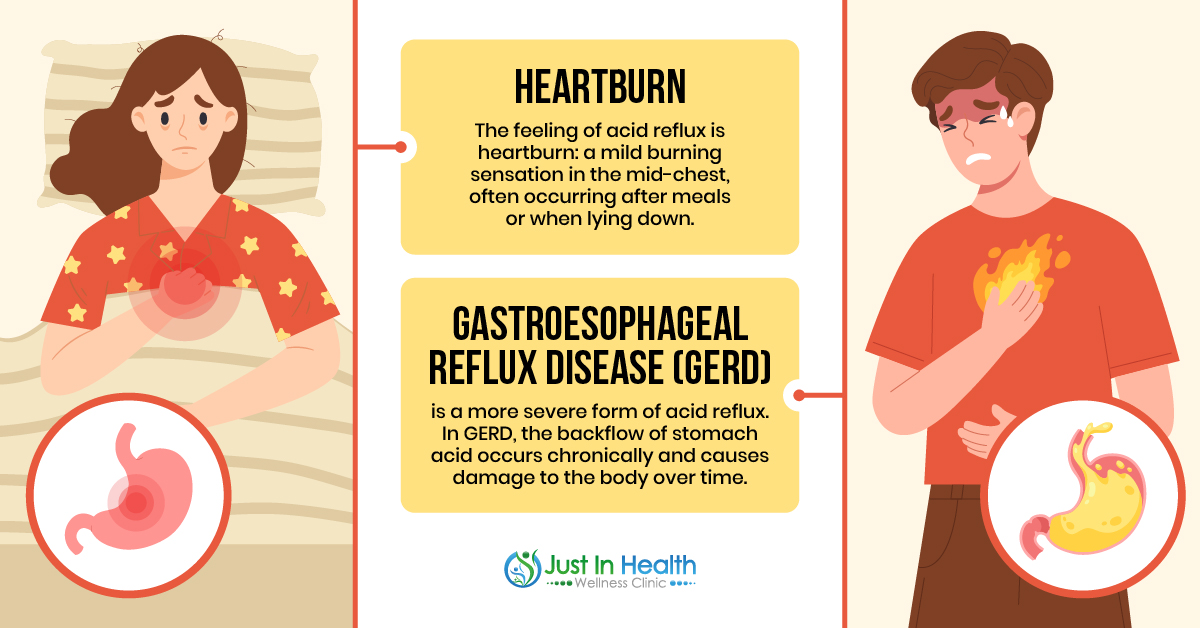
Heartburn is a burning sensation in the chest caused by stomach acid moving up into the esophagus. Chronic heartburn can develop into gastroesophageal reflux disease (GERD), a more serious condition that can damage the esophagus.
A weakened esophageal sphincter allows acid to escape, leading to inflammation and discomfort. Certain factors, such as obesity, pregnancy, and specific medications, can contribute to a weakened sphincter.
Natural ways to reduce acid reflux include avoiding trigger foods (caffeine, alcohol, spicy foods), eating smaller meals, and sleeping with the head elevated to prevent acid backflow.
A hiatal hernia occurs when part of the stomach pushes through the diaphragm into the chest. This condition can lead to acid reflux, chest pain, and difficulty swallowing.
Contributing factors include obesity, pregnancy, and frequent heavy lifting, which increase abdominal pressure. A hiatal hernia can weaken the esophageal sphincter, exacerbating heartburn and indigestion.
Holistic approaches include visceral manipulation therapy to help reposition the stomach, breathing exercises to strengthen the diaphragm, and smaller meal portions to reduce pressure on the hernia.
The location of stomach pain can provide clues about the underlying issue.
H. pylori is a bacteria that can cause inflammation and ulcers in the stomach lining. While many people harbor this bacteria without symptoms, some experience stomach pain, nausea, and bloating. Treatment typically involves antibiotics and acid-suppressing medications.
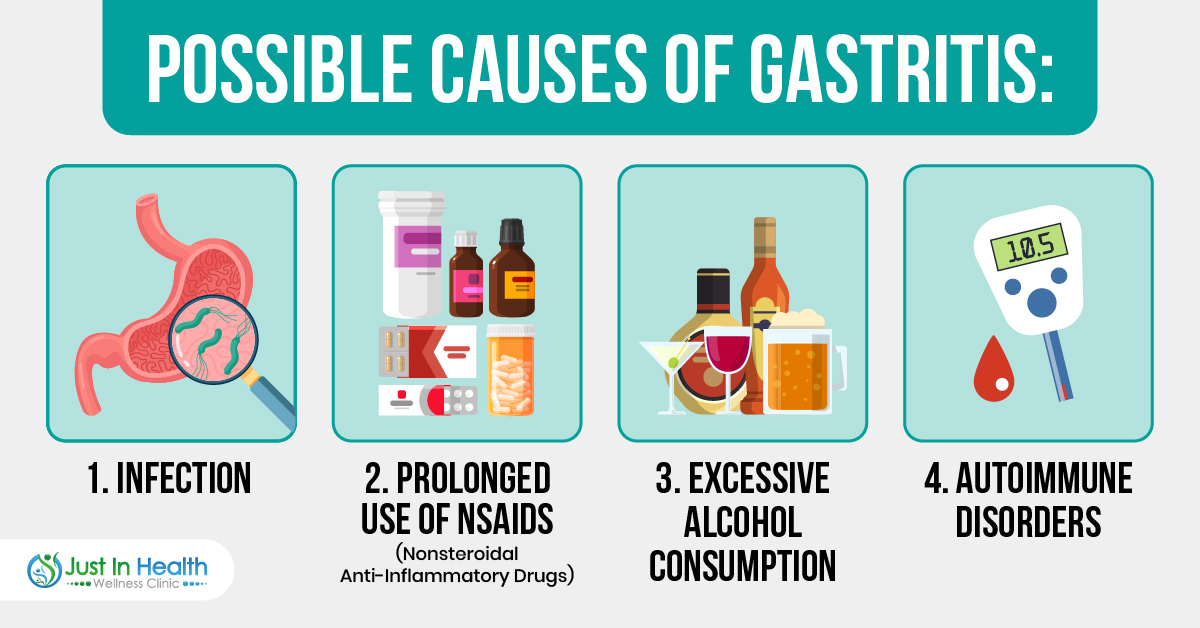
Gastritis, an inflammation of the stomach lining, can be triggered by chronic NSAID use, excessive alcohol consumption, or autoimmune disorders. Symptoms include nausea, stomach pain, and a sensation of fullness. Holistic remedies include avoiding irritants, drinking chamomile tea, and taking probiotics to restore gut health.
Chronic stress has a significant impact on gut health. It slows digestion, reduces blood flow to digestive organs, and can increase stomach acid production, leading to heartburn and gastritis.
Managing stress through breathing exercises, yoga, and regular sleep can help improve digestion and prevent stress-related digestive issues.
Small Intestinal Bacterial Overgrowth (SIBO) occurs when bacteria multiply in the small intestine, leading to bloating, gas, and diarrhea. Candida, a type of fungal overgrowth, can develop due to high sugar intake, antibiotic use, and a weakened immune system.
Addressing bacterial and fungal imbalances may require dietary changes, herbal antimicrobials, and probiotic therapy to restore balance in the gut microbiome.
Functional medicine approaches include visceral manipulation therapy, dietary modifications, and targeted supplements to support digestion. Increasing fiber intake, avoiding processed foods, drinking bone broth, and staying hydrated can all contribute to better digestive health.
Abdominal discomfort can stem from many causes, including indigestion, heartburn, bacterial overgrowth, and stress. Identifying the root cause is essential for effective treatment.
Integrating holistic remedies such as dietary changes, visceral manipulation, and stress management can restore gut health and achieve long-term relief. If symptoms persist, consult a healthcare provider for personalized care.
How can I tell if my stomach pain is severe?
Seek medical attention if you experience severe pain, unexplained weight loss, vomiting blood, or persistent symptoms.
Can stress alone cause stomach pain?
Yes, chronic stress affects digestion and can lead to bloating, heartburn, and gastritis.
Are probiotics helpful for indigestion?
Yes, probiotics restore gut bacteria balance, improving digestion and reducing bloating.
What foods should I avoid for heartburn?
Caffeine, alcohol, spicy foods, and citrus fruits can trigger acid reflux.
What natural remedy helps with acid reflux?
Aloe vera juice and chamomile tea can soothe the esophagus and reduce inflammation.
========================
“Functional Medicine Approach to Chronic Disease” by Mark Hyman, M.D.
“Gastrointestinal Diseases and Disorders: Diagnosis and Treatment” by James S. Scolapio, M.D.
“Indigestion: Diagnosis and Treatment” by Nimish Vakil, M.D.
“Helicobacter Pylori: Physiology and Genetics” by Harry L. T. Mobley, George L. Mendz, Stuart L. Hazell.
“Gastritis: Causes, Diagnosis, and Treatment” by Peter Malfertheiner, M.D., Ph.D., M.Sc.
“The Role of Gut Microbiota in Health and Disease” by Emad M. El-Omar, Ph.D.
“The Gut-Brain Connection: How Stress Impacts Digestive Health” by Emeran Mayer, M.D.
“Small Intestinal Bacterial Overgrowth: Roles of Antibiotics, Prebiotics, and Probiotics” by Grace L. Su, M.D.
“Visceral Manipulation in Functional Gastrointestinal Disorders” by Jean-Pierre Barral, D.O., P.T.
“Hiatal Hernia: An Overlooked Cause of Disease” by Steve Rochlitz, Ph.D.