
H. pylori, short for Helicobacter pylori, is a bacteria that affects the stomach lining. It can lead to digestive discomfort and potentially more serious conditions like ulcers and gastritis. Despite being one of the most common infections worldwide, many people don’t realize they have it. If left untreated, H. pylori can contribute to chronic digestive issues and even increase the risk of stomach cancer.
This article will explore H. pylori symptoms, how it spreads, testing options, conventional and natural treatments, and prevention tips to help you restore your gut health.
H. pylori is a bacteria that primarily infects the stomach and small intestine. More than half of the global population is estimated to carry this bacteria, though not everyone experiences symptoms. The bacteria sometimes weaken the stomach lining, leading to inflammation (gastritis) and even painful ulcers.
Many people live with H. pylori for years without noticeable issues, but for others, it can cause persistent digestive discomfort and serious complications.
H. pylori symptoms can vary, with some individuals experiencing mild discomfort and others dealing with chronic digestive problems. Common symptoms include:
✔ Abdominal pain or burning sensation (especially when the stomach is empty)
✔ Bloating and excessive burping
✔ Nausea and vomiting
✔ Loss of appetite
✔ Frequent acid reflux or heartburn
✔ Dark, tarry stools (a sign of internal bleeding)
In some cases, H. pylori can trigger symptoms beyond the digestive system, such as:
✔ Unexplained weight loss
✔ Fatigue and low energy
✔ Chronic bad breath (halitosis)
✔ Iron-deficiency anemia
✔ Brain fog and dizziness
If you’re experiencing any of these symptoms, getting tested to determine if H. pylori is the underlying cause is essential.
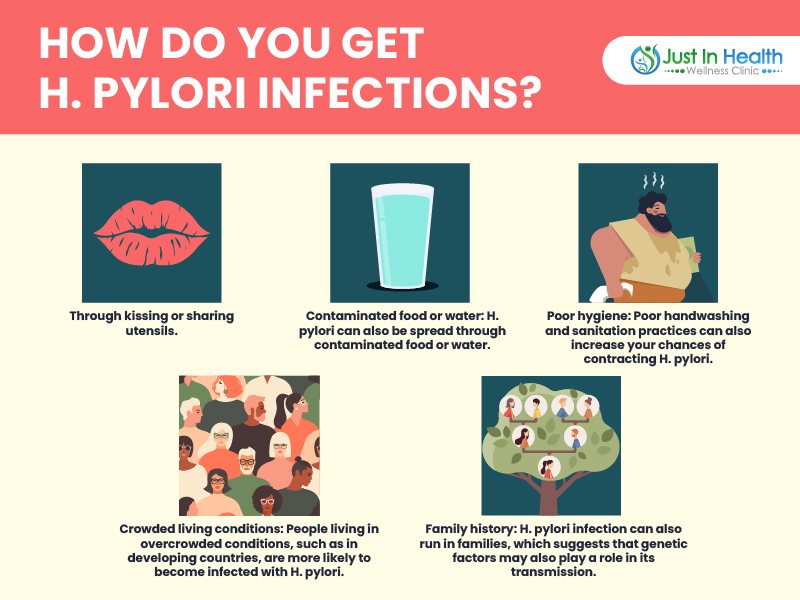
H. pylori is highly contagious, and most infections occur in childhood. The bacteria spread through:
🔹 Person-to-person contact: Kissing, sharing utensils, or coming into contact with saliva or bodily fluids.
🔹 Contaminated food or water: Eating or drinking from unhygienic sources.
🔹 Poor sanitation: Not washing hands properly after using the bathroom or before handling food.
🔹 Close living quarters: H. pylori is more common in crowded households, particularly developing countries.
Yes! H. pylori can be successfully treated with the right approach. However, because the bacteria are known for antibiotic resistance, treatment must be carefully planned.
Standard treatment usually involves a combination of antibiotics and acid-reducing medications to eliminate the bacteria and allow the stomach lining to heal. However, antibiotics only work about 70% of the time, and recurrence is common if the underlying causes aren’t addressed.
Many people turn to functional medicine and natural therapies alongside standard treatments for a more effective, long-term solution.

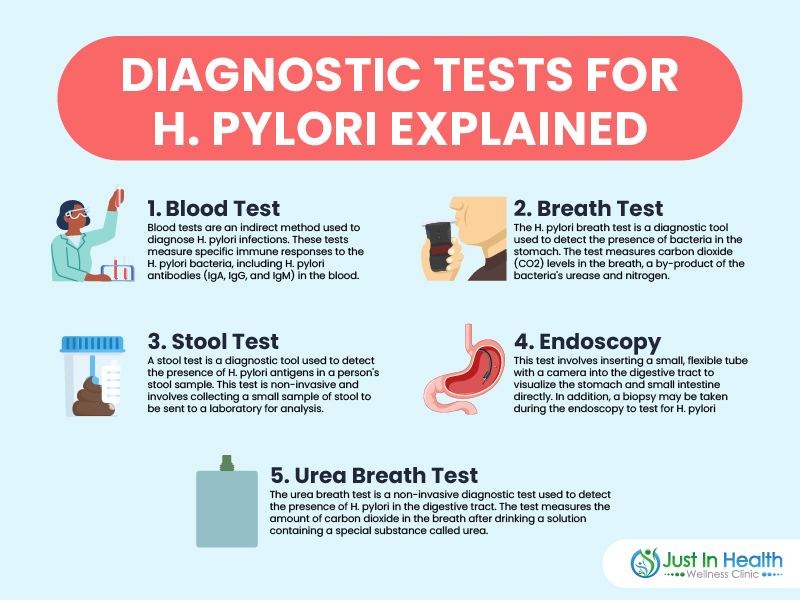
If you suspect you have H. pylori, testing is the first step toward recovery. Here are the most common methods:
A simple blood test can check for H. pylori antibodies and indicate whether you've been exposed to the bacteria. However, it cannot confirm an active infection.
A highly accurate, non-invasive test that detects H. pylori by analyzing the carbon dioxide levels in your breath after drinking a special solution.
A stool antigen test detects H. pylori proteins in your stool, making it a reliable way to confirm an active infection.
For more severe cases, a biopsy may be performed during an endoscopy, where a small camera examines the stomach lining, and tissue samples are taken for testing.
🔹 Triple Therapy: The most common approach, involving two antibiotics and a proton pump inhibitor (PPI) to reduce stomach acid.
🔹 Quadruple Therapy: For antibiotic-resistant cases, doctors may add a bismuth-containing drug to strengthen the treatment.
While these methods can be effective, they don’t always work due to growing antibiotic resistance and may have side effects like nausea, diarrhea, and disruption of the gut microbiome.
Many people prefer natural alternatives to help eradicate H. pylori while promoting overall gut health. Some science-backed remedies include:
✔ Probiotics: Support healthy gut bacteria and help fight off H. pylori.
✔ Garlic: Contains natural antibacterial properties that combat infections.
✔ Ginger: Reduces inflammation and aids digestion.
✔ Manuka Honey: Has powerful antibacterial effects that may help fight H. pylori.
✔ Aloe Vera: Soothes the stomach lining and supports healing.
✔ Broccoli Sprouts: Contain sulforaphane, which has been shown to kill H. pylori.
Making simple adjustments to your diet and lifestyle can greatly improve treatment success:
✅ Eat an anti-inflammatory diet (lots of vegetables, healthy fats, and lean proteins).
✅ Avoid trigger foods (spicy foods, alcohol, processed sugar, and acidic drinks).
✅ Drink plenty of water to flush toxins from your system.
✅ Manage stress levels with meditation, deep breathing, or yoga.
✅ Prioritize sleep to support the immune system.
A holistic approach combining medical treatment with natural remedies and lifestyle changes can lead to faster recovery and prevent recurrence.
Since H. pylori is highly contagious, taking precautionary measures can lower your risk:
🚰 Drink clean, filtered water to avoid contamination.
🧼 Wash hands thoroughly before eating and after using the restroom.
🥗 Eat a well-balanced diet to maintain a healthy gut microbiome.
🚫 Avoid sharing food, drinks, or utensils with infected individuals.
🏡 Improve home hygiene by keeping kitchen surfaces and bathrooms clean.
H. pylori infections are common but treatable. If you're experiencing symptoms like bloating, acid reflux, nausea, or stomach pain, it's crucial to get tested and start treatment early.
Combining conventional treatments with natural remedies and lifestyle changes can provide the best results for eradicating the bacteria and improving gut health.
If you're struggling with H. pylori symptoms, don’t wait—schedule a consultation with a functional medicine expert today!
Need help eliminating H. pylori? Click here to book a free consultation with Dr. J! 🚀💊
====================
Recommended Products