
HCL (Hydrochloric acid) activates pepsinogen into the enzyme pepsin, which then helps digestion by breaking the bonds linking amino acids, a process known as proteolysis. Enzymes break down proteins, cellulose, starches and other foodstuffs. This makes it possible for the intestines to absorb nutrients. Enzymes begin thedigestive process in the mouth, as they're secreted by salivary glands. They work to break down starch into sugars.
Dr. Justin Marchegiani and Evan Brand address some topics around digestion in today's podcast and also talk about various digestive supports. Learn more about the importance of hydrochloric acid and enzymes needed for digestion. Find out why and how the conventional model does not succeed in getting to the root cause of digestive issues.
 This interview really is all about the bases and the foundations of digestion but also touches upon the subject of gallbladder issues and other gut inflammation that can be avoided with proper digestive support. Discover how you can optimize your HCl levels and learn about the various enzymes that help in the digestion process as well as find out what the role of bile salts are.
This interview really is all about the bases and the foundations of digestion but also touches upon the subject of gallbladder issues and other gut inflammation that can be avoided with proper digestive support. Discover how you can optimize your HCl levels and learn about the various enzymes that help in the digestion process as well as find out what the role of bile salts are.
In this episode, topics include:
00:56 digestive issues and digestive support
8:09 gallbladder stones, flushes and surgery
10:51 hydrochloric acid doses
13:35 enzyme support
16:25 gut infections
![]()
Podcast: Play in New Window|Download
Dr. Justin Marchegiani: Evan, how are we doing today, man?
Evan Brand: I’m doing great. What about you?
Dr. Justin Marchegiani: Doing pretty good. Actually just got back from San Francisco. Nice little week up in the Bay Area and back to a nice hot weather here in Austin, Texas. Nice hot summer.
Evan Brand: Yeah, it’s–you can tell that it’s slowly sliding into fall here in Kentucky and I’m not ready for it yet.
Dr. Justin Marchegiani: Imagine the foliage. It’s probably awesome up there.
Evan Brand: It is when it turns. It hasn’t turned yet. In another month or so it’s gonna be crazy beautiful.
Dr. Justin Marchegiani: That’s great. So we talked before the show about addressing some topics around digestion. Especially how to use various digestive supports. I got a email question this week where a patient wanted to–want–wanted me to elaborate more on this topic. I think this would be a great topic to discuss today.
Evan Brand: Yeah, absolutely. Everybody–not everybody, but a lot of people have digestive issues and that’s kinda where I like to start with people most of the time. If you fix that, you fix a lot of other stuff.
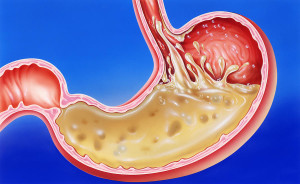
Dr. Justin Marchegiani: Yeah, so regarding digestive issues, there are various digestive supports you can use to help. So HCl or betaine HCl, various enzyme support products whether it’s like protease or lipase or trypsin, like protein or fat digesting enzymes. And then there are things like bile salts which can also be helpful for emulsifying and breaking down fat. So those are kinda like our 3 that we’re gonna contrast with today. So the first foundational one is HCl. And again HCl can vary depending on how much you need, anywhere between 1 to 3 or 4 grams per meal, and HCl is really important because that HCl really helps lower the pH in your stomach and that nice low pH activates a compound, a proteolytic enzyme called pepsin. It takes it from pepsinogen which is inactive to pepsin which is active. And when it’s active, it really starts to hold protein digesting process. So we need this nice low pH in our stomach and that nice low pH activates these protein digesting enzymes and that starts the digestive process and that nice low pH mixes in with all the food and that’s–this is called chyme and that chyme then gets released into our small intestine and without that nice low pH, we don’t get that trigger from our pancreas and gallbladder to release bile salts from the gallbladder, and then various enzymes like trypsin and proteolytic enzymes–that means protein digesting, and then also lipase, fat digesting enzymes. So again, this whole domino rally here of kind of, you know, what has to happen first, second, third, really happens with hydrochloric acid.
Evan Brand: Yup. And hydrochloric acid, if people don’t know, is a good thing. This is a time where acid is more is better most of the time. People may have this idea from the mainstream media––I just a commercial the other day that still makes me gag about Zantac and all these other Nexium and all these companies competing on who has the best acid blocker and 99.9–and correct me if I’m wrong–99.9% of the time, the issue is too low stomach acid and not too much and people that have like a faulty lower esophageal sphincter from stress or whatever, that could actually cause some of that acid to sneak back up into the esophagus where you don’t want it to, but if we have the HCl levels optimized, that could prevent some of that stuff from happening.
Dr. Justin Marchegiani: Yeah, one of the big feedbacks for it, that esophageal sphincter, that’s where the part of your stomach and your esophagus meet. One of the main mechanisms for that esophageal sphincter tightening is nice high levels of hydrochloric acid, but also keeping dysbiosis down in the stomach. So it’s one of these things where if we have inadequate levels of HCl in the stomach, well, we start to have bacterial overgrowth because food sits and rots and ferments and putrefies in the stomach and then part of that whole putrefaction process and rancidification fermenting process, we have various organic acids that rise off of that and then because everything is disrupted, that esophageal sphincter is left open and those acids will rise up and actually burn that lower part of the esophagus and the upper part of the stomach creating inflammation. And then you go to your conventional doctor and they say, “Oh, you have esophagitis or gastritis,” right? All you have to do is just break down the medical speak. Cut the word in half. Esophagitis or gastritis, stomach or esophagus, -itis meaning inflammation. It’s like, well, wait a minute. I already know those inflammation there, right? If you have pain in your throat, it’s probably esophagitis. If you have pain a little bit lower, it’s probably gastritis. The question becomes now, what’s the cause? Now your conventional doc will just throw a–an acid-blocking medication like Nexium or Prilosec or omniprazole, etc. But again, what’s the underlying cause? We already talked about the fact that lack of acid will create this environment where this food rots and then the esophageal sphincter stays open and organic acids rise up. So if you know that mechanism, giving a medication that’s blocking the acid, actually makes the problem worse. So when–once you have this biochemical physiological understanding, you can see how the problem is actually being made worse in the long run. You may get symptomatic relief in the short run but you have a massive amount of other problems because now you can’t ionize minerals. You can’t break down protein optimally. There’s gonna be more dysbiosis, more gut infections because we don’t have the ability to sterilize the environment so now we’re set up for a whole host of long-term issues.
Evan Brand: Yeah, and I’m trying to think of a good analogy. I know you–you’re always killing it with those, but it’s almost like blaming the firemen for the fire.
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: Does that count as an accurate analogy for that situation?
Dr. Justin Marchegiani: Yeah, that makes sense. I mean, most medications are designed to manage symptoms and there’s nothing wrong with that like in the short run. You know, a day or two, right? But the problem is when symptoms are managed and you have the false expectation that the underlying cause was fixed, that’s where problems become long-term because then now you’re stuck using this long-term and then because the–your whole gut physiology is screwed up, you can’t come off it. And the conventional medical model is really about managing symptoms and then essentially you get hooked on these drugs because the symptoms now once you come off are now really bad and you just–you can’t–you can’t deal. Any comments on that, Evan?
Evan Brand: No, I think that’s a great overview of how the conventional model once gain does not succeed in getting to the root cause of digestive issues.
Dr. Justin Marchegiani: Yeah, and these medications, I mean, they’re like in the top 5 every year. These proton pump inhibitors.
Evan Brand: Billions.
Dr. Justin Marchegiani: Yeah, billions, top 5. I mean, right next Synthroid and–and Lipitor. I mean, they’re–and your anti-depressants. They’re right up there in the top 5 every year and like I–the analogy I kinda tell my patients–you know, when you’re stressed and you’re taking these medications, they’re really lessening or they’re really taking off or–or turning off your force field. So imagine like the Star Trek ship, it’s got that nice force field around it so when the Klingons come in there and attack, it’s got the force field up and it can –it can defend itself but when we lower our hydrochloric acid levels and things come into our environment, we’re not gonna be able to mount an attack against it.
Evan Brand: Great. Yeah, I was hoping you would navigate into that territory. What happens then once that acid level is low over a period of time? It’s not just the crappy digestion, it’s not just the burping and the heartburn, indigestion. It’s not all that. It goes way deeper and that’s kinda what you’re alluding to now is that other stuff downstream, these next dominos in line, those get messed up, too, and you run into all sorts of things like biliary stasis, gallbladder issues, and all that.
Dr. Justin Marchegiani: Yeah.
Evan Brand: So I don’t know if you wanted to move down south, down the system, and talk about that now.
Dr. Justin Marchegiani: Yeah, if we don’t have enough hydrochloric acid, that nice low pH and all that chyme, which is just mixed up food, right? If you don’t have that nice low pH, our gallbladder isn’t triggered to contract. And if we’re not contracting that gallbladder, bile salts sit too long in that gallbladder and aren’t being emptied periodically, kinda like changing the oil in your car, things can get really grimy and get sludgy and that can potentially create a stone over time. And these stones then at some point when you eat a fatty meal, that gallbladder contracts, it’s like wrapping your hand around a porcupine and squeezing. It’s not gonna be a–a good situation.
Evan Brand: That’s a good one. Let’s–if you have–if we have a minute here, I wanna talk about gallbladder flushes real quick, because I know a lot of people do those and they read about them like drinking like a cup of olive oil at the end of a fast and I just, I get asked about that and I just think it sounds crazy. So I don’t ever have a complete answer on it.
Dr. Justin Marchegiani: Yeah, I’m not a huge fan of doing that off the bat. There may be a desire and a need for that down the road. But if your digestion isn’t working and you’re not breaking down food and then you go do this big flush and there potentially is a stone in there, and that gallbladder is contracting because of all the olive oil and/or apple juice you’re taking in, and that gallbladder contracts down around that stone, right? Visualize yourself grabbing a porcupine and squeezing, that there could be some inflammation and you may end up going to the ER, and then you’re gonna be pushed to have that gallbladder taken out always.
Evan Brand: Mmm.
Dr. Justin Marchegiani: I mean, I’ve saved hundreds of gallbladders just because gallbladder issues are almost always due to food allergens and a combination of low level stomach acid which, you know, may be driven by even a deeper infection, but definitely the food and the stomach acid off the bat is the first perfect storm element that really sets you up for gallbladder issues.
Evan Brand: Wow. Yeah, gallbladder surgery. It’s ridiculous how common it is, act like it’s just as simple as getting some stitches on a cut. “Oh, yeah, let me just pull your gallbladder out real quick.”
Dr. Justin Marchegiani: Oh, I know, I mean, I wonder–I wonder if most of these medical doctors had the same kind of mindset like if we dealt with our car, like if we just say, “Hey, you know, you’re having a little bit of a issue in your car today with this issue. Let me pull open the hood. “Yeah, oh yeah, what’s this thing right here? Let’s pull it out.” You know, I–I guarantee you they’d be a little bit more selective over their car but when it comes to their patients, they’re just like, “Yeah, let’s pull it out. It’s not working.” I say, “But why? And is there anything we can do conservatively to prevent that?” Like–
Evan Brand: Incredible.
Dr. Justin Marchegiani: Some of the things we talked about that are virtually free.
Evan Brand: Yeah, we can’t make billions. We could talk about all these supplements and we’ll never make billions off of these things. I mean, a bottle of hydrochloric acid is gonna be less than 30 bucks, you know, so it’s just insane.
Dr. Justin Marchegiani: I know and on that note, hydrochloric acid is a powerful supplement to start off it with anyone that has chronic health issues. Typically, how we dose it is we start off with 1 capsule per meal and I like to take it in the middle of the meal. Why in the middle of the meal is because, well, if you have gastritis which is that gut inflammation, right? Gastro meaning stomach, -itis meaning inflammation. So if our gut lining is thin and we’re inflamed and we put a nice hydrochloric acid capsule right against that mucosa and it starts to dissolve, well, it’s like touching a scab on your hand or on your arm. It’s gonna be more sensitive. So we take it in the middle of our meal, kinda like an Oreo cookie. It’s like the cream filling, not–not at the beginning, not at the end. And we start off with one and we take it at breakfast, lunch, and dinner. We see how we do and then each day we work up to 2, to 3, to 4. Again, there’s this whole idea, we can go up to warmness or HCl tolerance. That can be good. I’m–I’m also very careful of going above 4 or 5 capsules just because I don’t wanna cause a–a ulcer in the small intestine. So it–this called duodenum, that’s where the stomach connects in with the small intestine. When all that acid goes into the duodenum, our pancreas has to make a whole bunch of bicarbonate to start to neutralize that acidity. So if we’re jacking it up really high where we’re doing 8, 9, 10, 11, 12 capsules per meal and you’re not still feeling warmness, I get a little concerned because I don’t wanna cause a duodenal ulcer. So 4 or 5 tend to be a pretty good place that I stay at for patients, especially if they’re seeing a benefit of foods feeling lighter. They’re feeling like it’s digesting. They’re having, you know, better bowl movements. They’re having less burping or gas. We’ll stay at that 4 or 5 mark. I don’t like to go too much above that unless we’re closely monitoring them.
Evan Brand: Yeah, I got nothing to add there. That’s great advice and I typically take 1. I’m great with 1 but I’m still one so I’m still producing a–a decent amount for now.
Dr. Justin Marchegiani: Uh-hmm. Yeah, yeah.
Evan Brand: Until I get older.
Dr. Justin Marchegiani: Yeah, exactly.
Evan Brand: Like an old man.
Dr. Justin Marchegiani: Uh-hmm. And it–hydrochloric acid levels do go down with age, so we gotta keep in mind that because a lot of, you know, elderly patients, they’re having all these bone issues and osteoporosis issues and it’s like, “Man, like, you know, Boniva and all these other medications are not gonna fix the issue,” because a lot of times it really starts in the digestive system. We’re just not breaking down and ionizing these minerals and we need good levels of hydrochloric acid to ionize minerals, so we can absorb them into our bloodstream and utilize them.
Evan Brand: I don’t know if you agree with this, but to me, optimizing HCl levels to me is probably one of my top 3 to 5 foundational things I could ever do for somebody.
Dr. Justin Marchegiani: I couldn’t agree more, 100%.
Evan Brand: So–
Dr. Justin Marchegiani: Now the next thing on top of that is we’ll also add in enzymes and depending on how–how chronic or how long someone has had gut issues, I either use a combination product with enzymes and hydrochloric acid together with bile salts for my patients that aren’t doing too bad. Like patients that have more chronic issues, we’ll separate them out because a lot of times their gut lining is thinner. They have this gastritis issue where that gut lining has been worn down and they will only be able to handle maybe 1 or 2 hydrochloric acid capsules. But they’ll need a lot more enzymes. So if we package the enzymes together, we kinda hit the wall sooner, because we only can do 2. Where if we have the enzymes separately, we can go up to 3, 4, 5 enzymes per meal and it’s just the enzymes, and because the enzymes aren’t as abrasive we can hit a more therapeutic level with them and have better protein and fat digesting or digestion capacity even when the HCl has hit the wall at a 1 o 2 state.
Evan Brand: Interesting. So sometimes, people can get away with just enzymes and they won’t need the hydrochloric acid and combination with.
Dr. Justin Marchegiani: Yeah, I mean, I typically recommend enzymes separately but we’re still giving HCl by itself.
Evan Brand: Right, okay.
Dr. Justin Marchegiani: So like, we may hit the wall at 1 for instance. Some of my chronic gut issues, they’ll hit the wall at 1, but great, I mean, that doesn’t meant though you’re getting enough enzymes, well, we’ll work on upping the enzymes separately to 3 or 4 or 5 and seeing how we do. And some patients even after that, if I see a lot of fecal fat in their stool test, we’ll even add a separate product by itself that just has high amounts of lipase which is a fat-digesting enzyme and high amounts of bile salts. And with my chronic gut issues, we can–my chronic gut patients–by this combination here of combining HCl and enzymes or HCl enzymes and fat digestive support, we can get their body’s ability to break down some of these nutrients better which buys us time to start getting the gut and the adrenals fixed because if we absorb better nutrients, if we absorb the nutrients from our good diet better, we’re gonna be able to use those nutrients to help heal our body and then if we get to the underlying adrenal stuff, infections, dysbiosis, SIBO, etc., we’re gonna be able to fix this problem long-term so maybe in 6 months or so, we can pull them off from of these digestive support products as long as they’re managing their stress and–and eating well.
Evan Brand: Great point, yeah, and I see that people wanna self-diagnose themselves or they’ll zoom in on this tiny, tiny problem. But sometimes we can’t get to those tiny problems if we don’t zoom out and hit on the foundation that’s going to help improve that tiny problem downstream where we may not even need a specific protocol for X, Y, Z tiny problem because we fixed–we zoomed out and fixed the big thing that’s at the top of the chain.
Dr. Justin Marchegiani: Absolutely, and a lot of my patients have H. pylori infections and H. pylori is this gram-negative bacteria that actually produces toxins called lipopolysaccharide or endotoxins, but it also produces an enzyme called urease which takes the urea which is a by-product of protein metabolism, right? Protein’s di–protein digestion primarily happens where? In your stomach. So it takes that urea and metabolizes it into CO2 and ammonia. Ammonia has a pH of 11, so it will actually lower your stomach acid levels, meaning it will raise the pH, right? Remember low pH, 2 or so, is where you’re–where you’re nice and acidic, where your stomach should be so it will actually raise the pH, okay? And that will make your stomach acid levels go lower, alright? Don’t get that confused, so when pH goes up, stomach acid levels go lower, so it’s kind of an inverse opposite thing and that will affect your body’s digestion. So we can’t just give HCl or enzymes and just say, “Hey, the problem’s fixed, even though I’m feeling better.” Because if there’s an infection, especially H. pylori, we gotta get to the root cause.
Evan Brand: Yeah, what’s your favorite for that? Do you like the breath test?
Dr. Justin Marchegiani: Breath test can be helpful and what’s the breath test looking at? It’s looking at an excessive amount of CO2 essentially. Well, why CO2? Well, we just mentioned, right? What’s the mechanism? Urease from H. pylori takes the urea and pumps it out to ammonia and CO2. So it’s the–the by-product of what the H. pylori is doing. It’s what’s making the CO2 go up. So breath test can be helpful. We’ll look at stool antigen and stool PCR, which is stool DNA. And then we’ll also look at blood which is IgG, IgM, and IgA and that’s kinda looking at an immune response to the H. pylori. But I like the–the stool the best. That’s gotta be my favorite, PCR and stool antigen which are great. So we’re looking at a piece of the DNA and we’re looking at a piece of the actual infection in the stool.
Evan Brand: Nice.
Dr. Justin Marchegiani: Anything you wanna add, Evan?
Evan Brand: No, I’m loving it. Keep going.
Dr. Justin Marchegiani: So I find a lot of conventional docs, they miss the digestive support element and even the functional medicine docs, they miss the digestive support element or they don’t hit it at a therapeutic level, that’s step 1. And then step 2 is they miss that deeper underlying infection. And a lot of times, it may not just be an H. pylori. It may be an H. pylori, a parasite, and a fungal issue. So I see a lot patients because you know, candida programs are really pop–you know, popular these days, or they’re just doing a candida program but they have candida, but they also have an H. pylori infection and a parasite, and again, H. pylori and parasites, they’re more on top of that pyramid in our infection hierarchy where it’s kinda like if you just knock out the candida, it’s like pulling grass out at the surface–I should say, it’s like pulling a weed out at the surface. If we don’t get to the root, that weed’s gonna grow back so a lot of people are treating gut issues even SIBO for instance, but there’s a deeper issue underneath at the root that may be an H. pylori or a parasite, and all the SIBO programs and all of the candida programs may not be enough to get to the root issue.
Evan Brand: Great, yeah. Great point, and once again, cookie cutter doesn’t work, that’s why you need a practitioner to do this stuff. It gets–it gets complex sometimes real quick.
Dr. Justin Marchegiani: Yeah, I know you have a lot of experience, too, so NotJustPaleo.com as well as JustinHealth.com if anyone’s like thinking about this and like, “Alright, you know, I’m gonna try some of this HCl. I’m gonna try this.” If you wanna dig in deeper and see if there’s any other root causal issues, that will be your next step to–to dig in at least ensure there’s nothing else lingering under the surface.
Evan Brand: Yup.
Dr. Justin Marchegiani: Anything else you wanna add, Evan?
Evan Brand: No, I think this is a great overview. I think we can make it a lot longer, but there’s no need to because we have covered the bases and the foundations of digestion pretty well, so good job.
Dr. Justin Marchegiani: Yeah, you, too. And I think, you know, what we’re specializing is really foundational information because you can get minute and you can do this study or that study, or this isolated nutrient or whatever, but again, if the foundation isn’t there, people aren’t gonna benefit. They aren’t gonna get better so I hope people just walk away with a good foundational take home and also, remember one thing. Hydrochloric acid, taking HCl is not gonna lower your own production, okay? So that’s a good thing. It’s not like taking testosterone where your–your, you know, the organs act–that make testosterone actually shrink, right? You’re not gonna have that issue so with taking HCl, it’s not gonna affect our body’s production of it. It actually takes the stress off our gut so we can actually heal. So kinda keep that in mind, too. If we take some of these things, even long term, it’s not gonna hurt our own internal production. It’ll actually only help it.
Evan Brand: Great point. Yeah, I’m sure a lot of people are questioning that. Is it safe long term? And the answer is yes.
Dr. Justin Marchegiani: Yeah, because the–the main signal for HCl production is gastrin and they’ve done studies looking at gastrin levels while on HCl over periods of months and time, and the gastrin levels did not drop while on HCl which is good.
Evan Brand: Yup.
Dr. Justin Marchegiani: Alright, Evan, man, hey, great talking to you, bud.
Evan Brand: Yeah, sounds good. You, too.
Dr. Justin Marchegiani: Bye.
Evan Brand: Okay, bye.
[retweet]