
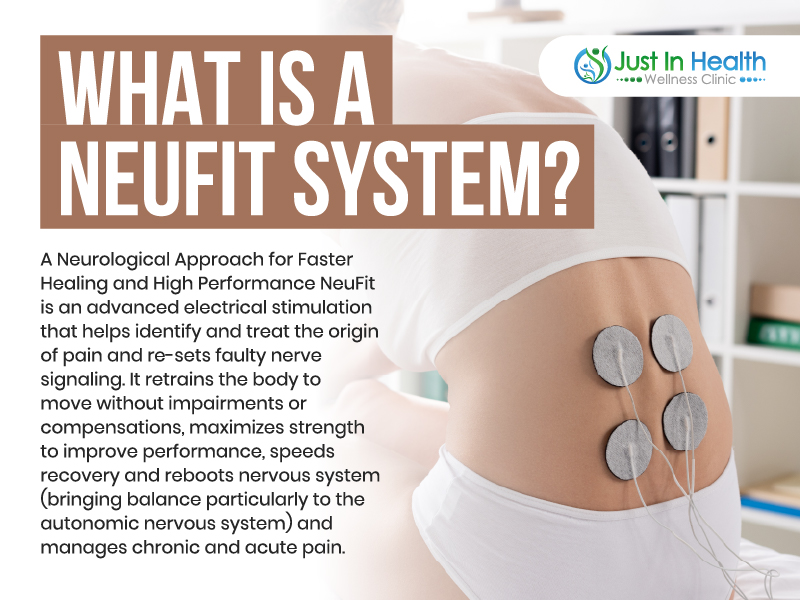
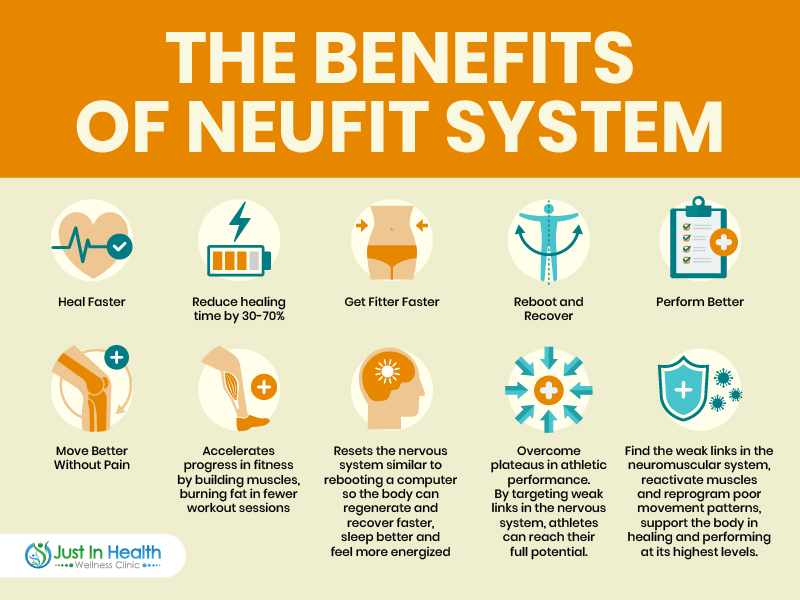
In this video, we have Dr. J and Garret Salpeter, the founder of Neufit Technology. Performance and recovery go hand in hand when training or doing physical activities, regardless if you’re an athlete or not. The Neufit Method improves performance and muscle health and optimizes recovery. Further, this video will tackle optimizing performance in fitness, improving the recovery process, and breaking down the significance of The Neufit Method.
Garret Salpeter emphasizes that even if you are not an athlete, you should know how to let your body rest, heal, and recover properly from any form of injury or physical activity. Everyone has their activity levels to maintain. It may not be sports-related, but everyone demands effort from their bodies on a day-to-day basis.

Dr. Justin Marchegiani
In this episode, we cover:
0:00 – Introduction
4;49 – What makes The Neufit Method different?
7:48 – The neurological response to injury and trauma
17:12 – The link of soft tissue of mobilization and nervous system
21:35 – The recent add-ons of Neufit Method
32:31 – Foundational diet changes to improve healing
Dr. Justin Marchegiani: Hey guys, it’s Dr. Justin Marchegiani here. I am with Garrett Salpeter, who is a CEO founder of NeuFit technologies down in Austin, Texas. Garrett is a great friend, as well as, an amazing colleague and he’s got a new book that we’re gonna chat about today. So, I’m gonna go through some of the, I think, the biggest take-home items that anyone listening can use to help accelerate their body’s ability to heal and perform better. Really excited to have Garrett on the podcast today. Garrett, how you doing man?
Garrett Salpeter: Thanks, Justin. It’s awesome to be here. Great getting to catch up with you before hopping on here and, uh, I’m excited to be on and appreciate the opportunity to talk about the book.
Dr. Justin Marchegiani: Awesome. Very cool. Love the graphics, love the cover, um, really nice, really enticing, been kind of going through some of the aspects of the book different parts of the book. What was the process of, you know, your last ten-year journey writing this book? I mean, do you just kind of go through and think about your biggest clinical wins with patients like how do you kind of go in and get this thing moving because there’s so much that you can talk about over the last 10-12 years of seeing thousands of patients? How do you go about and just start crystallizing that?
Garrett Salpeter: It’s, you know, it’s an interesting process. It’s something that was on my mind for a while like for a couple of years before I finally decided to start and then I worked on it, you know, in early morning hour before the kids woke up and in evenings and you know, so I worked on it off and on again for a couple of years. The original catalyst for doing it was a combination of two things: one is people telling me hey you know you gotta write a book to share you know you here all these great stories about how these technology helps these create these miraculous recovery stories and then what really motivated me to finally do it is I kept getting ask by people like hey where can I read more about this, hey where’s the book in this and I my answer until recently was well it’s you know stuff that I’ve learned by combining reading textbooks and combining different mentorships and workshops and experiences that I’ve done in the field of physical therapy and functional neurology and pedagogy and physiological psychology. And so, there wasn’t a place where everything was kind of brought together in one way and so that was a big motivating factor for me was to have a resource, to be able to share with people and then, um, and then I kind of fell into this trap of making it, you know, just going like super deep on all these areas that I’m interested in. Originally, the first version of the book was probably too dense and academic and so I had written, you know, I’d got to get up in the morning for an hour before the kids wake up and write this over the course of, you know, a year and a half probably. Got to 130,000 words, which is like a, you know, a huge like a thick textbook encyclopedia type thing. And then, we finally, you know, we’re talking with our team about hey what’s gonna be the most valuable thing that we can offer to people and we decided that it would be something that was more accessible that more people, you know, clinicians and lay people alike would be able to read and so I worked with an editor to help break it down from, you know, from 130, 000 words to 60, 000 literally like cut it half and then this is the finished product.
Dr. Justin Marchegiani: Very cool. Because I know you started off your PhD in this type of field in exercise physiology, human performance and a lot of, uh, electoral physiology technology and how it connects to healing. So, you kind of had this thesis kind of in mind and took that and kind of translate it back into a handbook that people can apply kind of day in day out for performance. So, it’s a big shift at the doctoral level, back to the everyday human level.
Garrett Salpeter: That’s right. It’s been kind of interesting thing, you know, like that it’s very true what I describe to people when ask me for the book before this was out was, you know, I’d say it’s a kind of this breadcrumb trail that I’ve been following through the research and these different disciplines and as part of my journey in trying to piece together this knowledge base in a meaningful way that can be beneficial clinically and in all these different settings, you know, part of my journey like I was so passionate about learning about this stuff and that I ended up going back to school into this neuroscience based PhD program in emphasis in motor control and I ended up ultimately leaving that in order to launch our product and, you know, do the other things that I’m doing now but we have a PhD neuroscientist who’s our director of research now, who’s been able to do that even better than I could or would. So, that’s great but, yeah, I mean, I literally have had to go all these different directions to piece it together and it’s just, you know, it’s very exciting to be able to come back full circle and package it together into a book like this that draws on all those different disciplines.
Dr. Justin Marchegiani: Yeah. Very cool. Because how I first came across you before I moved down to Austin is I found a lot of your YouTube videos online. And one of the things that struck me was you had a lot of these, you know, stories, this kind of timeline, um, situations. Where someone would come in with an injury and you would kind of timeline their ability to heal over 2 or 3 months or so of major injuries that would take six months – twelve months and I was blown away with the idea that you could take people that hey this injury according to conventional orthopedics is a one year to finish to heal and you would take these people and get their injury recovery time down in half or even 60 or 70% faster. I thought that was amazing and it kind of sold itself that hey what you’re doing is working and so that was pretty cool. Can you talk about, you know, some of the tenets that you are applying that you were applying that was allowing you to do better than what the conventional PT, Orthopedic surgery route was?
Garrett Salpeter: That’s a great question and that is, is kind of like, okay what’s the special sauce, what makes it different and that’s one of the biggest themes in the book that we talk about is making this distinction between hardware and software, between how most typical therapeutic interventions, most traditional physical therapy orthopedic medicine, is focused really enamored with and obsessed with tissue and structure whereas, there’s a whole other side of that coin, right? There’s function like hardware and software. The software, the function, which is of course is controlled neurologically is so often overlooked and ignored in these traditional models. And we’ve found that being able to prioritize the neurological response to injury and trauma is a huge catalyst for this breakthrough and a lot of it, is just as simple as, you know, look if you’re if your body naturally bracing and guarding and creating a bunch of tension around an injury, it can be impairing, blocking some of the blood flow and impairing the ability of the body to send nutrients and raw materials to heal there. So, the tissue of course that hardware component is important but the neurological response to injury is an impediment that blocks or delays that tissue healing process. By putting that first, by looking first at that neurological response to injury by finding where in the body it’s being imposed and resetting ang recalibrating that to an appropriate level, we’ve been able to open the floodgates if you will. So, the body’s natural healing process can progress without impairment and when it goes at its normal rate it’s not like we’re not doing anything we’re just allowing the body to heal and it’s just, you know, so if few people have been able to experience what the body can do when it’s really unleashed so to speak, that those faster healing times seem miraculous and really the miracle is in just removing those impediments, getting them out of the way and allowing the body to do it’s thing because it is a miracle.
Dr. Justin Marchegiani: So, essentially, conventional medicine they’re just kind of, they’re cutting out the injured inflamed tissue, there’s not really a lot of look at how that tissue got injured from a mechanistic standpoint then they hand them off to the PT that’s just stretching, typically stretching or strengthening that area without really looking at that whole chain. So, essentially, you’re looking at everything like it’s connected to the kinetic chain. So, you’re looking at all the muscles and the joints above and below, and you’re looking at the nervous system’s ability to recruit and stabilize those different areas. So, you have your Neubie device, so you’re using that as a means of one I think rehabbing and strengthening the muscle and the nervous, but you’re also using it as a means of detection. Can you talk about how it has dual purposes?
Garrett Salpeter: Yeah, absolutely. So, when we talked about this neurological response to injury and trauma, there’s the concept and then there’s actually the process of finding where in the body it exist and what it’s doing in the body and to understand what it is, one of my favorite metaphors is actually to talk about this notion of imagine a snake was, you know, come in, so I’m in my home office here imagine a venomous snake was coming into my office for me to react like this and you kind of run away or mobilize some energy so I can protect myself, that’s useful, that’s a valuable, you know, it’s a fear-based flight-or-flight response that mobilizes me to take action so I can you know fight or defend or protect myself or run away and flee and that’s valuable. However, if I react the same way to a rubber snake that my rubber snake that my daughter put there, that’s an over reaction that’s inappropriate. I’m wasting this energy, um, you know, trying to protect myself from something that’s not a real threat and our brains and nervous systems do this to us and you know forgetting these examples of like pain and injury for example. A lot of people have these experience, you know, thinking about someone who gets really nervous before they go public speaking for example, something like that. That’s the brain’s way of saying, hey this is life threatening we gotta protect you from this risk of being embarrassed because if you go out there and make a fool of yourself, you could get kicked out of the tribe for example, there’s like a deep survival fears associated with that. I think we all recognize that, you know, that fear is a kind of a hypersensitivity or it’s an overreaction or it’s a little bit mis calibrated to the situation like we recognize intellectually that we’re not really gonna die, if we go out on stage, because it feels like that because we’re overreacting. And the similar type of thing happens where, if we have an injury, you know, it’s football season, we’re working with a lot of professional and college and high school football players, you know, if an athlete goes out and sprains his ankle and they are totally shutting down as a response to that injury and that trauma, if they’re you know creating tension to lock down some muscles and totally shutting down others, that can be potentially productive if like if they were gonna roll that ankle again, it could that bracing could be protected there but if they’re not doing that if they’re trying to rehab and get to normal movements those patterns actually stand in the way, they delay that recovery process, they’re reacting, you know, as if they’re as if they’re pounding that ankle again, like there’s a real snake coming in when really it’s a rubber snake and they’re safe now, they just have to get themselves in the right state where they can heal. And by shifting by first of all identifying where so, to actually answer your question, if we’re able to take the Neubie device and scan around in their body, we can find where those hypersensitivity are in the nervous system where the brain and nervous system are shutting down muscles or creating these bracing and guarding patterns where they’re holding on in other muscles. We can find where those are and then send this very unique direct current stimulation to rest and recalibrate the nervous system and what does that really mean, well, it means, you know, an athlete who comes in with a sprained ankle who’s on crutches or can’t put any weight on their leg often times after that first session can walk normally it can load that weight, the load weight on their leg without pain and they make these amazing transformations in 15 minutes and you think, gosh, what happened to that 15 minutes. Did the ligament that was partially torn, you know, if it was a grade 2 and it’s a partial tear of the ligament, did that ligament heal in 15 minutes? No of course not. What happened was you reset and recalibrated those that suite of neurological protective patterns which some of which are tension, some of which are inhibition or turning off muscles and part of that is also pain. Pai is a protective output of the brain that’s part of that whole host of protective patterns and by resetting that, you immediately restore function back to a normal healthy level. They’re not ready to go back on the football field after that session, however, they’re in a state where they can move better, their muscles can better support that injured tissue as it heals and you’ve opened those floodgates, so healing mechanisms can actually work at their normal rate and do what their capable of doing.
Dr. Justin Marchegiani: What was always fascinating for me is when you would use the Neubie device to kind of search and scan the different tissue. Let’s say, you had direct pain on the knee, when you would search, you know, let’s say, from the hip down the quad right biceps femoris to rectus femoris into the calf, you would find hot spots or pain areas that would that the Neubie would pick up that you would perceive as pain but they wouldn’t necessarily be in the areas of pain. I think this is kind of what you’re taking about is conventional medicine would say oh I feel pain on the knee they’re focus on the knee. But you would scan it and you would get this feedback, that the patient would feel and they would feel areas of pain totally away from where that is. How does that happen, how does that work?
Garrett Salpeter: So, that speaks to a couple of these really powerful concepts like the difference between structure and function and also this notion that you talked about a lot about getting the root cause of the problem, right, you know, if you’re walking around all day and part of your quad muscles doesn’t work, you’re just kind of collapsing into that knee joint all day long and you’re gonna be setting yourself up for injury and you know eventually the knee starts hurting and you go and treat the knee but you’re not if you don’t go upstream and address that dysfunction or why it happened in the first place, you’re never gonna have a true long term resolution of the problem. And so, what the mapping allows us to do is to find where the dysfunctions are, which..
Dr. Justin Marchegiani: How do you measure that, like what’s the Neubie putting through like is there resistance in the tissue due to inflammation, lack of blood flow, like what’s causing that feedback at the tissue from a biochemical physiological level?
Garrett Salpeter: Ah, yes. So, the reaction, one of the things we’re working on is being able to measure some of these quantitatively and that so we should have some really cool information on that, you know, in the next couple of years as we build out our research program. What we know now, and what we’re identifying are areas where these exact neurologic protective mechanisms are present. So, what we’re doing as we’re scanning around, so if I have an electron pad, like this, and I’m scanning around the body what’s really cool about this current, so traditional first, we need a little context here so this makes sense, traditional electrical stimulation device is alternating current, tens units, Russian stim, they, when you turn them up to a high enough level to really make a difference, they cause muscles to contract and that becomes the limiting factor whereas with Neubie, we can at least to some degree, we can bypass a lot of that protective muscle contraction and speak more directly and powerfully to the nervous system. So, again, a little bit difference between structure and function, thinking directly about the nervous system. When we scan over the body, we’re sending a signal to the nervous system in the brain saying hey this area is being used, this area is being loaded, then we go here, hey this area is being used, this area is being loaded, here, hey, this area is being used being loaded. And wherever the body is working well, the brain sees that and says, you know, if were scanning it says oh that’s just Dr. Justin’s deltoid doing its normal thing, that’s just Dr. Justin’s biceps doing its normal thing. There’s nothing alarming about that, but if we stimulate a muscle or an area that either hasn’t been working recently because that habits or an area where one of these hypersensitivity and these, you know, these protective patterns that are being imposed on the body, if we scan one of those, the brain sees that and says whoa whoa whoa that’s threatening that’s alarming and it fights it, it reacts kind of a trigger point. If you were working on somebody and that you find that trigger point area that’s more sensitive. So, we find these areas of hypersensitivity and then we want to stimulate them and teach the, ultimately the brain, teach the brain and the nervous system that it can calm down that hypersensitivity. So, it’s, instead of you know, it’s like if you’re driving your car either you hit your throttle down harder or you can just take your other foot off the brake. Here, we’re trying to train you, you know, train your body to take the foot off the brake where it hand been imposing these limiting patterns.
Dr. Justin Marchegiani: Very cool. So, I know with the Neubie, unlike with your typical tens unit, right, you’re typically not gonna be exercising with like a tens unit, it’s like more like an electric aspirin. It’s kind of blocking the pain going into the brain. Here you’re actually able to move it in rehab. I’m just curious, a lot of different techniques in soft tissue world like Graston and active release technique, part of the reason on how they promote healing is they work on improving blood flow and they help release the fascia from the muscle belly. My experience using it, when I exercise with the pads on the various areas that in the current, I feel like there may be fascial release on that muscle helping to improve pain. Just curious, what’s your take on that fascia and the muscle kind of being mobilize and moving better?
Garrett Salpeter: This is really an interesting topic and there’s a few thoughts I have on that. One is people are doing manual therapy, it’s kind of this interesting..
Dr. Justin Marchegiani: I’m sorry just to add one little context. If this is my muscle belly, the fascia is like my shirt on top of it, so when tissue gets inflamed it’s like wearing a wet t-shirt it’s hard to get it off and so, just kind of giving people a visual imagine the we t-shirt on someone’s body that t-shirt is stuck and so helping to mobilize that t-shirt so to speak can help promote healing, go ahead.
Garrett Salpeter: So, there’s really, really important interesting connection between the movement of tissues and the function of the nervous system, so like in your example if that fascia or that shirt is glued down on the tissue underneath it, you miss out on that gliding and sliding between layers and you don’t get the neurological input from that area, so it goes out, you lose out on that, so the nervous system is this big feedback loop and all of the outputs of the nervous system which of course includes movement and pain. It also includes hormones, it includes heart rate and blood pressure, digestion like the nervous system controls our visceral organ function. So, all of these outputs of the nervous system that are relevant for health and cognitive performance and athletic performance and overall well-being. All of these outputs of the nervous system are vitally dependent on the inputs given to the nervous system and that can that of course is the things that you talk about in functional medicine, nutrition and diet and these lifestyle factors. It all absolutely to do with movement, also these neurological inputs of, including the tissues gliding and sliding over each other are super relevant for the overall health of the nervous system which is super important for the health of the overall body. So, being able to, there’s a few things that happen, being able to get movement in into those tissues is very important. A lot of manual therapists, when they say, you know, I’m releasing adhesions or I’m feeling this tissue move or something like that. A lot of what we’re learning is that, what they’re really doing is not making as much of those structural changes as they think, but they’re actually giving neurological inputs, the mechanoreceptors, the nerve receptors. They’re actually activating those to create more functional changes than structural changes and ultimately though, you need both, like you need the tissues to move over each other and you need to move them through enough ranges of motion to create the inputs so the brain gets enough inputs so they can maintain healthy function and get all the inputs it needs to drive appropriate controls of the body for movement and everything else. And when we’re working with the Neubie, you’re affecting both, you’re moving and affecting structures, you’re getting mechanical tension which can, uh, which can definitely move, you know, create the kind of friction that helps break up issues between the layers of those tissues and you’re getting the neurological input. So, it can work well in combinations with those other, you know, manual therapies and ultimately you need both. I mean, you need good structure, you need good function and, uh, I hope that adequately addresses the question but I think ultimately, we’re trying to work on both.
Dr. Justin Marchegiani: So, we’ll put some links below for people that want to get more information either about seeing Garrett or Garrett’s clinicians at his clinic or if you’re a practitioner and you want to get more information on, um, being able to use this device at your clinic or if you’re someone abroad that wants to work with Garrett’s stuff virtually, we’ll put some information down below. So, someone comes in, right, you give them a work up, you have a full physical exam, you’re looking at neurological signs, you’re testing muscles as well, to help find which muscles are off and on for compensation pattern stuff. You’re using the Neubie, you’re scanning looking for all these areas of dysfunction, you’re always evolving your method, right, the NeuFit method. What else has been plugged into the NeuFit method, the last year or two that you kind of added on recently?
Garrett Salpeter: So, the biggest thing that we’ve done in the last year is really explored the benefits of using very specific frequencies and this is one of the biggest champions of this type of work is a doctor named Carolyn McMakin, who has seminars on frequency specific microcurrent and the basic premise is that if you, uh, basic premise is resonance so for example, if I have the keys to my car and I go out in the parking lot, I hit the unlock button, this key only unlocks my car, it doesn’t unlock your car or my friend’s car or the other car across the parking lot. It only unlocks my car because that signal resonates with that car. It’s also the same thing if you ever heard of like the opera singer who hits that note, oh, you know, much better than I would dip, and that particular frequency of that note resonates with the lead atoms in glass and it breaks the glass. So, we can apply certain frequencies in the body that will resonate or preferentially go to and interact with certain tissues. So, if you’re trying to recover from an Achilles tendon injury, for example, we can, in addition to our usual treatments working on neuromuscular function, we can use a particular frequency that would direct that signal to the tendon tissue and help even further speed up the healing and amplify the healing effect of that, increase more blood and more resources specifically to that tissue.
Dr. Justin Marchegiani: Is this a new feature on the Neubie, where you can adjust the frequency?
Garrett Salpeter: So, it’s something that, um, we’ve had, we built it in to the Neubie, because I had kind of glimpses of this and we’ve only started to explore the, you know, the full benefits or more of the benefits of that in the last year and it’s part of, you know, clinicians who are in our, have completed our certification. It’s actually, that’s part of the level two stratification that we put out, um, in the, sometime in the last year and that’s been really exciting to see some of the, some the, you know, outcomes that people have been able to create with that and, you know, that can go down, that goes down a whole road of, you know, like Dr. McMakin, for example, has frequencies for different organs and things like that. We with the Neubie, our work and our scope is more around, you know, neuromuscular conditions and pain and things like that, so you know, we’re not necessarily able to, you know, speak about or make direct claims related to the health of certain organs or things like that, um, but, you know, there are some really cool things that people are able to do with this concept.
Dr. Justin Marchegiani: Very cool. There are two more things I want to hit on the book. You talked about heart rate variability which is essentially the unevenness between the heart beat and it’s a good window into recovery and the parasympathetic nervous system response. How are you gauging the amount of workload that the people you worked with can handle? Are you using HRV? How do you know, you’re doing too much? How do you know you’re on the sweet spot? How do you apply that with your patients?
Garrett Salpeter: That is, that’s a great question and this is I think part of the future of medicine and sports performance training is this notion of stress management and what heart rate variability, what it basically shows us is, it answers the question of how well are you, this individual standing in front of you, how well are you able to keep up with all the stressors in you life right now, you know, if you are, if you’re not, if you’re just like holding on to keep up with everything, you don’t have as much bandwidth to adapt to these subtle changes in air pressure as you don’t have these minor fluctuations in your heart rate, whereas if you are able to keep to keep up with that then you have more bandwidth to adapt to these subtle changes and so, heart rate variability is a great measurement. So, we look at a couple of different things that’s a big one, you know, if we look at someone’s HRV status when they come in for a session, and we see like dang they’re really in a stressed-out state. We may have a more recovery-oriented session with them that day. Over time, we also, you know, for people who have these wearable devices that tract their sleep, check their HRV, we have them do that, we just completed a study with Biostrap, who makes this one that I’m wearing in my wrist. It’s the best clinically validated of these, you know relatively inexpensive wearables, uh, they’re within one percent measurement of the gold standard, uh, of electrocardiograms like when you put electrodes all over the body and
Dr. Justin Marchegiani: that’s called Biostrap
Garrett Salpeter: Yeah, uh, so they have, you know, we worked with them and we saw that doing sessions on the Neubie, that people increased their heart rate variability, they decrease their resting heart rate without doing any cardiovascular training at all, um, also improved sleep and arterial elasticities, blood flow and blood vessel health and so, you know, all of that factors into, to saying looking at heart rate variability is something that we like, we don’t always look at it within a session, sometimes it’s you know, there’s a little bit of a delay in feedback. It’s well, you do something that day, see how their numbers were that night and the next day and then dial it back in the next time they come in. So, sometimes you get real-time feedback, sometimes it’s, you know, a day or two and you have to, you have to kind of start slow, see how much they can handle walk up to that line and you also have to factor in the stresses, you know in there because someone one day, if they’ve slept well and eat well might be and it’s, you know, weekend or something, might be able to handle a lot more than if they come in, in the middle of a week when they have a deadline, if they just have, uh, a fight with their spouse or fight with their boss at work or something like that and they didn’t slept well the night before and they’re sick and they’re going to be able to handle way different amount of stress and input in those days too.
Dr. Justin Marchegiani: Yeah. Which is totally different training philosophy, you know, 10, 20, 30 years ago was kind of like no pain no gain, you have to build a character, this is to toughen you up and it’s like well, really the goal of training is to add a stress into the neuromuscular system so your body can adapt from it and get stronger not so it can get weaker because if you can adapt to that stress, you just breaking your body down versus building it up and training and so it’s really kind of being training smarter versus harder kind of mindset.
Garrett Salpeter: Amen. Yeah. You know, I just think about it as, if I’m gonna invest the time and effort and possibly money to go to a physical therapy session or to a training session, you know, I just wanna have a return, I wanna have some benefit to show for that. So, it’s about, you know, ultimately about finding, you know, it’s not minimal or maximal, it’s optimal, it’s that kind of bell curve, it’s finding the right amount of input to get the correct output.
Dr. Justin Marchegiani: Love it. Very cool. You also started working with Terry Wallis, who is a popular figure in the functional medicine community, especially, on the autoimmune side. Dr. Wallis’ kind of story is for the listeners, she had multiple sclerosis was that one point even in wheelchair bound and couldn’t, you know, couldn’t walk and then was able to make different changes in her diet to help reverse her MS and MS is an autoimmune condition that affects the myelin which is the coating around the nerve so she was able to change her nervous system or her change her immune system, uh, attacking on her nerves so then she could actually start to heal and recover and now she’s fully walking. So, you’re using the Neubie device as a means to help stimulate growth, healing. Can you talk more about that application is?
Garrett Salpeter: Yeah. So, Dr. Wallis, I’m glad you mentioned some of her story, because it’s super inspiring and she’s now been able to help through her Wallis protocol and her book and her research, been able to help hundreds of thousands of people, stop the progression of or even reverse their MS and it has to do with a functional medicine approach reducing the inciting or damaging influences that are causing the immune system to haywire and create this autoimmune environment. All this stuff that, you know, you know more about than I do and that you talk about your podcast and the reason we worked with her is that she had this limitation in her program where she could get, she could help people stop the progression of their MS and then they get to the point where they say, okay that’s awesome. Now, what can I do to restore the function that I lost, now what can I do, if I wanna be able to drive my car again or you know, not to have caregiver at home or I wanna regain autonomy, I want to be able to walk or play the piano again, like okay, like that’s awesome. We stopped further damage but now, how can we do that and that’s where we got connected by a mutual friend and she saw, you know, I was describing NeuFit to her and some of the work we’ve done with some other neurological patients and she saw, hey, this kind of fills in, you know, this next step in our program, and since then she’s you know, invited me to speak at several of her, uh, seminars and live and virtual events and she very graciously gave an endorsement for my book and we’ve been able to work with her to share this message and kind of plug in NeuFit as part of her program and so through her, we’ve been able to introduce this to hundreds of thousands of people and many thousands of people have, you know, some have worked with us or gotten their own machine and worked remotely and many more have found NeuFit practitioners, we have on our website, we have a directory that we can link to, a directory of certified practitioners around the world who offer NeuFit and so many of these patients have gone and found people in their community, you know, sometimes they can find someone across town or, uh, nearby that they can go see and do this work, and we’ve seen people, you know, sometimes restore a little bit of sensation and function. Sometimes get out of a wheelchair and walk again and we’ve seen some of these transformational, really inspiring and amazing stories.
Dr. Justin Marchegiani: So, when you work with patients like that, are you doing a scanning method throughout that muscle belly area or are you just generally hitting the major muscles that aren’t working appropriately?
Garrett Salpeter: So, we typically will do a scan so that we can direct that stimulation, you know, in basically the areas where we’re going to get the most bang for the buck and we typically would do a scan, sometimes you can guess where you’re gonna put the pads and you can guess correctly based on knowing where their impairments are but sometimes there’s some nuances or different segments or different areas that pop up so we do like to do a scan , you know, at least in he first session as part of an assessment and then there we get the information to build a custom program and figure out, okay, where we need to stimulate to help get sensation or function back in the hands and feet or start to build enough strength so they can work towards standing and then walking or start to rebuild, uh, dexterity to be able to do the activity is that they wanna do.
Dr. Justin Marchegiani: Very cool. And then last question I have for you out of the gates here would be, nutrition is obviously important, right? It’s the building blocks of all of out nerves, our muscles, right? Quality is important, we don’t wanna add more toxins via, you know, plastics and hormones and pesticides, those kinds of things. What are some of the foundational diet changes, that you work on with your patients to really accelerate improvement? Is it the quality of the protein? Is it a certain amount, is it fats? What are the best bangs for your buck with nutrition to get better, your healing?
Garrett Salpeter: So, we’re looking at everything through a neurological lens and when we do that, we end up drawing many similar conclusions as you do through a functional medicine lens so there’s a ton of overlap. Maybe the way we speak about it or maybe the, you know, something some of the things we prioritize or emphasize are a little bit different but for us, one of the biggest in, especially in these autoimmune conditions right when you talk about the immune system and inflammation gone haywire but also just for brain and nervous system health overall. Inflammation is such a key, because if you eat an inflammatory meal, you’ll see IQ drop 10 or 20 points because the inflammation impairs brain function so significantly, and impairs peripheral nervous system function. [inaudible]
Dr. Justin Marchegiani: Blood flow too.
Garrett Salpeter: Yeah, absolutely. So, for us reducing inflammation is one of the highest priorities be whether you’re adding in overall health or you’re looking specifically through that lens of trying to optimize neurological function. So, that becomes a big deal, reducing inflammation. So, we’re looking at you know reduce, cutting out as many Omega-6 seed oils as possible but getting more saturated fats from good heathier sources. I mean, we’ve talking about, you know, grass-fed beefs or pasture-raised other animals or wild-caught fish, different things like that, you know the sources of fat become really important in reducing the Omega-6, having good monounsaturated fats like avocado and olive oil, you know, assuming someone is screened for food sensitivities and none of these things are gonna be like an individual’s person’s kryptonite or something like eggs can be great for some people, have a good health profile, if they have those nice, good dark orange yolks, um, but for some people have sensitivities and shouldn’t have them.
Dr. Justin Marchegiani: So, essentially, you’re really pulling out the inflammatory stuff, the refined sugar, the grains, those kin of things, maximizing good fats, maximizing good proteins, obviously having enough building blocks so the tissue we’re breaking down. There’s enough reserve to build that tissue back up as well.
Garrett Salpeter: That’s right. Yeah. So, you know, all those sources of fat I mentioned, the meats and eggs, you know also happen to have good, very good sources of protein associated with them, I also like collagen protein, if we’re trying to help someone rebuild tissues, um, and then also when we talked about inflammation and health of the nervous system, the gut is so important. So, you know, I’m a big fan of, uh, you know, different fiber powders that I put in my drinks every morning, um, and then, uh, you know the nervous system also is a big, big, big input. So, trying to do what we can to get that parasympathetic activation, you know, as many times as we can throughout the day to help with digestion is also a huge deal.
Dr. Justin Marchegiani: Are you still doing the ample drink every day?
Garrett Salpeter: I haven’t done those in a while. I like those, uh, I haven’t done them. Let’s see, nut there was a reason I stopped. Oh yeah, I think I didn’t, I didn’t, I really like the concept, I just didn’t love as much of the like whey and egg white proteins. I’m more of a collagen and you know meat guy.
Dr. Justin Marchegiani: Yeah. I’m a big collagen guy too. You just don’t get enough connective tissue, amino acids, the hydroxyl proline, proline, glycine, interesting. I have the same situation. What’s one clinical pro you’ve come across recently that you think most of the audience will be able to benefit from like, just anything in the last couple of months that’s like a real heavy hitter that would help a lot of people?
Garrett Salpeter: That’s a good, that’s a good question. Um, I mean in our realm, when we’re doing a lot more of this, you know, pain, movement, dysfunction, injury, helping people, uh, you know, the frequencies that I already mentioned, the biggest thing that jumps to my mind the last few months is some of this, some of this work that we’ve done on frequencies and, um, being able to find these resonant frequencies that it’s really cool when you feel this kind of resonating effect, it feel like this, you almost get these charges building up so it’s something that admittedly someone would have to you know, find a provider who has our device in order to experience it but for our practitioners being able to identify this and initially this frequencies were only used really in the micro current realm but use them with stronger power delivery with stronger current levels and deliver that power, that’s been one of the biggest things that really jumps out and, um, I just I have seen, already seen some really cool things happen there so that’s one of the biggest, uh, more for practitioners who do have access to this device admittedly but, uh, it’s really, it’s a really cool effect when you see, when you feel that resonance happened.
Dr. Justin Marchegiani: Very cool. Awesome. Well, thanks for all the excellent information, Garrett. Again, the NeuFit method, all kinds of good info and more we talked about the couple of things in the book here as well, um, take a look at it. If you have chronic pain issues, and you’re not healing or you have lingering injuries that aren’t getting over the top, we’ll put a link down below, where you can reach out to Garrett and his staff and we’ll put a link to the book as well. Appreciate it. Anywhere else Garrett, the listeners can go and check your information on it?
Garrett Salpeter: So, we’re most active social media wise on Instagram and the handle is NeuFit RFP and its N-e-u like neurological F-i-t and then RFP for rehab fitness performance. So, I’m on there, our team’s on there, we respond to DMs and comments and everything about, uh, we’d love to interact with you there, and hopefully if you’re, you know, if you’re interested with the book, hopefully, you’ll, uh, read it, if you check it out on amazon, please do leave an honest review on there. That feedback is wonderful. It helps us know what people like, what people don’t like. What content we can provide more of and I can assure you that having put in the hours on the book, I really appreciate that feedback very well much.
Dr. Justin Marchegiani: Very cool. If you guys are listening and driving, we’ll put links down below where you guys can reach out and support the book. Okay, Garrett, awesome chatting with you. Have a great day man. Good chat. Take Care.
Garrett Salpeter: Thank you, Justin. It’s been a pleasure.
Dr. Justin Marchegiani: Same here. Bye now.