
How do your emotions get affected by your gut state? In this video, Dr. J and Evan talk about anxiety and stress as an example and how we can manage them based on evidence-based practice. Excessive worry and stress can worsen GI problems, and studies show that treatments and good food templates will help people cope with their GI symptoms.
Dr. J and Evan clarify that the brain immediately affects the gut. For example, the thought of eating can stimulate the release of the stomach's juices before food gets there and vice versa. A sick intestine can alert the brain, just as a troubled brain can alert the stomach and intestines. Therefore, a person's intestine and stomach distress may cause or be the product of stress, anxiety, or depression. It's because the gastrointestinal (GI) system and the brain are intimately connected.

Dr. Justin Marchegiani
In this episode, we cover:
0:00 – Introduction
2:21 – The Importance of Gut Microbiome
4:21 – The Gut Microbiota's Effect on Mental Health
8:43 – Strategies on how to Approach Adverse Reactions to Probiotics
15:13 – Potential Neural Marker in Anxiety Disorders
Dr. Justin Marchegiani: For the podcast, really excited. Evan and I are gonna be chatting about the gut-anxiety connection. A lot of people have mood issues, uh, mental, emotional issues and they’re connected to the gut. And most people unless you have bloating gas, diarrhea, constipation, acid reflux, they’re not really connecting any gut issues to their mood especially anxiety. So, we’re gonna try to connect the dots for everyone here today. Evan, how are we going today man?
Evan Brand: I’m doing really well, you know, I’ll start out by saying if you were to go to a conventional doctor and the referral for anxiety or depression to a psychiatrist, they’re never gonna consider the gut. They’re never gonna run a stool test or an organic acids test or a mold toxin test. There’s a study done on mice and mice that were exposed to various mold toxins. They have lower levels of dopamine and we know people with lower dopamine, they could be more apathetic, they could be more depressed, they could just be less excited for the world and although the organic acids doesn’t measure GABA, we can tell just based on symptoms, like easily stressed, hard to relax, you need alcohol to calm yourself down or maybe you need chocolate to self-medicate. We know these people probably have low GABA and GABA is the breaks of the brain. At least, that’s how I refer to it. Think of the GABA as being able to inhibit or slow down the sympathetic overdrive and GABA is going to calm that and increase that parasympathetic reaction. Now, the connection is to gut, well, we know, there’s a paper here we pull up just because we like to have a couple studies, there’s one titled, “Gut Microbiota’s Effect on Mental Health: The Gut-Brain Axis”. Long story short, the study backs up, what we’ve already known and you and I have been doing clinically for a long time, which is that we’re fixing dysbiosis because we’re finding that when you increase levels of lactobacillus, this is key in producing GABA and so that’s pretty interesting and the study goes on to talk about the different inflammatory pathways and how dysbiosis creating inflammatory proteins in the gut. That’s gonna also affect anxiety. So, dysbiosis alone that’s sounds crazy to some, maybe to mental health physicians but if you have gut overgrowth problems, that could be the biggest single smoking gun for you mood issues.
Dr. Justin Marchegiani: 100% because the gut microbiome very important. It helps modulate the immune system. So god healthy levels of beneficial bacteria, Bifidolactobacterium, Lactobacillus beneficial flora. They’re gonna actually, help modulate the immune system, they’re gonna help with permeability, keeping gut permeability down. They’re gonna help with inflammation reduction. They’re gonna keep the inflammation down. They also help, um, take mold toxins that you may get exposed to and make them less virulent, less strong, less inflammatory as well and then also beneficial bacteria are gonna synthesize nutrients based on the food coming in, so it’s gonna take your poop and it’s gonna take poop and convert it to nutrition versus dysbiotic bacteria is gonna take you poop and make things take your nutrients and make you more toxic, right? So, we wanna really get high levels of nutrition and you’re gonna get endogenous production through health gut bacteria, like vitamin K, different B vitamins, you’re gonna get some fermentation acids that actually make it harder for a lot of bad stuff to grow. So, this is kind of important starting place and if you look at some of the medications that are coming out for more mood stuff, some of the mechanisms seem to be more of an anti-inflammatory on the brain. That’s very interesting because we know, the mechanisms in the past have been kind of SSRI or tricyclics in the 80s and 90s or SNRI, right. These different kinds of medications of course, you have benzodiazepines that work on GABA and the different GABA agonist, right. So, now, we’re working on inflammation and we gotta be careful because we had some inflammatories natural, not natural but anti-inflammatories in the early 2000s, they called, that was called Vioxx that killed 60,000 people. So, we gotta be careful because when you, uh, use a lot of pharmaceuticals anti-inflammatories there could be side effects and I imagine if it’s on mood and the brain, you could see strokes and things like that. So, we gotta be careful. So, we try to use as many natural components foundationally with diet and supplements. First, because of the least likelihood to cause problems.
Evan Brand: Wow. That’s insane. Well, you and I talked about the impact of exercise on anxiety before, we’ve covered that. We know that exercise is a super potent antidepressant. Here’s something cool about the gut in this particular paper. I put it in the chat for you if you wanted it, but it talks about how Lactobacillus strains upregulated BDNF, which is the brain derived neurotrophic factor and that resulted in increased regulation of the HPA axis. Let me just read the last part again because that’s pretty nuts. Supplemental Lactobacillus increase the regulation of the HPA axis, so here we are working with people using adaptogenic herbs but let it, but the cool thing is we’re actually fixing the adrenals by fixing the gut too, which is amazing and then it goes on further to talk about supplementing with Bifidobacteria and how the patients in the study rated an overall happier mood using six dimension of mood including: energetic, uh, composed versus anxious, elated versus depressed, clearheaded versus muddled, confident versus unsure, and agreeable versus angry. So, long story short, this actually improved the HPA axis functionality, as well as diazepam, or there’s another one here citalopram, that’s an anti-depressant, that’s an SSRI so long story short, this is pretty nuts. Probiotic therapy reduces the depressive symptoms and improve the HPA axis as well as an SSRI. So, there you freaking go. And here’s one more thing, Bifido infantis increases tryptophan, a serotonin precursor. So, we always talk about, okay get tryptophan in the diet but simply the good bacteria can actually make tryptophan, which then makes serotonin and GABA. This stuff is just amazing.
Dr. Justin Marchegiani: I put the study up on screen. So, anyone watching this video here could take a look at it again. If you are listening to audio, we put the video link down below. If you guys want to look, this in the journal clinical practice 2017: Gut Microbiota’s Effect on Mental Health. And I’ll just gonna read that conclusion again. Dysbiosis and inflammation of the gut have been linked to causing several mental illnesses including anxiety and depression, which are prevalent in society today. Probiotics have the ability to restore normal microbial balance, therefore, have a potential role in the treatment and prevention of anxiety and depression. It gets really powerful there. And again, that’s only one of many things. Now, um, just to comment, I see a lot of people that get their mood worse when they have some of these things too. So, what’s the deal? Well, probiotics can be high in histamine and they be high in FODMAP. So, if you have a lot, if your immune system is so wound up, the histamine from these probiotics may cause problems, also the fermentable nature of these probiotics may cause problems, if you have SIBO. So, if you have massive bacterial overgrowth or your immune system is so wound up, when you can’t process histamine or you’re sensitive to histamine then you have to be careful with these things. So, even though we say, this is good, it doesn’t mean it’s good for everyone. So, we’re just trying to lay out, hey, it maybe good for you but if it’s not, here’s maybe the reason why and we just have to dig in deeper and so there’s really no just magic solution. There’s a lot of tools that we kind of line out and we go in sequential order and work them through with our patients to get the best results possible.
Evan Brand: I’m so glad, you went that direction with the conversation because me listening to myself as a third person, I’m thinking, oh my God, I need to go out and buy probiotics right now and I’m gonna just feel happier and less anxious and all that. And that certainly was not the case for me when I had gut infections and I tried probiotics, it made me worse, it made my skin worse, it made mood worse, I got more anxious, and what the hell is going on. Well, as you mentioned, there’s a sequential order so I love that and this is why it’s important for you to do, and for I to do what I do because you and I are seeing these things clinically and the trenches is totally different versus somebody with a health podcast. They could look at this study and they could do a whole podcast about this, and then they could trick people not on purpose but just not having the clinical background, they could look at this and go, oh my God, probiotics are gonna be the miracle cure and then people are gonna listen to the podcast, they’re gonna do it and then they’re not gonna have a good reaction like me and they’re not gonna know what to do. So, I’m so glad that you’re integrating the clinical approach to this thing which is wait a second, yes, this is all true but there’s an asterisk next to this study and the asterisk as you mentioned is what if there’s bacterial overgrowth and the histamine bucket’s already so full or what if a mold or a mast cell has problem and the histamine bucket is already so full, so you can’t tolerate these probiotics. So, maybe walk us through what you’re doing, what do you suggest people do if they’ve had a reaction like that to probiotics, maybe they didn’t do it at the right order, or how should they approach this?
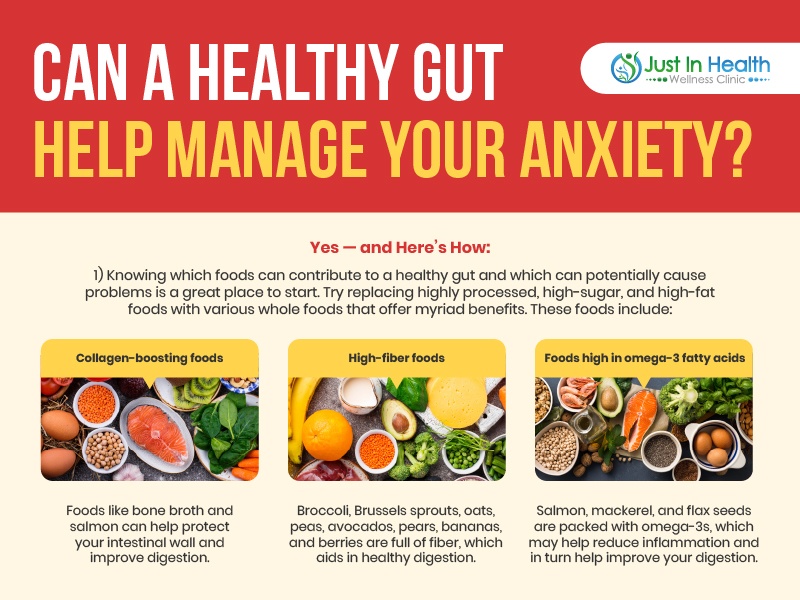
Dr. Justin Marchegiani: Well, the first thing we have to really do is just calm down the immune system and the biggest factors that we have to do that is the food that’s coming into our body. So really, choosing a good anti-inflammatory, nutrient-dense whole foods and, and if we know that there’s a lot of digestive issues, bloating gas, we may have to restrict FODMAPs and fermentables out of the gate to kind of decrease the dysbiosis. Because when we address like gut microbiome issues, we hit in three ways, right, we starve it, we kill it, we crowd it out. So, starve, kill, crowd, starve, kill, crowd. And so, the first aspect of that is shifting the foods to starve some of these microbiomes that maybe bad and then again it’s gonna be short-lived, we’re not gonna, we don’t wanna go low FODMAP forever, right, because there’s a lot of good foods that have FODMAPs in it and even histamine in it. So, there’s no reason, we’d want to do that but, in the beginning, if we can shift the immune system, calm it down, if we can shift some of the microbes down and then as we start adding different things in supporting our ability to break down food, start adding in adrenal support because when our nervous system is just stuck and our vagus nerve and our parasympathetics are low and our ‘fight or flight’ is high, our immune system is gonna be, it’s gonna be overly sensitive, okay. It’s gonna be overly sensitive and we’re also gonna have poor digestion and when we have more poor digestion, we’re gonna have gut permeabilty issues, we’re gonna break down our food and we’re gonna have more of these foods in our gut get into the bloodstream and stimulate the immune system in a negative way. And so, if can calm down that immune response through decreasing our sympathetic nervous system whether it’s breathing techniques just good diet and lifestyle, good food, managing blood sugar throughout the day, not over under exercising, good hydration. All of those things are kind of, you know, the foundational marks, that we put as we work up a patient. So, we have that foundation there.
Evan Brand: Here’s the question that came in from Keith, he said, “what are your thoughts in taking colostrum for gut health? We use colostrum but as you mentioned in that in immune situation, we might not want to use colostrum. I’ve had some people, where their immune system is so just haywire that colostrum does affect them. It’s not super common but there are some cases where we can’t use it and so in that case, we may be coming in with more herbal based leaky gut supports DGL, glutamine, zinc, carnosine, more amino acids
Dr. Justin Marchegiani: amino acids, nutrients. Yeah, I mean colostrum, because it comes from a cow, right? It’s gonna be, more dairy based. Supposedly, colostrum is dairy free meaning, you’re not gonna get the casein and the lactose. So, it depends on how sensitive, you are. Some people, they may be sensitive were they still in a problem. Some may, it may be okey. I tend to just avoid colostrum, just because my patients are very hypoallergenic and so I tend to use more of the more hypoallergenic compounds like the zinc and the glutamine and the DGL and just things like that. Not saying, it’s not beneficial and I’ve had my patients take it and do well with it. So, I’m on the fence with it for sure, I have a little bit of colostrum in my true keto collagen and patients do really well with that. And so, it’s a tool that we put in our tool belt, but for our sensitive patients, I tend to not be the first thing that I jump on for sure. I think we’re on the same page with that.
Evan Brand: Yeah. Uh, here’s a person here, “what about a probiotic that has both Lactobacillus and Bifido, will they cancel each other out?” No, we used those together all the time and some of the most high-quality professional formulas we make. We have combinations because you get different nutritional benefits in the gut from different species. There are some cases, where I have done straight Lacto or I’ve done straight Bifido, just to see how people do? But those are like the one percent sensitive people. The average person, we’re working on, they can tolerate a combination and then obviously, if we’re working on mold or Candida or some other problem, we’re often throwing in Saccharomyces boulardii in there too. So, then now you’re doing Bifido, Lacto and you’re doing Saccharomyces. That triple combo which technically Saccharomyces boulardii, even though it’s marketed and sold as a probiotic technically a yeast will often work that into the protocol and it does so much better.
Dr. Justin Marchegiani: Yeah, 100%. Evan, what’s your experience using spore-based probiotics?
Evan Brand: You know, they give me just terrible gas. My God. It just hurts my tummy; I’ve tried them and I went on them and I went off of them. I went low dose. I went high dose. I mean, we even manufactured some too and I’m like, God, I just don’t feel that good with them, I’ve had some people that are like, hey, this thing is a miracle cure, this is the best I’ve ever felt and good for them. But for me, it just did not go well, so I feel much much better with a low histamine, more I guess, you would just call it living probiotics as opposed to the spores. What about you?
Dr. Justin Marchegiani: Yeah. I mean, It just depends, I think patients that don’t do well with your Lactobacillus, Bifidobacter, I definitely have a good bunch that do better with the spore based probiotics. So, depending on the level of SIBO that’s going on, some patients do really great with it. I have no problem myself with higher dose Bifidobacter, Lactobacillus infantis species, so I don’t have with it. But some patients, I know with significant SIBO history just do well on, if they just do much better and supposedly that the spore-based probiotics really help potentiate the growth of these other beneficial flora. So, it does help a lot of the other beneficial flora and they do hang out a lot longer too.
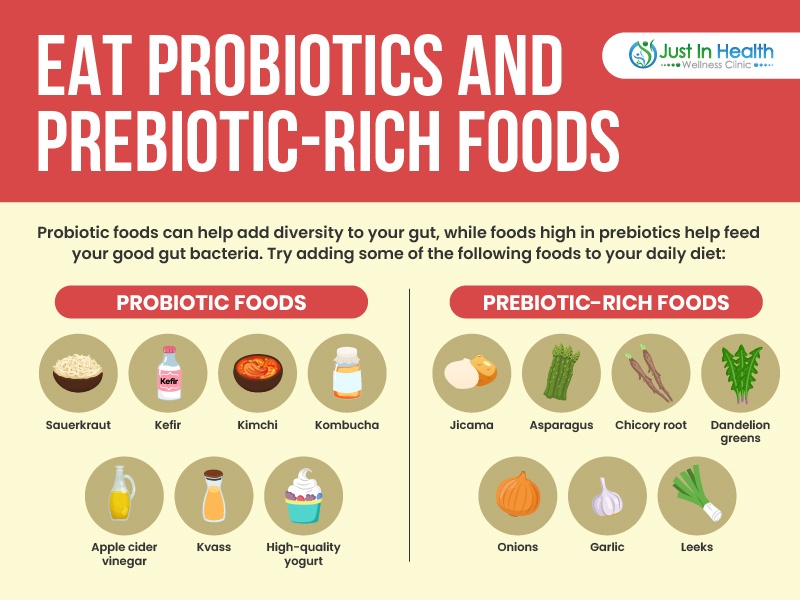
Evan Brand: Yeah. And I’ve tried a couple of different professional brands. I mean there’s two big brands out there. I tried both. The one I did actually feel pretty good on, a couple others I didn’t feel so good on. So, I think it could be a brand difference too. There was another question here, “when is the best time to take probiotics with fiber or empty GI?” I don’t know the whole wheat fiber deal. I’ve never heard of that before. I personally take them on an empty stomach and I’ll do them first thing in the morning like before breakfast. I’ll just pop all my supplements or I’ll take them before bed. Unless, I’m taking a binder then I won’t. My thought on it is to try the bacteria in there especially because some of the professional manufacturers, you and I use, we’re using an acid resistant capsule. So, it’s gonna actually bypass the stomach acid and deliver the beneficial microbes to the gut so in that case, that’s why I like it to be there. Just because, there’s not as much competition with the food could just be theory, I don’t have any proof that it works better but that’s how I approach it.
Dr. Justin Marchegiani: Yeah, that makes sense. I mean you can definitely have some beneficial effects with some fiber, with some probiotics because the fiber does act as prebiotics and it can help kind of provide the fertilizer for the seed, the seed being the probiotics to grow. I do like it. A lot of your conventional probiotics tend to do better on an empty stomach but I mean taking them with food has some beneficial effects as well with digestion and such and so I say. Try to take most of those with food. I think that’s good. I just wanted to pull one study up here, I think this is interesting, um. Let me pull this up here. So, just kind of support we’re talking about right. This study is looking at neuroinflammation association alterations of the brain is a potential neural marker in anxiety disorders, so we’re just trying to build up the case that we’re talking about here. Preliminary evidence suggests anxiety disorders are also associated with increased inflammation. Systemic inflammation can access the brain and enhance pro-inflammatory cytokine levels that have been shown to precipitate direct and indirect neurotoxic effects. Prefrontal and limbic structures, these are parts of the brain that have to do with higher thinking, uh, emotions, memory are widely reported be influenced by neuroinflammatory conditions in concord with these findings various imaging studies on panic disorders, agoraphobia, generalized anxiety have been reported alterations in the structure and the function and the connectivity of our prefrontal and limbic structures so what they’re saying is inflammations affecting the parts of you brain that are involved. They’re higher thinking, higher function memory cognition anticipating, you know, cause and effect based on your actions, right. Prefrontal cortex is it’s the part of the brain that allows you to anticipate, to think, to plan, um, most of people from our you know from evolution we’ve been more, um, midbrain kind of reptilian brain type of you know, kind of knee jerk reaction kind of response and the frontal cortex gives us the ability to think and certain nutrients have allowed that part of the brain to grow. High quality cholesterol, Omega-3, free fatty acids, amino acids help that brain to grow. But if we’re driving inflammation in that’s gonna have a negative impact. Now what are the things that are gonna be driving inflammation in our diet? Well, Omega-6, refined processed vegetable oils, trans fats, refined sugar, too much carbohydrates, too much sugar, these are all gonna drive brain inflammation. And of course, inflammation in the gut can cause inflammation in the brain. Inflammation in the gut is bidirectional, it is a two-way highway. Inflammation in the body whether it’s like getting exposed to round up or mold toxins can cause gut inflammation. Inflammation in the gut through dysbiosis and food allergens can also cause leaky gut and cause inflammation from the gut to go outward up to the brain and it can activate the microglial cells in the brain which can create fogginess and more immune response that can make us feel worse and more, um, more anxious or depressed based on what’s happening in the gut.
Evan Brand: I just sent you one, other paper too, which kind of interesting, talking about antibiotics and how antibiotics are gonna drive up depression and anxiety and talked about treatment with just a single course of antibiotics was associated with a high risk for depression and then also anxiety. So, I’m not saying don’t take them, I mean if you need them to save your life. But I will just say, that’s there’s so many people that have been put on these different medications that affect the gut and so when we’re trying to paint the picture here of what went wrong, why did someone become anxious, it could have been that they went in for a routine dental procedure and they were taking the antibiotics, they screwed up their gut, now they have dysbiosis as you mentioned, this big inflammatory link to the brain. Now, they’ve got this bacterial overgrowth, they simply were using something as preventative medicine, these antibiotics and then boom, now they’ve got this overgrowth. And then as you mentioned these bacteria are pooping poop and then that’s going to make you more anxious, so there was a question that came in about, well, “how much time do probiotics take to work for anxiety?” I mean, that’s a really tough question to answer because what else is going on, are there gut inflammation issues, are there bacterial overgrowth issues. What about Candida problems, I mean, there’s other things we have to factor in, so I wish it were just so easy to say hey take this probiotic in three weeks, you’re gonna be less anxious. I wish that were the case but, I think the answer is it depends.
Dr. Justin Marchegiani: Totally. One study here, I’m putting the study up on screen, so you guys can see, Anxiety exposure and the risk for depression, anxiety or psychosis, journal of psychiatry 2015. So, you guys can see the abstract and the conclusion down below. Take a look at this study, all right. All right, where is it. Systematic Administration of Curcumin Affect Anxiety-Related Behavior in a rat model. So, it’s interesting. So, what we’re trying to look at here is results suggest that curcumin has anxiety-lytic like effect on biochemicals and behavior. Uh, it may be useful agent to alleviate or treat psychiatric disorders similar to those observed in patients with PTSD. So, what are they saying here? They’re saying in this rat study, giving curcumin actually resolved and significantly had a benefit on anxiety. Now, why is this? Well, because it has natural anti-inflammatory benefits and the postulate is that by reducing inflammation in the brain and in the body that also helps the mood and anxiety. Now, we don’t wanna just rely on the supplement. So, people that are watching this right now, don’t just say hey, I’m saying to fix your anxiety get curcumin. Fix all the foundational things that set the table, that drive inflammation and then once you have the foundation then you can go dig deeper and using specific supplements to reduce inflammation like curcumin, like Boswellia, or frankincense. You can also, there’s systemic enzymes that can be taken away from food. There’s a lot of good higher dose fish oil, ginkgo. These are excellent nutrients that can help drive down inflammation. A lot of the bioflavonoids and some of our lower sugar fruit like berries and quercetin, those kinds of things. And other studies on a handful of blueberries a day can reduce inflammation in the brain to. And we talked about that in the past, so inflammation plays a major role and get the foundation right. Because if you have a lot of dysbiosis but you’re trying to take curcumin to cover up the inflammation, fix the gut stuff first, fix the adrenals and the sympathetic overload first, fix the food and the blood sugar and then you can dive in deeper with extra functional medicine nutritional, uh, tools.
Evan Brand: Yeah. Yeah. Good point. And I’ll just say it in another way, which is that you could take all the generic stuff meaning generic natural stuff as you mentioned Boswellia, curcumin, potentially high dose fish oil to reduce inflammation. Maybe you’re gonna lower the anxiety some but you’re still not getting to big root of it which for me was gut infections. I had parasites, I had H. pylori, I had major bacterial overgrowth, I had Candida problems, I had mold problems. All those things were affecting my gut which were affecting my brain so I was having just out of the blue, anxiety, I mean some points, I was panicking, I thought I was dying in some situations. My blood pressure was going crazy for a while, I mean it was all related to these toxin issues and so I encourage people to get some of the labs run so you can figure out what the heck’s going on. The first place to start obviously is gonna be a stool test. So, we run a DNA stool test that you can do at home and you get that back to the lab and then you can get a really work up on what type of infections do you have. Is it just bacteria or do you have parasite? What about your gut inflammation? Have you measured that? Because if you’re anxious and we see high gut inflammation, we gonna go ding ding ding look at the connection there. And then, we mentioned on the Oak test, there’s not GABA but we can do trial runs. I manufacture a chewable version of GABA that we use, it’s pharmaGABA, which is fermented and bioavailable. So, we use that. And if people have a good response to that, then we assumed that they had a low GABA situation. If they take one or two of those and then they feel better then hey we’re pretty happy.
Dr. Justin Marchegiani: Also, let me just. That’s very good and so, if you wanna support the show, some of the supplements that we’re gonna recommend we’ll put it down below in the notes section you know recommended supplements. So, Evan has a chewable GABA. I also have a liposomal curcumin. When you’re taking curcumin, you wanna make sure it’s liposomal. So, it has maximal absorption, only about 15% get absorbed,uh, it’s also better absorbed with black pepper as well, but people that have night shade sensitivity that may be problematic. So, if you want curcumin supreme is a liposomal version, we’ll put down below. Put Evan’s recommended products too. Now, interesting study here, when I look at inflammation in the same rat study. When they looked at the administration of curcumin, they actually saw a decrease in cortisol. So, this is serum cortisol here and as they increase the curcumin, you can see the drop in cortisol. And it makes sense because cortisol is an anti-inflammatory, so, the more your inflammation your body has, the more you’re gonna surge cortisol to help reduce the inflammation. The problem is cortisol is catabolic. It’ll break down tissue and so in the long run, you don’t want cortisol out of the balance because it will start breaking up tissue. So, in interesting enough to see that the reduction in cortisol followed by the increase in the amount of curcumin given to the rats. And the increase in, um, improved mode, the decrease in anxiety. So, that’s powerful. So, we wanna look at everything from a root cause. We wanna have all of our foundational tools and our palliative functional medicine, nutritional tools to plug in. And its good data to back it up, so we, you know, we can see, yeah, these things make sense because I always tell patients I’m talking to, what’s the mechanism, what’s the root cause, are we getting to the root cause and are there anything else we can do palliatively to support the healing of the root cause.

Evan Brand: Yeah. Meaning, okay we could do some chewable GABA, we could do some curcumin, or whatever else to try to calm things down, while behind the scenes, we’re working on getting the mold out, fixing the bacterial balance, integrating probiotics, restoring gut flora, bringing in Saccharomyces boulardii to address Candida. All thes things are, I mean, that’s the art of it, right? That’s the fun and the beauty of what we do and it’s just a blast. Let’s hit this question here from Sarah before we wrap it up. She said, “Are there any thoughts on raw milk to help heal the gut if tolerated, ok? There are mixed thoughts with this.” I’ll rant on it really quick. My thought is because I had a lot of issues with dairy, I personally just do butter and I feel best with that. And I would argue that to help heal the gut, we can use all these clinically shown ingredients that don’t use dairy proteins like the zinc, carnosine, the glutamine, the chamomile, the DGL. So, my bias is to go for that. But, what do you think?
Dr. Justin Marchegiani: I have the same as well, um. I don’t do great with raw milk. I get massive diarrhea, massive bloating issues even raw. Now, the benefit of raw milk is, you have all the cream right the homogenization tends to like kind of damage a lot of the globules and then of course pasteurization destroys all the enzymes that help you handle casein and lactose, which is the sugar in the milk better, the caseins, the protein. And so, there’s that right? And so, you tend to had. If you have problems with dairy, you have a better chance of being able to tolerate it with raw milk. Now, even with raw milk, I don’t do it as well, but I do, I don’t tolerate as well but I do tolerate butter and ghee wonderfully because it’s cut out the casein, it’s cut out also the lactose as well. So in general, if you’re more hypoallergenic probably stay away from it, wait till you’re healthy or try it, um, if you’re relatively healthy and you wanna give it a try, sure, but in general, if you’re having immune issues or chronic inflammation issues, probably stay away from it until you get things under the control and then you have a better baseline and then when you try to add it in, then you’ll really be able to know, if you can handle or not because you’ll, you’ll go from feeling good to not and It’ll be quite clear.
Evan Brand: Yeah. Question from Ty, “what’s the first diagnostic tool we can use to determine the state of your microbiome?” uh, typically two things were gonna do, the stool test, the DNA stool test we use at home and something that Justin and I run clinically on pretty much everyone and then the organic acids test is helpful too because we’ll certain bacteria pop up that maybe the stool test missed or vice versa. So, stool and urine at home, those are thing that we can run and they’re incredible valuable tools, so valuable that I almost don’t even want to work with somebody without those data points because at that point you’re just guessing and we prefer to test not guess.
Dr. Justin Marchegiani: Totally, now on those tests, we may look at commensal bacteria like Bacteroides and Firmicutes, uh, Bacteroides and Firmicutes, you want essentially, you know good levels of Bacteroides or Firmicutes. If people have high levels of Firmicutes in relation to Bacteroides that could be a problem but that usually is never the problem in and of itself. Usually, there’s dysbiotic bacteria, Citrobacter, Klebsiella, Pseudomonas, um, Morganella, right? These are all dysbiotic type of flora that are overgrown, that can throw off a lot of the commensal stuff. So, ideally if we see commensal bacteria off. We want to address the dysbiosis first and then we can use different fibers and prebiotics and probiotics down the road. Once we’ve kind of fixed a lot of the dysbiosis and that kind of help get it back in the balance.
Evan Brand: Man, I tell you half an hour flies but we gotta run and this is something we could do a part two part three on but the big smoking gun for people with anxiety might in my opinion based on suffering for years and years and years of with different issues, it’s the gut, the smoking gun for anxiety, mood issues, depression, fatigue. A lot of this is coming from the gut. You and I have hit upon how B vitamins are made in the gut too, you did a really eloquent explanation on previous podcast about how you’re making the nutrients that fuel the mitochondria, we went pretty deep into that before so that’s an exciting mechanism that I think most people are not talking about they’re putting people on Adderall or other things to try to boost up their mental energy. You gotta look at the gut so I encourage people to get tested. And if you need help, you can reach out clinically. We have a question from, uh, where’d it go, Pelona, “how can I contact you or have an appointment?” So, uh, Dr. Justin Dr. J, he’s available worldwide, so am I. If you want to reach out to him, it’s at justinhealth.com. You can reach out worldwide, phone, facetime, skype, whatever and then for me Evan, evanbrand.com. We’re available for consults and we can send labs to your door, we run those, we get them back to the lab, jump on a follow-up call, review the results and then make you a protocol, get you feeling better as quick as we can.
Dr. Justin Marchegiani: Excellent. I’ll put a list of recommended products and recommended, uh, resources for today’s podcast to kind of back up what we’re saying. Also, you can watch the video on screen where we pull up some of the studies and if you guys enjoyed it. Gives us a thumbs up. Put your comments down below. Let us know what you like and what you wanna see improvement on and recommended topics coming up all right. Evan, thanks for everything. evanbrand.com, justinhealth,com We are here to help you guys. Have an awesome day.
Evan Brand: Take care though.
Dr. Justin Marchegiani: Take care. Bye.
https://justinhealth.libsyn.com/the-gut-anxiety-connection-podcast-352
International DSL GI Map Genetic Stool Test