
In this podcast, Dr. J and Evan talk about the connection between the gut and respiratory system. You might not immediately associate gastrointestinal problems with lung disease, but the two frequently coexist. The tissue and glands in your lungs and intestines are the same and react to the same triggers.
At first look, the operations of your digestive and respiratory systems appear to be somewhat dissimilar. Though, the systems are connected in a variety of ways. The digestive tract can function because of the outcomes of respiratory action and vice versa. In addition, the systems collaborate to deliver energy to the body's cells.

Dr. Justin Marchegiani
In this episode, we cover:
3:08: Key factors of lung inflammation
7:48: Probiotics as regulator of immune response
11:56: Foods major role in gut-breathing connection
20:17: Available Testing and Herbs
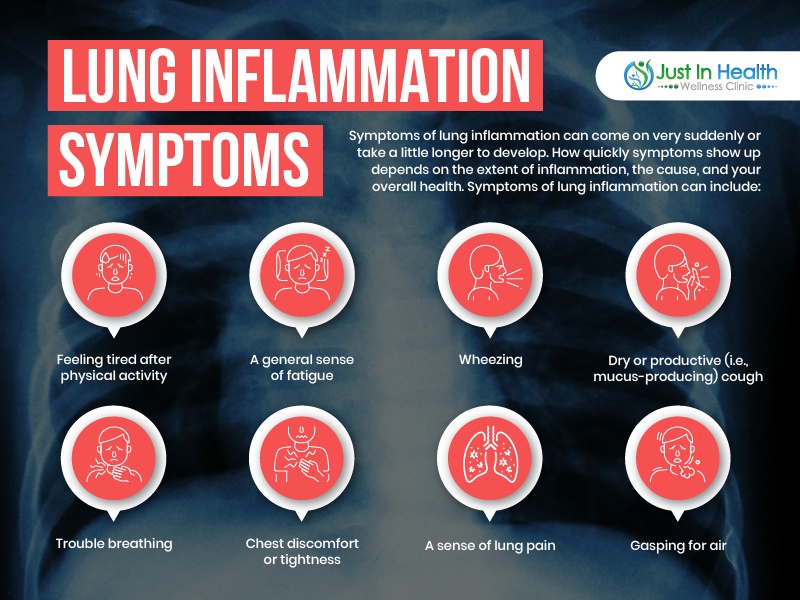
Dr. Justin Marchegiani: And we are live. It’s Dr. J here in the house with Evan Brand. Today, we’re gonna be talking about the gut, lung connection. This is really important. Lung health today, it is very important. We have to get good oxygenation. We have to make sure that inflammation from different microbes in the environment, whether it’s allergen or infections, we have to make sure that we’re able to still breath and transfer oxygen even with those stressors in the environment. We’re gonna talk about how the gut is connected to that, how inflammation in the gut can be bi-directional and can affect the lungs as well. So, let’s dive in. Evan, how are we doing today man?
Evan Brand: Hey. Doing really well. Starting this thing off, I was looking at some papers this morning. I told you this was just too important for us not to cover so in the journal of immunology from this year 2021, I’m just gonna read you one, really, really big thing here which is the fact that intestinal dysbiosis is associated with increased mortality in respiratory infections due to an exacerbated inflammation and decreased regulatory or anti-inflammatory mechanisms in the lungs and the gut and they say here, pointing to this important relationship. So, this was actually the first time I’ve heard. You and I have been talking about stuff for years, I mean, we’ve done between us both close to, you know, thousand podcasts and we’ve been talking about gut-brain axis, we’ve talked about the gut-thyroid axis, we’ve talked about the gut-skin axis but I don’t think we’ve ever hit on the gut-lung axis and so this paper is just really reviewing the literature on this and it’s absolutely incredible because guess what, the beneficial bacteria helps respiratory infections and there’s 30 pages, if not more, I haven’t even had a chance to review all the papers on this but there are countless, countless papers now and pages of papers showing that the probiotics actually can reduce the inflammation in the lungs, however, if you’re in the hospital or if you were in the unfortunate situation of being in a critical care unit, an ICU, you’re gonna be getting antibiotics more than likely and you’re not gonna be getting probiotics. And, we could go into the mechanisms but I think the mechanisms will probably bore people but long story short, there’s an increase natural killer cells and obviously decreases in inflammatory cytokines and there’s many, many other mechanisms but long story short, probiotics are absolutely amazing and we know that the antibiotics that you’re gonna get in these situations are gonna do the exact opposite.
Dr. Justin Marchegiani: Absolutely. Here’s a great study here. I know, we’re kind of referring to some of it. I’m going to share my screen here with the audience so everyone can see it, all right. Let me know if you guys can see this here. I’m gonna pull this up here so you guys can see it. All right. Can you see my screen there? All right. Awesome. All right. So, off the bat right, one of the key driving factors of lung inflammation is gonna be dysbiosis, right? Why is this? A lot of this has to do with the fact that bacteria, 80% of the immune system is in the intestinal tract, right? You have some in the GALT, which is gonna be the gastric associated lymphoid tissue, that’s in the stomach, right here. And then, you have the MALT, which is the mucosal associated lymphoid tissue. So, the mucosal, uh, that’d be the intestine. So, the small intestines in the middle here and then the peripheral on the outside is the large intestine. And so, a couple of the big things that you’re gonna see is when the immune system is overactive. One of the first things the immune system does is when it’s overactive, it actually creates inflammation, right? Part of inflammation is vasodilation so it can bring the immune system, the immune cells there to help fight it off. Think if you get bumped in the eye. What happens to the eye? It gets swollen, right? And so, you create this low-grade inflammation which is part of how the immune system works. The problem is, you know, most that inflammation that we’re seeing in people, it’s not an oops, I broke my elbow, it’s gone in a day or two, it’s a chronic low-grade inflammation and so you can see, um, when we add in things like probiotics over here, right, probiotics do a bunch of different things, they regulate the Th1, the Th2 immune cells, right? So, Th1, Th2, right, so that’s gonna be the natural killer cells on the Th1 side versus the antibodies on the other side and so, we have this balance between helper natural killer on the one and we have the antibodies on the two. So, we have this good balance and if they have it out of killer, like, let’s say we have higher Th2, you may see more allergies and things like that which can obviously stress out the lungs and obviously if we have some kind of infection in the lungs, we want good Th1 modulation because if the Th2 is really high, the Th1, those natural killer cells are gonna be lower. And so, you can see, obviously, it’s gonna express several viral defense genes. It inhibits various cytokines and chemokines so the chance of you having, um, what’s that, what’s the expression they call it here, it’s the inflammation after a virus kind of comes in and ravages the lungs
Evan Brand: Like the cytokine storm
Dr. Justin Marchegiani: Yeah. Cytokine storm and so this really helps modulate the imbalance in cytokines after the fact, right? And obviously, it’s gonna modulate immunoglobulins, that’s your antibodies, your IgG, IgA, IgM, IgG and then to modulate your innate and adaptive immune system and obviously it’s gonna help with the allergenic anti-allergenic property, so that’s gonna be a Th2 stimulator. So, you can see, it’s gonna really help modulate this here. And again, this article doesn’t even really address it but if we don’t have good gut absorption of let’s say of vitamin A or vitamin C or vitamin D, right, if we don’t have good absorption in the gut then obviously all those nutrients play a major role in modulating the immune system too. Any comments on that, Evan?
Evan Brand: Yeah. Well said. So, I’ll take it a step further. We see all sorts of dysbiosis, bacterial overgrowth, Candida, parasites, worms, gut inflammation coming from the diet. You alluded to the malabsorption. So, let’s say, you’re giving someone X amount of zinc, let’s say you’re giving someone X amount of quercetin and vitamin D and vitamin C and you’re thinking that you’ve got a good protocol, well, we talk about this all the time. It’s not really about what you eat or what you take, it’s about what do you actually digest, what do you absorb and what do you assimilate from that so the problem is I have first-hand experience now with some really, really intense medical cases, we’ll just leave it at that for now. And, this particular person has been getting vitamin C in a crushed-up tablet form where in reality, we should be getting IV vitamin C. So, it’s not just about what you get, it’s how you get it, it’s how much you get it, it’s how much what you get from what you’re taking. And, there’s a lot of issues and if you say you’re getting 2 grams orally in a crushed-up low-quality form, we know that Vitamin C. In general, we see it low all the time on organic acids testing. Maybe, you’re getting a tenth of that so you’re really just gonna get the therapeutic amount so a lot of people I find are either being fairy dusted or fairy dusting themselves because they’re putting so much hope into the products they’re taking and they’re just not getting much from that due to these underlying issues with the gut. And, you and I have beat the drum on the gut for freaking 10 plus years and we’re still having to beat the drum on the gut but I hope that you feel as good as I do about all the work we’ve done because we know that everything, we’re doing with the gut is improving people’s responses so that if they do get exposed to something, they gonna have a much, much healthier, better response to it.
Dr. Justin Marchegiani: 100%. I want to show one more article up here if you don’t mind. We’re trying to incorporate some of these new systems here so people can kind of see what’s happening with some of the articles that we’re looking at while we go live. I think it should be helpful. All right, there’s one thing I wanted to post here. So, we’re looking at different infectious stress on the lungs and what’s happening but look at what’s happening with probiotics, right? Probiotics are having an effect on modulating TNF alpha, Interleukin-6, it’s having also effects on modulating over here, your CD4 cells, these are your natural helper cells. Probiotics, actually, have a major role in modulating this whole immune response and so, you know, I think one of the best things you can do if you have poor gut health out of the gates here is potentially adding in some probiotics, uh, maybe adding in some fermented foods as long as you are getting bloated or gassy. Now, some people that have SIBO, these things may make it worse and so if you’re one of those people that probably won’t be the best thing but if you’re trying to be more in preventative mode, we probably want to get some of this dysbiosis under control and work on building up good bacteria after the fact, kind of my general analogy is you get your car washed before you get it waxed. You go and throw down seeds only after you’ve done the weeding in your lawn. Anything else you wanna add, Evan?
Evan Brand: Yeah. Except for like in acute situation, you might have to change the order of operations, you might have to go hardcore in it maybe some bloating, some burping, some gas, some kind of reaction, you know, you gotta make a pros and a cons list, right? There’s always a risk benefit analysis and those short-term effects from a probiotic if it were in the wrong order per se are not gonna be a huge deal, long-term.
Dr. Justin Marchegiani: Yeah. Absolutely. Let me just kind of, all right, good, so I think that’s really good. So, first thing I wanted to add on top of that is we know gut permeability is a major stress on the immune system because you’re allowing undigested food particulate potentially or potentially like endotoxins which are like the outer shell of the bad bacteria, potentially even mycotoxins from fungus or mold, right? These things affect gut permeability. When the gut is more permeable, that allows more foreign antigens, think of antigens as like foreign proteins, right, so you could put bacteria, viruses, food, all in that kind of anagen category. It exposes more things to the immune system and the more you expose bigger chunks of things to the immune system, the more responsive the immune system will be. And so, ideally, we don’t want to poke the bear, right? Think of it like, gut permeability is poking that sleeping bear and we don’t want to over stimulate that and create immune responses unless we really need to.
Evan Brand: Yeah. You know, what’s crazy too, this, I mean, we’ve seen so many things with obesity and you know worse outcomes and diseases and you know. I went to the restaurant yesterday, I got some delicious chicken wings, some grilled chicken wings and I look around and everyone, this is on a Sunday, everyone’s drinking mimosas and bloody Mary’s and whatever else and the majority of the people are obese and they’re getting pretzels and nacho cheese and then they get donut holes delivered to their table and then they get a sandwich with like six pieces of bread and the cheese is going off the sandwich and then they go and get chocolate cake afterwards. It’s like, my goodness, just imagine how much better we could be if people just had chicken wings like me for lunch. I didn’t have donuts, I didn’t have queso, I didn’t have freaking pretzel, I didn’t have bloody Mary, like, come on. People, it’s like, they don’t care about their health until they are forced to care about their health but by the time you get to that point it’s already too late so I guess my little rant here is just, I really want people to start taking their health seriously now. Stop waiting until you're at rock bottom before you decide you wanna change things. Use this information that Dr. J and I are providing and implement it now, like, people listen, listen, listen and then the implementation is just not there. I really hope people implement the stuff you and I talked about.
Dr. Justin Marchegiani:100%. So, I mean, out of the gate, I mean, of course, you know, you have caught people on a bad day, maybe they’re 90%, you know good and 10% off and you caught them on their cheat day, right? But odds are that’s probably not the case but we have patients who are really good and may have a bad day every now and then. And so, hey fine, if you’re doing great and you’re on point and you’re in great health and you want to cheat every now and then, I always recommend trying to choose the least damaging cheat possible, right? That probably isn’t the best example of that but in general, food plays a major role, right? Because food’s gonna have nutrients to run your immune system, right? Our fat-soluble vitamins, our antioxidants, you know zinc, magnesium, selenium, all play major roles with the immune system. Our antibodies are made from proteins so if you’re not getting and digesting good protein, you’re not gonna be able to make good antibodies for your Th2 immune response and then obviously, if you’re eating inflammatory food, the more omega-6, the more you stimulate your prostaglandin E2, that’s more the side inflammatory side, the more you’re gonna have unprovoked immune responses and you’re just gonna be chronically inflamed and then you may have this cytokine storm we talked about because you don’t have good balance to your immune system and so, also, on top of that, right, we know how much carbohydrates, especially refined processed carbohydrate. It feeds a lot of bad bugs. So, if you have a lot of fungus overgrowth, yeast overgrowth, bacterial overgrowth, these bugs prefer refined processed foods, right? It’s gonna just be easier to digest, easier to feed them and so you’re gonna create overgrowths like that. And these bad bugs, obviously, produce other types of toxins in your body, right? Bad bugs eat your nutrients and poop. And then, instead, versus eating your poop and producing nutrients, right? Bad bugs take the nutrients you’re eating and they’ll produce more toxins and endotoxins and different metabolites, lithocholic acid, etc., versus producing B vitamins, producing vitamin K, producing different beneficial acids that prevent the colon from overgrowing, right? Probiotics, acidophilus, literally, translates to acid loving and so good probiotics actually produce and lower the pH in the intestinal tract which actually makes it harder for bad bugs to grow, right? Bugs tend to prefer an alkaline type of environment to actually grow in the lower intestines.
Evan Brand: That’s a great point. I don’t think many people know that about acidophilus. I’m glad you broke that simply for people that you actually want lower pH environment because that’s not really a place for these pathogens to thrive versus when you’re on proton pump inhibitors, for example, acid blocking medications or if you’ve got an H. pylori infection, you’re gonna have that higher pH, you’re gonna have that more alkaline gut and then that’s where things really get into trouble, I mean you and I, I think we’ve done a whole podcast on this but the brief spark notes are lower stomach acid, age, stress, not chewing your food, that’s gonna increase malabsorption and feed the bugs too. So, this once again goes back to the same thing and we’ve said 100 times you get your gut tested. Figure out if you’ve got this overgrowth going on. Don’t wait until you’re in a critical situation. We got to get your gut fix now. Think of working on your gut as preventative medicine. How revolutionary is that?
Dr. Justin Marchegiani: Absolutely. And then also, when you consume too much carbohydrate, we talked about how you’re gonna feed the bad bug. We talked about what the bad bugs do in regards to impeding nutrients, adding more toxins, pooping poop, right? There was one more thing I wanted to kind of highlight on that realm, we talked about the gut permeability and the overstimulating immune system. Also, high levels of carbohydrates, glucose looks very similar molecularly to vitamin C and so you have these macrophages, little Pac men and Pac women that go along in the lymphatic system and in your bloodstream. They gobble up bacteria, gobble up viruses, gobble up crud.
Dr. Justin Marchegiani: Also, high levels of carbohydrates, glucose look very similar molecularly to vitamin C, and so you have these macrophages. These little pacmen and pacwomen that go along in the lymphatic system and in your bloodstream. They gobble up bacteria, gobble up viruses, gobble up crud. Vitamin C kind of docks on that macrophage and and kind of supercharges the macrophage so it can gobble things up more. Guess what glucose can actually come in there, and docks on that macrophage, and it can decrease the macrophages' ability to gobble things up. Now in literature, the literature logs to make things confusing, so there's kind of like two sets of language. There's like the lay language right where we're kind of communicating it in a way that everyone gets it. In the literature, they'll call it the phagocyte index, right P-H-A-G-O-C-Y-T-E-S, so phagocyte with a P-H, right? So go on PubMed, type in phagocyte index and you'll see, that's the macrophage. The ability to gobble critters and bacteria up, and so if we decrease the phagocyte index, it's going to be just they're not going to be able to gobble things up as much, and so this is really important and so high levels of glucose, high levels of insulin, which, again, glucose and fructose stimulate insulin production, right? And so, you're going to have. Less gobbling of your pacman and pacwomen in your bloodstream to be able to control these critters.
Evan Brand: That's crazy. Ok, so you're saying if I’m in the hospital and the nurse or whoever brings me my lunch, which I saw when my grandmother was in the hospital couple years ago for heart issues. You know what they brought her for lunch? It was this little like packet of peanut butter which was corn syrup and like peanuts. And then I think it was probably a piece or two of bread and then it was a little Jelly packet. And guess what that was? Corn syrup and like fake artificial flavor and purple dye and whatever else. So, you're saying that's not the optimal diet for good macrophage. I guess you would call it bug eating per southeast.
Dr. Justin Marchegiani: No. One, it's going to feed a lot of despotic bacteria. Two, it's going to decrease the phagocyte index, so your body's ability to gobble up the bacteria and such. And then I would say on top of that, the more insulin resistance you have, 'cause, how, how It works is right? You take in glucose, you take in fructose, right? When there's fiber attached to it, it actually decreases; glucose and fructose is damage. I.e. like if I consume some fructose from blueberries 1, there's a bunch of antioxidants with the blueberries. Bunch of different course. It ends and bioflavonoids and vitamin C on that. There's also fiber so fiber kind of blunts the effects that you may get from fructose when you consume things like blueberries or strawberries. But when you consume fructose without the fiber, i.e., high fructose corn syrup, right or table sugar, which is sucrose to gross is fructose and glucose. High fructose corn. Syrup is just like 55-45 fructose to glucose. Where table sugars, half and half right? When you consume it without the fiber and out the nutrients. What happens is the body says ok, we gotta go store it in the liver. So, in the 1st place it goes to to dump that fructose is stored In the liver. Once the the fructose sources are done. There can't store it anymore. It starts to convert it. With that, and then once the liver starts getting fatty, all this fructose just hangs around in the bloodstream and it's creating all this oxidative stress. It's like putting a barbecue sauce right on your chicken before you barbecue it. It creates this browning effect. And so when you have all this high level to fructose in your bloodstream because your liver saturated, your liver is now fatty. It can't store anywhere else. You have high levels of insulin now you start browning all the arteries. And then what does that do? It creates inflammation and makes your platelets and your blood cells just more sticky. So you have increased chances of clotting. What's going to happen when you have clotting in the lungs? It's going to create a whole bunch of lung stress, right? Obviously hard issues if it's in the heart. Brain issue is in the brain. And so if we can get the fructose and the high levels of insulin down, one, that's going to help blood flow. It's gonna decrease your oxidative stress reserves and so when you have high levels of oxidative stress, what does that? Due to your needs of vitamin E and vitamin A and vitamin C? It increases it, because your body is having to put out these fires and think of these antioxidants is like the fire extinguisher. So, it's wanting to use all these antioxidants. And of course the fuel that feeds a lot of this stuff is going to be high sugar and crap that also feeds the bacteria, which then makes the immune response worse so you can see all these things, they kind of compound on each other one after another.
Evan Brand: Yeah, yeah, that was a great way to put it out so I was kind of picture in my head. This snowball effect that gifts. You and it gets nasty quickly.
Dr. Justin Marchegiani: It does. It really gets nasty.
Evan Brand: And then if you're really, really bad and then you're on the feeding tube, I mean we've seen, and I know you've talked about this before with your some of your work in the medical industry years ago. I mean, you've talked about some of this stuff they feed people. It's it's bad. These feeding type solutions. I mean, I'm pretty sure it's just straight garbage. I don't have an ingredient list in front of me, but I know it is not good.
Dr. Justin Marchegiani: Yeah, 100% and uhm… You know sugar is used, it hits that opiate receptor, right? It's, it's people use it to kind of modulate pain, modulate all the bad stuff that's happening so it's you know it's very addicting. You know, once you're stuck on it. We had a question come in, “How do you test for some of these things with the bacterial overgrowth?” So you can do a SIBO breath test Lactulose breath test. We can do one of the different organic acid tests that we'll look at some of the bad bacteria metabolites like benzoate, hiparate 2, fat 2 3 phenylacetate, Indicam; These are different organic acid or bile acid markers that we can look at. Will also run good, comprehensive DNA stool tests that will look at some of these bacteria, and if they're overgrown right, some of the common bacteria will see, or Klebsiella, citrobacter, prevotella, morganella, Pseudomonas, right? There are some of the common ones that we'll see, and there will be elevated way outside the reference range when this happening.
Evan Brand: Yeah, you've got strep. You've got staff. We'll look at Candida on the stool, even though it's not as accurate as the urine will look at. The parasites too. What about like blasto and crypto and Giardia? What about H. Pylori infections? All these things add up against you, so our goal is really trying to get everything on paper and figure out what all you're up against and the. Cool thing is. A lot of times, you and I are knocking out infections that maybe we didn't even know were there because we can't test for everything like we have really, really good testing. But I'm sure there are still different pathogens that we don't even know, but the cool thing is with these herbs and with these synergistic formulas that we're using clinically with people is that you may have some antiviral, antifungal, antimicrobial antiparasitic properties all to these same compounds. So you may knockout 4 different infections with the same nutrient as opposed to, let's say a specific drug designed to target a specific pathogen, like an anti-giardia antiparasitic medication. Whereas herbs we may come in and knockout, giardia plus crypto, you know. Plus the H. Pylori all in one fell swoop, so that's the benefit and not to mention. Let's say it's berberine, that we're using for antimicrobial support. We may help support glucose there. We may, with some of these.
Dr. Justin Marchegiani: Yeah, yeah, there's some of that.
Evan Brand: We may. We may lower inflammation at the same time as we're eradicating the infection, so that's just really beauty. Once you get the data, the beauty is that you can work on multiple mechanisms at the same time getting someone to the finish line fast.
Dr. Justin Marchegiani: Yeah, and also when you take some of these herbs, these herbs are going to have antioxidants in it so the oxidative stress that you kind of create with the killing of these microbes. These herbs are going to have some antioxidants present in them just due to their their phyto signature. Obviously when you take in an antibiotic, right, you're not going to have a lot of nutrients or antioxidants present with that. They actually they can create more oxidative stress. Just going to PubMed type in antibiotics and oxidative stress or antibiotics and mitochondrial stress. There is a study supporting this, so the part of the benefits with the herbs is that you're going to get some antioxidant nutritive properties 'cause based on their phyto signature and again, this is all going to be dependent upon. These herbs being higher quality right, not cheap ones, and if they're grown in soils that have high levels of lead or mercury then that could obviously be a negative impact. So we want to make sure we're sourcing out high quality herbs. That's why we want to have a professional grade where we have third party testing on them to make sure they're adequate. The next thing on top of that is there's synergy between some of these herbs. So, for instance, you talked about berberine's right very helpful. Barbarians also help modulate lipids, right, triglycerides, cholesterol, right. They also help with blood sugar and guess what? Berberine's combined with warm wood our shown actually have antiviral qualities which is very helpful. So if you have any kind of lingering viral stress that can also be very helpful. I see people when we do gut killing, they, they may start to flare their herpes because their immune systems going after it. Sometimes that can happen too. Or there may be very helpful with their EBV or something else going on in their bodies. So we gotta keep an eye on all those things.
Evan Brand: That's cool. Yeah, that's really fascinating. Oregano 2, right? We love oregano will use that as a broad spectrum too. That has a lot of cool different antiviral into microbe properties olive leaf is another great one. That we use and…
Dr. Justin Marchegiani: Yep, olive liters of antiviral properties to anti inflammatory for sure.
Evan Brand: Sure, and it's gentle. You know some of these things are just so gentle that even in young children that were seeing with these issues, I mean, I know with you and. I you know. I've actually had couple clients, they they've really tooted you and eyes horn. They say you know that you and doctor J or kind of the only guys out there with young kids that actually are doing functional medicine because so many people are doing like, functional medicine theory you know? Or maybe they're clinician and they're older. Maybe they don't have kids, so I wanted to pass that feedback on to you that are our clients. They they really love that about us that we've got young kids, 'cause we're implementing this stuff with our kids too. I know you and I have both done antimicrobial nutrients and other supportive stuff for our children, and it's been really great because there's so much fear and I, I guess you would just call it misinformation when it comes to to kids. Kids are so resilient, but they do sometimes need help and you know, you'll often get the recommendation or the the comment that, Oh well, the pediatrician doesn't know anything about that. For the kids, I will tell you, personally herbs are great for kids and we use protocols and kids all the time. There's so much to be done with kids.
Dr. Justin Marchegiani: 100%. So, just kind of out of here just if we kind of re summarize what we're trying to, you know, make sure you. Guys extract from here. Is number 1, beneficial bacteria is going to help modulate the immune system, decreased permeability, immune permeability, which or gut barrier permeability, which takes stress off the immune system. it's going to modulate the cytokines the interleukins. So, when your immune system comes in there you're not going to create more damage from the immune system, so it's kind of like the firefight is coming in and you have a small fire and instead of putting it out with one of those portable little fire extinguishers they bring the whole big ladder and truck in there and spray so much water they knock down all your walls. It's kind of like, well, that's kind of an inappropriate response to that kind of fire. Same thing with your immune system. We don't want your immune system to be creating stress and inflammation because the response is inappropriate, right? We could see this with other stress infection. We see it with allergies, right? And so we want to make sure we have good immune stress. We want to make sure that your gut is healthy where it's extracting all of the nutrients we're putting foods in there that aren't feeding the bad bugs, but also providing lots of good beneficial healthy fiber and healthy full spectrum antioxidants and nutrients that help the gut in the immune system as well. Any comments on that Evan?
Evan Brand: Well, you know that just kind of spurred the five and we could do a whole Part 2 on this, but I mean there is a role of some leaky gut support outside of probiotics. During this, you and I have our own custom professional formulas that we use with various nutrients like Aloan, Muk and cama meal and other things that you can use to actually support the gut lining. So this would be another great thing to. Implement if you're in these situations, maybe you're unable to get testing because you know it takes. You know, couple weeks, turn around time or a little more, depending on what you're doing. So if you're kind of in a more acute situation, I think not knowing what you're up against, you still could bring in some of these leaky gut supports now. And then if you're in a situation like I'm telling you to wait before you hit rock bottom, wait before you know, don't wait before you hit rock bottom. Don't wait before you have to go. To the hospital work on your gut now. If we have all the data we can work you through these steps here and then we may have already gotten you to the gut healing point to where you're not coming into this infection with a leaky gut. I would much rather someone come in with a healthy gut. We know we're gonna, they're gonna do far better and with this discussion you and I talked about today of the gut-lung axis, now is the time to focus on your gut, so you don't have to focus on your lungs.
Dr. Justin Marchegiani: 100% and it gets great. Makes a lot of sense. So you guys listening to you enjoy today's content here, we'll put a list of some of the products that we use. Some of the probiotics that we that we specifically like in use with our patients. I'll put some of the the immuno-nutrients that we'd like to kind of modulate the breathing pathways- quercetin stinging nettle-all excellent. I love ginger tea as well, we'll put that in the links down below those are all excellent things. And of course some of the herbs that we like as well will put some of the clearing herbs that we like for the dysbiosis and such in the comments or in the comments, ah description below. And if you want to support us, you can purchase some of those things there. If you also want to reach out, we're available for functional medicine consultation support all around the world. Will put that link down below as well; evanbrand.com to reach out with Evan. Doctor J, justinhealth.com to reach out with myself. Thanks so much. Evan, any last things you want to highlight?
Evan Brand: No. That’s it. If people need help, feel free to reach out. We're here for you. We'd love to help you do, do an overhaul. You know what I mean? If we got to look at your system, let's look at your system. Please reach out if you need help. Doctor J at justinhealth.com me, Evan, evanbrand.com. Would love to help you and we're here for you.
Dr. Justin Marchegiani: Awesome! Alright. Have a good one everyone! Take care. Bye now.
Evan Brand: Take care. Bye, bye.