
Regular blood testing is one of the most important ways to keep track of your overall physical well-being. Getting tested at routine intervals can allow you to see how your body changes over time and empower you to make informed decisions about your health. Here's Dr. J and Evan talking about the areas to check aside from the usual blood tests we know.
A conventional medical doctor will typically recommend that you get routine blood work, but this is the bare minimum. There are several significant reasons you may want to get blood tests more often than that. Either you want to optimize your health or to reduce the risk of disease and health complications.
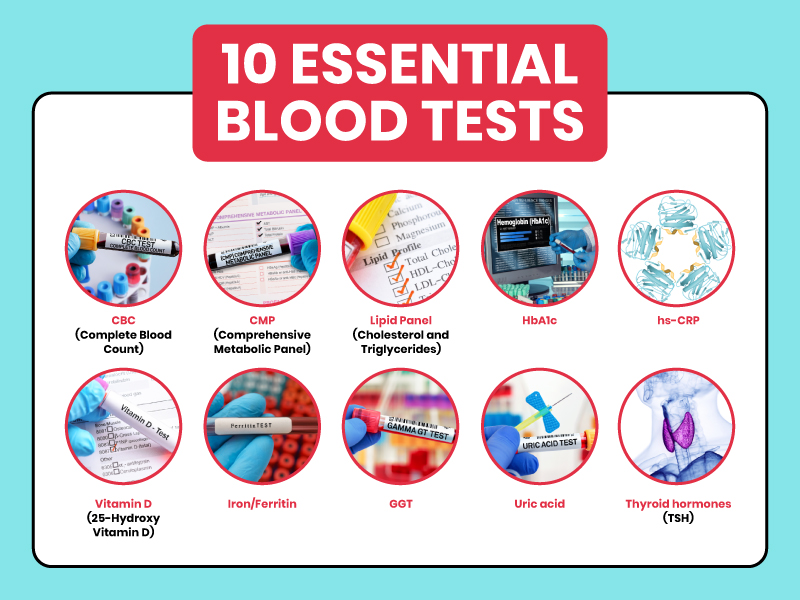
What are some routine tests and others that you should ask or know? Aside from CBCs (Complete Blood Count), Dr. J and Dr. Even pointed out enzyme markers, cholesterol tests, blood sugar tests, liver markers, thyroid panel, and so on. It will help your doctors make a differential diagnosis and dive into the root cause of your present health status. To know more, check out this podcast.

Dr. Justin Marchegiani
In this episode, we cover:
3:12 Conventional Side of Blood Works
12:14 Thyroid Panels
17:56 Blood Glucose
23:50 Adrenal Issues
29:33 Lipid Panels
Dr. Justin Marchegiani: We are live. It's Dr. J here in the house with Evan brand. Today, we're gonna be chatting about blood tests that we use to help assess our health and help us get better. So we're gonna be chatting a little bit about kind of intro blood tests, what the best tests are kind of what our perspective on that is, Evan, how are we doing today, man?
Evan Brand: Doing really well excited to dive into this topic, I went, got my blood work. And I got my wife's blood work done on Friday. And I just want to give a brief little note on how you and I run blood work as clinicians because it's very easy. And it's so convenient, because we don't have to go and beg a GP or an MD and say, Hey, please, please, doctor. I mean, you and I've heard countless stories. Yeah, I asked my doctor to run this, they wouldn't run it, I asked my endocrinologist to run this, they wouldn't run it. With us, the accounts that we have with our credentials, were able to order and create customized lab panels. So you and I both have created customized blood panels that with a click of a button, we can go boom, order it for anyone, whether it's ourselves, or our clients or patients, and then we get an instant requisition form. We go straight into labcorp request, you check in, you sit down, they call your name, you hand them the paper, you get the blood draw, you go home, it is so amazing. Every time I get my bloodwork done, I'm like, wow. And I didn't have to get anyone's permission to do that. But my own.
Dr. Justin Marchegiani: Isn't that nice? Yeah, it totally is nice. Also, there's the big insurance scam, right. So because we have accounts directly with the lab companies, we can order tests, and typically we get, you know, an 80 to 90%. You know, discount in price compared to what the insurance would bill. So like my typical thyroid panel, full thyroid panel that I charge my patients probably around $120. And the insurance would typically charge a patient for that well over $1,000. So then patients, most patients don't get 100% coverage, right, especially if you're not in network, and then the doctors can't ever retest, but once every six months, so then you're you're stuck not being able to ever retest. But they think, Oh, I'm gonna get coverage for this. And then they get 90% coverage, and they end up paying more money. For the for the 90% coverage, even though they paid 100% cash, it had been cheaper. So that's kind of the insurance scam. And then the problem with that is they can't retest but once every six months, so they're kind of stuck. So yeah, it's really nice to be able to order what the patient needs and to be able to reorder and reassess. Based on a time that is good for us. Not good for the insurance companies. That's kind of nice, right?
Yeah. And you're kind of we're kind of circumnavigating that conventional system where you're waiting two, three months, and then you get a bill in the mail and you're like, oh, medical bill, What's this about? And then it's like, oh, you owe 700. with us. It's all transparent. It's up front, you pay, boom, boom, boom, you're done. I've already paid for it. I know that I'm not spending another penny. And the turnaround time is insanely quick to like one or two days, typically on some of these panels are running. So let's go into some of the details. Now, let's quickly compare and contrast. I think you and I have a lot of fun. Like where we did our conventional functional medicine vers conventional medicine, gut workup. Let's talk about the same with bloodwork. So if you go to your doctor, and you have them say, hey, Johnny, we're going to run your blood. What is that going to look like?
So conventional medical doctor, they're typically going to do a CBC, they're going to do a metabolic panel, they'll probably do a lipid panel that's usually going to be at maybe a year analysis, that's kind of it. So like on the CMP they're kind of looking at liver enzymes. They will look at some electrolytes on the liver on the CMP as well. Those liver enzymes electrolytes, maybe some protein markers there, they'll probably look at glomerular filtration kind of some baseline kidney function with creatine and and bond. The kit the liver markers are going to be a lt and as to the liver enzyme markers, the gallbladder is ggt but probably look at some bilirubin your electrolytes are going to be sodium chloride, potassium magnesium, all serum not not intercellular which is a difference Okay. And then on the red blood cells are going to look at red blood cells RBC some adequate hemoglobin that's part of the CBC right complete blood count which is going to help be helpful for anemic patterns right low iron right, although also run indices which are MC VMC, HMCHC right me corpuscular volume me corpuscular hemoglobin me corpuscular hemoglobin concentration. When those markers go high, that tends to mean that we're dealing with B vitamin issues like b 12, full eight issues, and we call that megaloblastic anemia. So we have two kinds of anemia. As we look at big cell anemia is right we tend to be more B vitamins stuff. And then small anemias. We tend to be more on the red blood cell hemoglobin hematocrit, low iron side, and then we have immune markers, whether it's neutrophils, lymphocytes, eosinophils, monocytes, and basophils, which could be from bacterial issues, parasite issues, gut inflammation issues, viral issues. And then I would say on top of the CBC, that's pretty much it and then your limits. So total cholesterol, triglycerides and then of course, your LD vldl pattern, and then there's some add ons that we may talk about whether it's c reactive protein for inflammation, fibrinogen, for inflammation, homocysteine for inflammation, methylation, vitamin D. and we can kind of go into each one of those in regards to what we think is important on the functional side. But you know, the whole lipid thing is, it's kind of overplayed, right people think that lipids are a really important issue now once you start going over 200 or so on the total cholesterol, and that may not be. And we'll talk about the ratios and the perspective that we add to when we look at it.
Evan Brand: Yeah, so the way you talk, it sounds pretty good. It's like, oh, wow, that's a lot of stuff. But truthfully, there are rarely issues that show up on just standard bloodwork. Now, if you have more of the functional training that you and I've had regarding blood chemistry, you can kind of, I guess you would just say pick through the CBC with a fine tooth comb, and you can really look and maybe find some functional issues, like for me, I know that I you know, for a very long time, my hematic crit, you know, I've always had the hematocrit be a little bit high, which, based on some of the training you and I've had, it would indicate that there's probably a dehydration issue. And that's tough. You know, it's, it's, it's tough to stay hydrated. And so even if I mean, I'm sipping on water all day, but you know, I've heard there's a big influence on anti diuretic hormone, and all of that when you're exposed to mold toxin, that's a conversation for another day. But anyway, unless you're really looking with a with a fine tooth comb, conventional bloodwork doesn't reveal much. And you may see a little bit of this a little bit of that, but it's not, I'm not making too many protocol decisions based on a CBC I would say.
Dr. Justin Marchegiani: So when I look at blood, it can give me a good area of where to where to look next, or where to dive in deeper, which is helpful. And then if we look at it, using the optimal reference range, or a functional reference range, we can definitely glean better information. So the problem with most conventional medical doctors, they're looking at blood through a pathological range, they're trying to pick up like major disease patterns or pathological patterns. And so how it works is you have to show you have all people kind of fit in what's called the bell curve. And the typical range is going to be two standard deviations to the left and right, this is represents about 95% of the population fit into the so called normal. So you have two and a half on the high two and a half on the low that are on the high or low side, pathologically, right. And so the problem with that range is it as people get more unhealthy and sicker. And as those sick people tend to test more, what happens to the lab reference range over time, it gets wider. And so it becomes more encompassing, it's like having a bad field goal kicker and you make the field goal every year wider and wider and wider and closer and closer to compensate for the lack of, you know, good kickers out there. So it's kind of like that. And so what we do is we kind of narrow up that range a little bit, and that narrower range helps us pick things out before it becomes a problem. So let's kind of go over a couple of things. So with women or people that are vegan vegetarians, women, because they bleed more when they're when they're at menstrual age, right, typically 50 or below 48 or below, they can be more anemic. So we may look at things like lower red blood cells, right, red blood cells, you know, below 4.2 or so we may look at hemoglobin below 12, we may look at him at a crit, you know, in the mid to low 30s as a sign that there could be some low iron issues brewing, we may also run an iron panel, it's not typically run, but we may run things like ferritin, or iron binding capacity. Or we may look at things like iron saturation to get a window of low iron, for instance. And that's commonly missed, because what most conventional Doc's do is, their threshold for low iron is really low. And there's a lot of women I see in vegetarians in general that could be on that lower side could be a little bit anemic, and then they're not going to be able to carry oxygen throughout their body adequately, which makes a huge difference in energy and stress and and mitochondrial function and thyroid function because you need to be able to carry oxygen to have good energy.
Evan Brand: Yeah, let's go into some of the more let's let's, let's break some of the stuff down. But before we break it down more, let's hit on what are the things that that we're going to run and so I've got my panel pulled up that I ran. And so I'll kind of run through some of these things. But as you mentioned, ferritin that's typically not going to get run I've rarely rarely seen fair to run by anyone. The iron saturation as you mentioned the iron binding capacity. That's really wrong. That's right to be ti BC. Often on your bloodwork, the vitamin D. I mean, my God, it's so important, but yet vitamin D to this day is still not commonly run. Nope. And if they run it, they may run the wrong one. I've seen people where they don't run the 25 o hydroxy. tryptophan, they're going to run like the even the beat the D two. They're going to run the What is it? Ergo?
Dr. Justin Marchegiani: Yeah, the vitamin D too. Yep, Ergocalciferol.
Evan Brand: Yep, yeah. Ergocalciferol? Yeah. So you have a vitamin D, they may run the D two and you're like crap I needed to d3.
Dr. Justin Marchegiani: Yeah, the [inaudible]. The animal base kind of the d3 is the more active form. The D two is the more plant synthetic form, typically made from lanolin. A lot of times, that's the D two, that's the ergocalciferol. Ah, so vitamin D is really important. And then the range on that is pathological as well. They want above 20. Why? Because they're looking for rickets, right, the bone bending disease, right, because d3 helps absorb calcium and helps a calcium get into the bone. So we want 50 to 70 or maybe 70 to 100 if we're autoimmune or cancer risk. So vitamin D is a big one, I would say also on the CBC, we may be looking at immune cells, if I see low white blood cells, you know, below four and a half. There could be some you know, deficiency issues if there's high white blood cells, you know, greater than seven and a half there could be some immune stress. Now we look at the, the immune cells, how do we look at those never let monkeys eat bananas, that's the mnemonic device and doctor at school we learned so neutrophils we want to see, you know, below 60 lymphocytes, we want to see mid reference range when we see high neutrophils or low neutrophils and elevated lymphocytes. That's a common h pylori or bacterial infection pattern. If we see elevations in eosinophils, greater than four, we're thinking potential parasites or chronic environmental allergies by sea monocytes, greater than 10. I'm thinking some kind of intestinal inflammation. So we there's different, you know, patterns you may look at, when we look at some of these immune cells. That's very important. But unless it's very high, they're typically not going to say much. And if it's very low, they typically don't say much either there.
Evan Brand: Yep, so also more advanced thyroid markers. It's very, very sad how many people go to even an endocrinologist and they may only end up with a free T for possibly a free t three, but even that's not guaranteed. Maybe a total T for you may get Of course, TSH is going to be on there. But you and I are definitely going to be running like thyroid globulin, I mean obat antibodies, we're going to be running t TPO, thyroid paradoxus antibodies, maybe TSI, sometimes if we think there could be something else going on next. And then you've got the uptake of T three, what else you got? You got reverse t three that we're going to be looking at. That's an awesome marker. And that's never run.
Dr. Justin Marchegiani: Yeah. So when it comes to a thyroid panel, you already mentioned it, most conventional endocrinologist and primary care are going to run TSH because that's the major screening brain hormone, not a thyroid hormone majrooh. It's not a thyroid hormone, but it's a major brain hormone that talks to the thyroid and you'd be lucky to get a T for total after that. But we know downstream is a lot of conversion issues and even patients that have normal TSH, guess what, especially if they're on Synthroid, which is a synthetic thyroid medication that's just T for many of them can't make that conversion. And that's a problem too. And so you can have adequate T for good TSH and low t three. And you may have a lot of thyroid symptoms. So it's really important that we look at things complete. And don't even get me started on thyroid antibodies, because that's almost never run and thyroid antibodies are the major mechanism why most people sideway glands aren't functioning properly because their immune systems have beaten the crap out of their thyroid for a very long time.
Evan Brand: And we're talking what I mean, you'd say probably over half of cases of hypothyroid are probably autoimmune based on what I've seen, what would your guess be?
Dr. Justin Marchegiani: Yeah, I would say that and some may not even come back on the lab test, but it's very helpful to be able to look at those we run TPO antibodies and thyroid globulin antibodies. And so my full thyroid panel nevitt, some kind of a TSH, T for free and total t three free and total TPO antibody, federal globulin antibody, and we may run a reverse d3 or an uptake. Those are all okay markers to add to. So that's kind of your complete thyroid panel. Let me just piggyback to the CVC. Is there anything else on the CDC? I think we hit it all there. We can go to the metabolic profile now if you want.
Evan Brand: Yeah, well, you mentioned like earlier, like CBR active protein c reactive protein, I guess it kinda depends. I mean, sometimes that standard, but a lot of times that's not an hscrp is, you know, going to be the same same section of the inflammation panel on your blood. So hopefully you get those two run together.
Dr. Justin Marchegiani: Yeah, usually CRP and cardio CRP is basically the same thing CRP, they're just, they're breaking the number down typically below two, I think the cardio CRP, they typically don't do it less than two or so. So when they you do a highly sensitive CRP, they're just breaking it down into a smaller number. Let's go we want to see that below one that's great as a good marker of systemic inflammation. And fibrinogen is great. We have for highly inflamed, we may see a lot of clotting happen. And fibrinogen looks at clotting factors, which is helpful. So if we don't have good fatty acids, good omega three omega six ratio or a lot of inflammation, a lot of trans fat, high blood sugar cells tend to agglutinate they get very sticky. And so it's nice to see where that stickiness that stickiness level is. And homocysteine is also another measure of blood inflammation because it's homocysteine is an inflammatory metabolite. That typically happens when there's not enough B vitamins B six and four And B 12. In their active form, that can be a big inflammatory issue there too.
Evan Brand: Yeah, that was a problem for me. Actually, I did have elevated homocysteine couple years ago and started hitting some more Foley and it fixed it. So it was fun to see how the blood correlated to that.
Dr. Justin Marchegiani: Yeah, you know, we're going to try to get as much of that which we can do leafy greens and high quality, you know, essential fats and meats, right, but that's good. And so metabolic profile, we may look at liver enzymes that could be helpful patients that have a lot of insulin resistance and inflammation, you may see an elevation in liver enzymes. What does that mean? That could be a non alcoholic, fatty liver, non alcoholic steatohepatitis, that's Nash or non alcoholic fatty liver, meaning your liver has stressed not from alcohol, but from typically too much fructose and junky carbs. So the liver is a people think the liver is just a big filter for toxins. No, it also has a major effect at regulating blood sugar, and is also a storage site for sugar, especially fructose. So when you over consume fructose from high fructose corn syrup, or, you know, just too much carbohydrate, in general, the liver really gets stored up. And then when that liver fully gets saturated, overly saturated with fructose, for instance, you start having all these up regulations of inflammatory enzymes called the the junk enzymes, the J, the J and K one enzymes, and you see a lot of inflammation and a fatty liver there, and you see it an ultrasound. And so that's a common marker seen those elevated liver enzymes, and it's good to be able to look at that.
Evan Brand: Yeah, I don't know if you've tested bloodwork much with people like in the middle of a protocol. But I've had a couple interesting cases where, while using binders, we've seen liver enzymes go up. And it could have been also parasite protocols and things like that, that were kind of interwoven with detox protocols. But I've seen liver enzymes temporarily go up during that. So I don't know if you pay much attention to that. But I've seen it and they always go down as soon as it protocols over so.
Dr. Justin Marchegiani: Even with some killing herbs, like worm woods, a common one that we may see a little bit of elevation and liver enzymes, people that are sensitive, some of the killing herbs, it could be a little bit of stress, is it just the herbs? Or is it the dead debris that is now mobilized from the killing of those microbes, it could be both. That's where adding things like binders can be very helpful just to kind of put handcuffs on those critters and escorted out of the body versus kind of having it go back into general circulation. also adding an extra glutathione support can be helpful too. Just to really support and tone if I deliver those are very important too.
Evan Brand: Yeah, well. And it's common for you and I to use some sort of a liver gallbladder support too. So we may be throwing in like some extra taurine or Mathionine or beet powder artichoke. And there's many, many things that I say milk thistle already NAC. So there's a lot of stuff we can do. But yeah, I just figured I mentioned it. Because if someone's listening and you happen to do blood work in the middle of a protocol, it's possible that the levels may you may look at him and go, Oh, my God, my liver enzymes, but it will go back to normal relatively quick after killing protocols over.
Dr. Justin Marchegiani: Exactly. Also, we may look at glucose, blood glucose is going to be on a metabolic profile as well. CMP panel, I don't love it as much, because most people that are going to get a blood test and they're getting pricked in the arm of the big needle, or they kind of stressed. Yeah, and so that the cortisol from that can really increase their blood glucose. So I like getting a really good blood sugar kit like this. And then you can measure your blood glucose during the day. So here's my little kit here. And so I have I use the keto Mojo now because it measures ketones, so I'm a little meter, I have my little pricker here from my finger, and then I have the blood glucose and the ketones. So this one right here is the blood sugar. And this one here in the lighter blue, this is my ketones. So it's kind of nice to have those. So I can test my blood sugar before I eat. And then I can do a one two hour three hour and play around with my blood sugar. The whole goal is the more you keep your blood sugar down after a meal and bring it back to baseline within two or three hours, the less insulin you're making, the higher it goes up and the longer it takes to come back down, the more insulin you're making. So it gives you kind of a good window how you're responding to food.
Evan Brand: Yeah, what I wanted to point out is that you're doing more functional analysis of glucose versus if you just go into your doctor once every six months, you get a morning fasted glucose, that's just not enough information.
Dr. Justin Marchegiani: It's not because the whole goal while you're just checking morning glucose is because you're thinking your food, so out of whack, that your glucose is now elevated as a result. Now the problem is most people haven't eaten in 12 hours. So for your glucose is still be out of whack. 12 hours later, the problem has to be pretty severe number one, and then number two, a lot of times it can be elevated not because of food, but because of stress hormones in the morning. And so the stress hormones, people say oh, I'm at 105. Yeah, but it just could be a good cortisol response in the morning called the dawn phenomenon that's raising that glucose. That's why you want to check it against your foods during the day. If you have a blood glucose issue. You're going to see one and two hours later, it's chronically elevated, and it's taken a bit of time to come down. So that's a better marker. Make sure you're handling glucose okay.
Evan Brand: Yep. How about hemoglobin A1C, this is something that for diabetics, obviously, this is hopefully going to be regularly checked. But for your average person that maybe has some issues, A1C is probably not going to be on your standard blood panel.
Dr. Justin Marchegiani: I don't love A1C, I used to like it. I don't love it as much, I find that when people's blood cells live longer, because they're more healthier, they have more time to accumulate blood glucose. So the A1C it's a part of the hemoglobin and they're looking at the coding, the coding of glucose on the outside of the hemoglobin, right? So imagine, like, you know, when you, you know, you go up into your car during allergy season, you can see like a big fixed swath of like pollen on the car, they're kind of looking at the swath of glucose on the outer part of the human lobe. And now the problem is, the longer your red blood cells are hanging around, the more time they have to accumulate that blood sugar. So it can be helpful to look at something. But if you're, if you're a little bit on the higher side, or like, let's say 5.5 or so, let's say under six, but 5.5. And up, it may just because your red blood cells are a little bit more healthier. So like, for instance, with my anemic women who may have a ton of blood sugar, right, a lot of carbs, because maybe they're vegetarian or vegan. Guess what? When you're anemic, your red blood cells die faster. So all my anemic women have A1C super low, like in the forest. And so it's not going to be a great marker when your red blood cells don't live that long, and we see it with our anemic patients.
Evan Brand: That's a good point. Good point.
Dr. Justin Marchegiani: If I see someone six or higher, yeah, it's helpful, you know, but when you're kind of in that subclinical zone, you're going to typically have to go back to one, a meter like this, to really look at it. And then also look at your fasting insulin, which is a better marker, because that's going to give you a better window, how much insulin you're making frequently.
Evan Brand: Yep, good point, that analogy is perfect. The pollen on the car. So good job there.
Dr. Justin Marchegiani: Right. And if you leave your car out there a lot longer, you're gonna get a lot more pollen. It's kind of like that, right?
Evan Brand: I'm always under five though, no matter what with a one C, I'm always right. 4.9. Somewhere in there.
Dr. Justin Marchegiani: Yeah, I'm pretty low, too. I'm always like, right in the low fives. 5'1 5'2. But I've seen a lot of patients in my career that have that have really good diets that have tested their blood sugar, have good insulin, and they'll still have a little bit higher on the a one C and I'm just like, yeah, it's just it's missing some people. That's all. It makes sense. The question is, what's the mechanism? And that's what it is.
Evan Brand: Yep. Makes sense. You hit the you hit the dawn phenomenon. So you know, cortisol that may be run via blood, although we don't really like blood cortisol too much. We really like more functional analysis of cortisol, like with urine or possibly saliva?
Dr. Justin Marchegiani: Oh, yeah. And part of the reason why we don't we don't like it, is it because when you're measuring a stress hormone, while creating a stress response, ie putting a needle in my arm, you may influence that a little bit, right? And so that's kind of the reason why we don't love that. And even if you're like, Well, you know, do the adrenals make cortisol fast enough after the needle happens to show in the blood? Well, it's not just that it's the fact that you're anticipating it happening. Therefore, you're replaying that stress in your mind all the way up to the doctor's office to go and then the elevator getting into the you're already making that stress hormone while you're anticipating what's going to happen.
Evan Brand: Yeah, you go in the friggin lab with the scientific fluorescent lights above your head. It's all awkward the quiet they got some like drug commercials on in the waiting room, Justin, and they call your name come on back. Yeah. So and, you know, also Not to mention, too, that that's just a snapshot, right? I mean, that doesn't tell us anything about what's happening at two or 3pm when you're complaining of that midday crash. So I really am not too interested about what happened at 8am. I'm really want to know what what's going on at 2pm when you're saying you need that third cup of coffee.
Dr. Justin Marchegiani: Exactly, yep. 100%. So it's, it's really important that you're kind of on top of that. So I think we hit some good blood glucose stuff, we hit some liver enzymes we hit. I'm thinking here, we hit some of the electrolytes. electrolytes are good, too. So sodium and chloride are really good ones. Now when I see patients that have adrenal issues, you could easily have low sodium and high potassium, or you can just kind of have lower minerals all together. Now the serum is not going to be the best marker for testing minerals. So when you see your minerals out of balance, you know, it's a big issue, but you could still have mineral issues. And the serum be okay, because it really matters what's in the cell. Not necessarily what's floating around in the blood. So think of interesting Imagine you're in a pool, okay? The pool is serum. Okay, you're in the little floaty. You're in the little inner tube, right? So it's you in the inner tube, right? You and the inner tube and the water in the inner tube that's intercellular. The water outside of the inner tube is extracellular serum. So that's kind of how you think of it. So when we test some of these nutrients, it's better to get a sample of the water in the inner tube with you that's intercellular versus the water outside of the inner tube. That's serum.
Evan Brand: Yeah, and how do people get that? What is look like?
Dr. Justin Marchegiani: Well, you can like we can add like a red blood cell serum or a potassium serum on some of these panels, we may run like a spectracell, or a Nutri eval or an ion panel that looks at more intercellular nutrients, we may look at different tests that allow us to do that. But there's not too many add ons for conventional testing like quest or labcorp. Outside of I seen a blood cell magnesium is good. You can do a potassium if you wanted. So there are a couple that you can do to get a window into that.
Evan Brand: Yeah, I was gonna say I looked through all the options for the conventional labs, RBC magnesium, I think that was about it. I think that's all I could find.
Dr. Justin Marchegiani: So yeah, not too much. But it's something you know, because magnesium is a big one, right? And with magnesium RBC, we want to see a greater than five on that one, red blood cell magnesium greater than five. So that's helpful. And then, of course, we mentioned magnesium surround, we want that greater than two. And then your minerals, you want them somewhat mid reference range, once we start going under 100 or so I think like sodium, it's like 104 is kind of mid range. If you're under 104, it could be a problem, potassium, I forget the exact ranges in it, but I want them all about mid range. In regards to the reference range.
Evan Brand: What do you feel about using conventional bloodwork to do like omega three omega six fatty acid panels, I know, there's some Doc's that are just so obsessed with all these ratios. But, you know, truthfully, if you're doing the things that we're discussing with our clients and patients for nutrition, you're going to pretty much be optimized anyway. I don't know what that would tell you. Besides, hey, maybe you need to do a little more this or that?
Dr. Justin Marchegiani: Yeah, it's a great question, I think, look at the person's food. Like someone could have really good diet, but let's say the meat and the eggs aren't pasture fed. Well, that could easily be the reason why your omega six to three is off a little bit. Or it could be that you know, you're just doing too much plant fats, and those plants or from coming from, you know, omega six bass plants soy or canola or safflower. So if you're doing good fats, like coconut oil, and olive oil and avocado stuff, which are monosaccharides are Yeah, so those are, yeah, those are MonEl fatty acids versus like, vs. poly, which is like a fish oil, right. And then so the fish oils, you have omega threes, right, which are going to be like, the ones that are we talking about that are going to be more on the anti inflammatory side, right? These are the Polly's. And then of course, the Omega sixes are going to be more on the vegetable side. These are going to be also Polly's but they're going to have six bonds, these are going to be your safflower canola, these are going to be your soybean oil, all of your plant based fats, most in the most of your plant bait fast, to extract the fats from them with the olive oil or maybe an avocado, you tend to have to damage the fats, they tend to be more damaged, they tend to be more on the Omega six side. And when you get when you eat plants by themselves, you're not getting that concentration of fats. And so you tend to not have that high omega six to omega three, when you're doing just vegetables by themselves. Okay. And so we can just look at how much fish you haven't per week, how much pasture fed eggs you have in a week, how much steak or meat that is grass fed, you haven't per week, and then you can kind of look at it relative to what's high on the Omega sixes like the knots and the seas and the refined vegetable oils. And you can kind of get a pretty good assessment of where you're at, which is like kind of for one or less. So four times omega six to one is pretty, it's pretty. Okay. And you can always run that omega three to six tests on the blood too. Does that make sense?
Evan Brand: It does. Yeah, I just find that it's not a huge needle mover. So I don't run it too often. I mean, I think it's cool to check in you could call it kind of a lie detector test as somebody says they're doing everything that's dialed in, but then you find out that Oh, they've been coconut grass fed steak, but it's been in this healthy heart oil blend that they found on the shelf and it was a safflower canola combo. You're like, Oh crap, then we missed it. And you got to get off of that stuff. So yeah, I mean, I was just gonna say so it's not really a standard thing. For me at least you know, I'm not running into often with people but-
Dr. Justin Marchegiani: But it's there it's an option and then it's something if someone wants to run we'll run it and so we have the polyunsaturated which is the fish oil or on the omega three side, right. And then we also have things like flaxseed oil, but it has to get converted to the to the higher up fatty acid so you know, omega three fish, and then you get to get some mega three from cows that are grass fed as well.
Evan Brand: What about particle size on a lipid panel? So we talked about that briefly. It's just a good add on that most people don't do and our friend jack Wolfson, he discusses particle size and I think it's something that more people are asking questions to their doctor about but it's still very uncommon to run.
Dr. Justin Marchegiani: People that have a cardiovascular history. Just want to run it to begin with. I think it's okay. I can almost always tell you what your particle sizes if you're eating good health saturated fatty acids like coconut oil and grass fed butter. And you're getting meats that are like good quality fish, good quality grass fed beef, egg yolks, you're keeping a lot of your junky fats down a lot of the refined sugar down and a lot of the trans fats down, you're going to have a large, you're going to have a particle size A, which means large and buoyant and fluffy, right? Think of a like you want an ad on your test. And then you have the small dense atherosclerotic particle size B, think B for bad, and the B for bad, more trans fats, more inflammatory, processed vegetable oils, more refined sugar. And so with patients, I almost always can look at their diet. And guess what that will be to begin with. So if I do a dietary check and do a diet recall, what's what's the average day look like? And I look at that and I get a window, it's pretty easy to predict that. And so we'll run it for patients that have a cardiovascular history, and they just want to know, but for the most part, it's not hard to predict it.
Evan Brand: Yeah. And when you see it, are you just tweaking dial? Like, if you see a bunch of small dense particles, or are you coming in? Are you using any kind of like plant sterols or anything like that, to help with it are you just tweaking diet, and then it fixes itself?
Dr. Justin Marchegiani: It depends how acute the patient is. But if it's if it's not acute, meaning the patient's not dealing with a heart issue right away, then we're going to just tweak the diet, and that's going to take care of it, we're going to add an extra omega three fatty acids from fish oil, we're tweaking the diet, we're getting the carbs down, we may be adding extra nutrients to manage blood sugar and manage inflammation. And then usually within a month or so you're gonna see a big change. After we retest. Awesome, yeah, usually once you get about 100 good meals, then you're going to see a big shift. A good average person is doing about 21 meals a week, right? So three a day times 721. So four to five weeks, once you get 100 meals in, if you can get them close to in a row. Your body has a huge shift in physiology.
Evan Brand: It's amazing how quick you can change stuff I knew. I mean, sometimes we get impatient because like what the detox piece like that takes longer. I mean, I'm here I am a couple years in detox and mycotoxins. I've still got some going on. So, you know, with that, it's like, oh, man, you get impatient. But luckily, with the blood, it's a quicker turnaround time sounds like.
Dr. Justin Marchegiani: Oh, totally, man. It's really important. So I think we hit some of the big markers today. I would say one other one for lipids. You know, I don't really care if cholesterol is a little bit on the higher side, just I try to make sure the cholesterol to HDL ratio is ideally you know, four. So if the if your Triggs are sorry if your total cholesterol is 200, and your HDL is 60, or what's that ratio to the math, put my calculator 200 divided by 60, that's 3.3. That's pretty darn good. Usually, when you're under three and a half, that's half the average risk factor. Okay? When you let's say you're at 242 40 divided by 60. On the HDL, now you're at four. And so I like to look at the total cholesterol to HDL because HDL is what recycles cholesterol. Okay? So if you have good recycling lipoproteins, ie HDL, that's a good sign. And then I'm also going to look at my trigger to HDL ratio, we want that under two. But if we can have a closer to one, that's wonderful, what does that mean? Take your trig number, let's say your trig numbers at 60. Let's say your HDL is at 50. Well, what's that? What's that number? Well, we do 60 divided by 50. We're at like, 1.2. That's good. So we want to under two but closer to one's ideal. That's a really good marker. That's my insulin resistance inflammation marker for my limits. So I'll look at trade over HDL. That's a really good marker.
Evan Brand: Yeah, you know, I talked to jack one time about the, the blood and I said, When do you start getting freaked out regarding total cholesterol, because if you talk to a conventional cardiologist, they're they're brainwashed on that 200 number. And he says that he's got people up in the 450s, that he's not worried about 1%, like total cholesterol being 450. And it's not an issue. So he just talks about, like he said, ratios, inflammation associated with it, you know, then you get into more trouble. But I mean, the total number, I mean, he acts like it's just minimally important.
Dr. Justin Marchegiani: Yeah, on its own, I would be a little bit concerned once you start getting in the mid 300. Just because that's that could be more hypercholesterolemia. And that's not necessarily a diet thing, that's more of a genetic thing where you're making a lot more cholesterol. So I personally would get a little bit more concerned with that and I'd be monitoring that. But it's hard to really jack up your cholesterol when you're keeping inflammation down. Like I just did a blood test for my lipids last month, and my cholesterol my total cholesterol and you know what I eat man? I good fats, good proteins, good eggs, good fatty acids. And my total cholesterol was at 165.
Evan Brand: Whoa, yeah, I was like a 202.
Dr. Justin Marchegiani: Yeah, 165 my my trades were at 60. And my HDL is we're at 50. So I had like a 1.1 1.2 ratio for trigger over HDL, which is great. And so most of the cholesterol, you're gonna Ahead is gonna be made by your body. So when it starts getting too jacked up and your diets good, you know, we want to look at thyroid hormone, maybe that could be a big thing. And there could be a hypercholesterolemia genetic issue, and we can always run a genetic test for that to see what's going on. And if that's the case, what are natural things you can do to get your cholesterol down, you can do higher dose berberine to make sure your thyroids check, you can also do some potential plant sterols as well. But get that check. So my philosophy if it goes a little too high, I'm curious, I'm worried about the hypercholesterolemia piece.
Evan Brand: Yeah, and I don't mention that 400 number just to get people off the hook. I just thought it was interesting that that's what he was saying. And he's probably talking like, you're in big trouble if you get to that point. But But anyway, so that's rare, though.
Dr. Justin Marchegiani: That's super like these are very, very rare situations, you know, sub 1% of the population are going to be there. My never seen it ever. I have two patients with that. But most people already know about it, because someone in their family already had been picked up previously. Yes. So most people already know what especially today, you know, maybe 3040 years ago, not as much, but people that have had those issues have already been picked up. They already know genetically, if it's in their family, and then once you know genetically, if it's in their family attend to get tested for it.
Evan Brand: Yep. Right? Well, let's wrap this thing up. So as we mentioned, bloodwork is a piece of the puzzle. If you go to a practitioner, and they're like I'm going to analyze your blood and tell you everything you need, they're wrong, because you mentioned some of the clues into the immune section about parasite infections and all that. However, I will speak for you and say that you're not going to depend on that bloodwork solely to identify parasites, you're still going to be running comprehensive genetic DNA based school panels, you're going to be running organic acid panels to look and deeper. So yes, you may look at those things. And I think it's awesome that you gave us some insight into that, however, I'm not going to go to a guy who's going to look at the blood and say, Yep, you've got parasites, let's put this protocol together, I'm going to want more data. So blood is just part of that data. And it can be helpful, especially when you're working with autoimmune people, because you and I like to look at these antibodies, and it's very fun and satisfying. And it makes you look better when you could have a a woman come in with a TPO of 1000. And all you do is fix her gut and our TPO antibodies go down to sub 200. That's exciting.
Dr. Justin Marchegiani: Totally, that's huge. So I think today is very great, great podcast, because we're talking about actual things. We want people to kind of like say, Hey, you know, what's it like to be inside Dr. J, and Evans head, and this is kind of it. And everything that we look at, we're kind of like a detective, we're putting like checkmarks in the column over here that support us going in this direction, or going in that direction. So we add up all of our checkmarks, right, and we're kind of create what that differential diagnosis is, and what tests we're going to do to dive in deeper in in whatever those avenues where those check marks are adding up. So that's kind of inside of our head, we're walking through you through our thinking. And if you want to dive in and reach deeper, you know, into work with a practitioner, like Evan or myself, you can head over to EvanBrand.com, you can schedule a consult with Evan or myself at JustinHealth.com. And you can schedule we are available worldwide to help y'all with your functional medicine and natural health care needs. And if you want to get to the root cause we're going to be the best person to to look at anything else you want to highlight here today.
Evan Brand: Maybe just one frequently asked question, Well, I'm not where you live. Does that matter? Well, in the US, it doesn't matter at all. We can run like a blood comprehensive blood panel, we can run that anywhere now. We'll try to help people internationally in regards to providing maybe some codes or things like that to help people. But at least for the us know, you location does not matter. We haven't had any issue with that. I think New Jersey for a while was getting a little more strict. But beyond that, no. I mean, nationwide, it's a piece of cake. So as we talked about the beginning, create a panel, send a requisition form to your email, print it go get your labs drawn, you're done. It's awesome. percent was in New York, or was in New York or New Jersey was one of them.
Dr. Justin Marchegiani: Yeah, both.
Evan Brand: They're both difficult. But was it for blood? Or was it for some of the functional or was it-
Dr. Justin Marchegiani: For blood, but there are some still some Malin fingerprick tests that we have accessible to deal with patients like that. So we still have options for them. Maybe not quite as much. And then if they're near the Connecticut border or the Pennsylvania border, we have also options there too, but we still have some mail and stuff. That's helpful.
Evan Brand: Cool, cool. All right. Well check out the sites JustinHealth.com. EvanBrand.com. We'll be back next week. Take care.
Dr. Justin Marchegiani: Excellent. Have a good one, y'all. Take care. Bye.
https://justinhealth.libsyn.com/essential-blood-tests-to-analyze-your-health-podcast-305