
By Dr. Justin Marchegiani
A recent study of non-celiac subjects shows a strong connection between gluten and depression. In conventional literature, only people that have celiac disease are supposed to be sensitive, but we now know you don’t have to have the full-blown symptoms of the disease to be gluten sensitive. The study concluded that short-term gluten exposure induced depression with no GI symptoms.
The study was presented in the journal of Alimentary Pharmacology & Therapeutics. I’m going to walk you through the study; what the study found; what the underlying mechanisms are, or how gluten exposure can cause depression; and what you need to do if you suspect your depression is due to gluten sensitivity.
The study looked at gluten causing depression in gluten-sensitive individuals that were non-celiac. There were a couple of markers they used: HLA-DQ2 and HLA-DQA8 testing as well as blood testing for celiac disease. If the subjects were negative for these, they were considered non-celiac and were put in the study group. None of the subjects in the control groups had celiac disease. This was to assure a celiac subject didn’t throw off the results. Celiac disease is an autoimmune condition that wears away at the microvilli in the small intestines, and people with celiac disease are traditionally sensitive to gluten.
The study consisted of three groups (listed below). For the first three days of the study, all the subjects were gluten free as well as low FODMAP (a group of carbohydrates that the small intestine has difficulty absorbing). People often wonder if it’s the gluten or the FODMAPs causing their problems, but in this study, they controlled this by keeping the FODMAPs low and the diets gluten free.
They established a baseline for group C three days before then changed them to the group-A diet for three more days. They gave the subjects various questionnaires that looked at personality, depression, anxiety, and a number of other symptoms, and what really stood out was the subjects’ anxiety and depression. This is a key finding because many people who are exposed to gluten notice they just don’t feel good for a couple of days. With something as simple as gluten, even if you don’t have celiac disease, even if you’re gluten sensitive but non-celiac, you could still be manifesting these symptoms because of that gluten exposure.
We have various microbes in our gut—these are our good bacteria. These good bacteria produce nutrition in the gut and send feedback signals back to the brain via our central and enteric nervous system.
These feedback signals from our nervous system via our gut bacteria can affect our immune system, the motility of our bowel movements, and the release of neurotransmitters. Neurotransmitter production in our gut can have a major impact on our mood. That is why many psychiatric disorders are associated with gastrointestinal disorders.
To schedule a complimentary consult to help remove your gut and mood problems, click here!
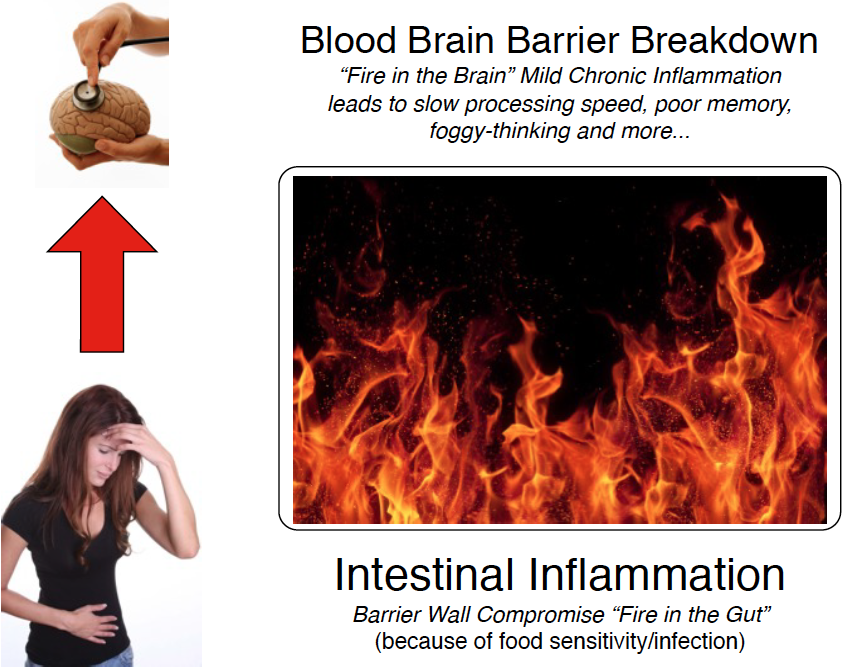
Basically, dysfunction in the gut-brain axis is attributed to excessive amounts of bad bacteria or dysbiosis, small intestinal bacterial overgrowth (SIBO), food allergens, inflammation and chronic infections.
Having healthy gut bacteria is important. Antibiotic exposure, extra medications, extra alcohol, and so on is going to wear away your healthy gut bacteria. So it’s vital you adapt an eating plan that relies on consuming low-toxin, anti-inflammatory, and nutrient-dense foods.
If you have SIBO, it would be very important to cut out FODMAPs, add probiotics, and address any chronic infection that maybe present. Addressing chronic infection is very important because an infection will constantly throw off your gut microbes and put stress on your immune system and your protective mucosal membrane barrier (secretory IgA).
Ignoring chronic infections is like trying to grow a garden without removing the weeds at their roots. You can go through the garden with a Weedwacker and only remove the weeds at the ground level, but roots run much deeper. Most people have had the experience of getting down on their hands and knees to pull weeds out at their roots. Well this is the same process that needs to be taken with specific antimicrobial herbal medicines to address the chronic weeds/infections in our gut!
“The synthesis of 5-HT in the brain is dependent on the availability of its amino acid precursor,
tryptophan. Interestingly, recent work has identified a link between protein ingestion, tryptophan production and concentrations of 5-HT in the brain.”
In this rat study referenced above, the rats that consumed zein (corn protein), casein (one of two dairy proteins), and gluten (protein found in most grains) showed a reduction in serotonin two and a half hours after ingestion. The data suggests serotonin levels in the brain are very sensitive to the nutritional quality of the proteins that are consumed. This adds another level to why gluten, over other proteins, may affect some individuals’ moods.
There are various microvilli in the small intestine that absorb nutrition. One of the things the study talks about is decreased 5-HT (5-hydroxytryptophan) absorption in the gut, and 5-HT is a precursor to serotonin. The 5-HT travels through the blood-brain barrier and converts to brain serotonin. It’s important to note here that while 5-HT converts to serotonin, serotonin cannot cross the blood-brain barrier. So 5-HT must pass through the barrier to be converted.
So you can see that if there is a 5-HT deficit coming out of the intestinal tract, there’s going to be a deficit of serotonin in the brain. If we don’t absorb that 5-HTP, it can’t cross the blood-brain barrier, and we won’t be able to convert it to serotonin.
Also to note, about 50% of the cells in the brain are microglial cells, which help provide immunity. When we constantly light up these cells with inflammatory molecules, they continue to be stimulated and stay turned on because they are constantly responding to inflammation. And because microglial cells make up such a great percentage of the brain, they don’t easily turn off—it takes a lot to get them dampened. The more our microglial cells stay on, the more brain fog we suffer from.
You have arteries (imagine tiny garden hoses) that travel up each side of your neck called the carotid arteries. These arteries can become sluggish from gluten choking the blood flow up to the brain (this is known as hypoperfusion). There are a handful of studies showing that hypoperfusion can affect blood flood to the cerebral cortex/front cortex and can even cause migraines.
The frontal cortex is where your personality, behavior, and all of the higher functions that make us humans come from. If we don’t have blood flow, we don’t have oxygen, and if we don’t have oxygen, we also don’t have adequate nutrition.
If you’re going to be exposed to gluten, even if it’s cross-contamination in a restaurant or somewhere else, or you’re out bingeing on your so-called cheat day, it can cause ramifications—like depression—and you should be aware of it.
Some people that are gluten sensitive have autoimmune conditions and need to be off gluten long-term. These people can’t even afford a cheat day. If you’re not feeling too good and you’re feeling a little down, consider the possibility that your depression could be due to gluten exposure.
To schedule a complimentary consult to help remove your gut and mood problems, click here!