
Dr. Justin Marchegiani and Evan Brand share with us today some pertinent clinical information regarding low DHEA levels and symptoms of adrenal fatigue. Find out 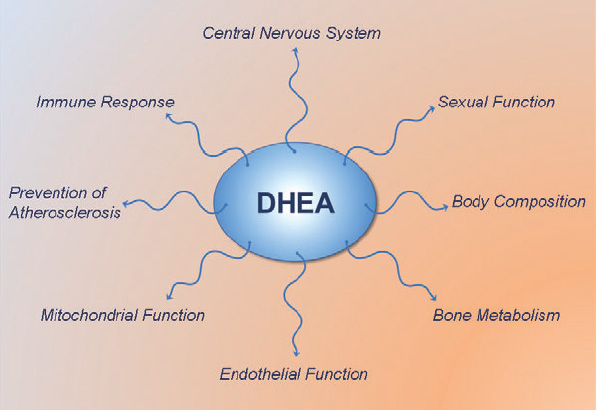 more about the relationship between DHEA and cortisol and get more insights on cortisol rhythms when you listen to today's podcast.
more about the relationship between DHEA and cortisol and get more insights on cortisol rhythms when you listen to today's podcast.
Learn about the symptoms that people get if they have adrenal dysfunction or if they have adrenal imbalance. Dr. Justin also discusses how DHEA affects women who are experiencing menopause. Discover what strategies you can do to help with stress hormones. Also find out about what salivary tests you can take to measure your DHEA-sulfate levels and learn how you can supplement DHEA.
In this episode, topics include:
00:58 About cortisol
2:33 What is DHEA?
5:03 Symptoms of adrenal imbalance
12:10 Strategies to help with stress hormones
15:00 Supplementing with DHEA
![]()
Dr. Justin Marchegiani: Evan, it’s Dr. J. It’s a beautiful Monday down here in Austin, Texas. What’s going on over in Louisville?
Evan Brand: It’s pretty. I had the window open but I had to shut it because there’s a bunch of big trucks that drive by and I wanted a super clean audio today.
Dr. Justin Marchegiani: Nice, awesome. Well, we got more pertinent clinical information coming out from our patients and from our practice, so more applicable information for everyone at home and we talked in our pre-show that we wanted to talk about DHEA, dehydroepiandrosterone. Do not confuse that with DHA, the 22-carbon fatty acid in fish oil, known as docosahexaenoic acid. We got all these multi-syllable words here that belong on Jeopardy. So we’re gonna be talking about the DHEA, the sex hormone precursor, not the fish oil DHA.
Evan Brand: Yes, sir.
Dr. Justin Marchegiani: Alright.
Evan Brand: So when we’re looking at adrenal cortisol or adrenal stress profile test, this is something that you and I run on every single patient, we’re gonna see that 24-hour rhythm where we want cortisol to be highest in the morning and we want it to gradually drop to the lowest point of the evening, where melatonin can come up and the person can actually go to sleep and feel good. But something that we see every single day is people are gonna have a few different things wrong with their adrenal rhythm. So one is gonna be that they have high cortisol that’s out of the charts which means that their body’s in a super catabolic state and they’re in one of the earlier stages of adrenal fatigue where they’re trying to start thriving and adapting to this stress. The body is producing excess hormones to deal with bear that they’re running away from even if that bear is taxes that they haven’t paid that they need to pay. And so secondly–
Dr. Justin Marchegiani: Yup.
Evan Brand: What we’ll see is that the cortisol is gonna be depressed all day and they’re gonna be in the later stage of adrenal fatigue where they’ve waited so long, they’ve burned the candle at both ends before they’ve come to work with one of us that now they have the depressed cortisol all day and that’s a whole another issue. And then the third piece of the puzzle, what we’re gonna discuss today, is the DHEA which I kind of using analogy of a bodyguard that’s gonna be anabolic in nature, that’s going to protect you from the potentially catabolic effects of cortisol and a lot of people will have either really high DHEA and their boat is still floating and they can cope–
Dr. Justin Marchegiani: Uh-hmm.
Evan Brand: With this cortisol or the DHEA is super tanked out and the cortisol’s tanked out as well and those are some of the worse cases that we’ll see.
Dr. Justin Marchegiani: Absolutely. Now DHEA, if we kinda break hormones into a couple of different categories to keep it simple, hormones typically help your body grow and heal and recover, fight inflammation and/or improve energy. We kinda put our all hormones in that category. Alright, if we look at like progesterone and estrogen, they’re helping with growth, right? So growth, tissue growth, ideally pregnancy at some point for women. We have sex hormones like testosterone and DHEA which can be very helpful for men and healing and recovery and again, we have hormones that are more stress-based hormones, catecholamines, norepinephrine, epinephrine, adrenalin, again those are all the same hormones, 3 different names, right? Medicine likes to be confusing like that and those are helping more with stress responses and to mobilize fuel during a stress response. So if we look at it in 3 categories, it’s inflammation, it’s cell growth and repair, and it is energy. So when we look at DHEA, that’s helping more of the anabolic, the growth side and as we become more and more stressed, our body prioritizes resources to deal with the stress of right now and hold off the healing of tomorrow. The problem is if you’re constantly stressed, well, tomorrow always keeps on getting put off by one day and we never quite reach that optimal repair window that we’re looking to be in for optimal health. So when we’re stressed, we’re breaking down faster, right? That’s catabolism or being in a cata—a catabolic state, right? It’s catastrophic to be in a catabolic state. That’s how I—I remember that. It’s not a good thing, so you’re breaking down too much and we wanna shift it over and DHEA is really an important anabolic hormone and it’s a pre-cursor, right? Because it can turn into 7 or 8 different things. They can turn into all 3 estrogens, estrone, estradiol, estriol. It can turn into your progesterone and it can even turn to—into andro or androstenedione and it can even turn into potentially DHT and testosterone. So a lot of different hormones it can go into and the goal is to help rebuild your body.
Evan Brand: Yeah and DHEA drops with age, too. So–
Dr. Justin Marchegiani: Big time.
Evan Brand: You and I aren’t too old yet where the point we’re still probably making a lot of DHEA but I’m seeing people with 22, 23 years old that have depressed DHEA levels worse than some of the 60-year-olds that we’ll look at. So just because you are young, it doesn’t mean that you are gonna have that maximum output if your adrenal stress is going to overwhelm that level. Maybe we should talk about some of the symptoms that people may be feeling if they do have some type of adrenal imbalance which would include DHEA.
Dr. Justin Marchegiani: Great. So a lot of the adrenal symptoms are gonna be connected in and around energy, in and around pain or inflammation whether it’s in the joints or it could be inflammation in the brain like brain fog, mood, memory, because DHEA is primarily gonna be produced by the adrenal glands, a female is gonna significantly notice it as they transition to menopause because now they’re—they’re not getting a lot of their anabolic hormones from their ovaries anymore because they’re no longer cycling. So as soon as they start going into this perimenopausal range where they start shifting or missing periods or they go 3 years without a period, that’s considered to be menopause. Once they start transitioning between 48 and age 51, they’re gonna be relying more on their adrenal glands for that sex hormone output. So my analogy is we get this backup generator, right? Let’s see you live in the northeast. I great up in the Boston area so this was common for me. But you’d have a—you purchase generator because if you ever had the power go out because of a big snowstorm for 2 or 3 days, you wanna make sure you don’t freeze. So you buy this big generator and typically the generators will run off of either electricity or gasoline. Now the gas has to be in the tank for that generator to work. So imagine if you got this big snowstorm, it hits and you don’t fill that generator up fully with gasoline, well, now when it comes time to need it and rely on that generator to power your house and to keep the heat going and electricity on, well, it’s not gonna be there for your needs, so you’re gonna start having symptoms have like maybe lower heat in the house. You may have less electricity. Maybe the TV will flicker. Now that’s kind of akin to your adrenal glands because that’s the backup generator for women as they go into menopause for their sex hormones, so just like we had a—a generator that was not fully charged when the snowstorm hit, the snowstorm now is gonna be menopause so when menopause starts happening that generator, your adrenal glands, are more depleted with DHEA so now when we start to rely on more on those adrenals, they aren’t gonna be there to help us in this stressful transitionary period. And then the symptoms of menopause come on harder which can be the mood, the hair loss, the—the skin issues. Obviously the hot flashes, fatigue, depression, a whole milieu of symptoms. It could be 20 or 30 going down a line, vaginal dryness, low libido, all of the—you know the top 10 or 20 things that we see, weight gain that all of our patients complain of.
Evan Brand: Yeah, I would say the sex drive one’s huge, too.
Dr. Justin Marchegiani: Yes.
Evan Brand: Every woman is—I—I’ve heard several women say they haven’t had sex in 10 or 15 years with their spouse. That is a long time and not to say that that’s what the whole relationship is built around, but a lot of people prioritize that as making love is a—is a good piece of their marriage and if that’s not in place due to hormones, it’s not you that will often get blamed or you’ll feel guilty or something or not. It’s time to take a deeper look at the hormones, it’s not just your brains.
Dr. Justin Marchegiani: Yeah, I totally agree. And then a lot of times that’s a symptom of something deeper hormonally, right? Because fertility is an important sign of health. So if for some reason those fertility signals aren’t there, i.e., libido being an important fertility signal, right? If we don’t have the libido, then you don’t have the—the strong motivation to—to have intercourse or to make love. So that’s a really important sign that something is not there on the hormonal side and again, when we have adrenal issues, we kinda have our 3 stages of adrenal fatigue or a better terminology is adrenal dysfunction, which just means as we go from stage normal to 1, that’s a sign that cortisol’s increasing and as we have that hyper-stress response, cortisol and DHEA will typically increase together. And as that response stays, right? If we have like someone sneak up behind us—boom—we go into that stage 1. It’s a quick—we call it the alarm phase by Hans Selye. It’s the alarm phase. So—boom—cortisol goes up, eventually we adapt and we go back into normal cortisol rhythm. But if we continue to stay stressed, our cortisol will start to drop with the rhythm. We’ll start to become more aberrant, meaning instead of having that nice high to low to lower to lowest rhythm, it starts going off. Maybe a little bit lower in the morning or higher in the afternoon or lower at night, right? And we start to feel that in our moods and our energy, and then we start to see DHEA drop in the stage 2 as well. DHEA will drop. And as we go into stage 3, we’ll start seeing cortisol and DHEA drop as well. And that’s like our ideal like scenario. We can go into some other scenarios that happen outside of our conventional 1, 2, and 3 for adrenal dysfunction. But as we go deeper from 2 into 3, what’s happening is HPA axis dysfunction. That thermostat in our brain is not able to talk to the AC and the heater, i.e., our adrenals and maybe thyroid and other gonadal glands. So we start having this type of dysfunctional pattern.
Evan Brand: So the way that I’ve understood, too, and correct me if I’m wrong is it’s not that the adrenal glands run out. They’re never gonna run out of hormones because they’re being told what to do by the brain and this whole HPA axis, so I’ve used this analogy for a while where the body is basically saying, “Hey, Justin, every time we give you stress hormones, you’re taking it and you’re running with it, and burning the candle at both ends or whatever, and so now I’m gonna downregulate and stop producing these hormones for you.” So basically what we’re doing is we’re trying to turn on this process again and basically tell the nervous system in the brain, “Hey, everything’s okay, let’s turn the system back on.” Is that the best way to bring that across or do you have any other ways you could explain or visualize that?
Dr. Justin Marchegiani: That’s exactly what we’re trying to do. We’re trying to get that HPA axis rhythm back on track. We’re trying to help support our body’s ability to regulate inflammation, generate energy, but also repair because the allocation is always hard wired to deal with the stress of now and the healing of tomorrow and we wanna make sure tomorrow actually happens. so our body can do what it has to do to repair.
Evan Brand: I mean, we definitely are in the—I think there’s a key chess piece going about it. It’s like a here today, gone tomorrow world, or something to that effect where people really are—they’re so stressed out and they’re so focused on today.
Dr. Justin Marchegiani: So Evan, we were just talking about strategies to help with stress hormones and to help push some of the anabolic hormones like DHEA back into balance. If you wanna go over a little more specifics on that?
Evan Brand: Yeah, so the treatment is something that we’ll get to but the testing is the first step so people listening they may resonate with some of the symptoms but you really have to do get that—you need that 24-hour cortisol rhythm to be able to identify it and that’s something you and I rely on very heavily because without it, we’re just guessing and checking and that’s where—this is nothing against naturopaths or anything, other type of medicine practitioner—but if you go to someone and you complain of the symptom and you just get thrown a supplement and even if it is a natural herbal supplement or minerals for example, if you don’t have a lab that you’re basing that protocol on, you’re sort of short-changing your potential results because you might start spending money on various supplements and bottles and I know everyone has a supplement graveyard where they’ve tried things and they don’t work, you and I want to minimize how many supplements end up in the graveyard or completely eliminate the graveyard because we’re gonna be basing things on your results rather than, “Well, I think you might benefit from this.”
Dr. Justin Marchegiani: Exactly. And again a lot of people is they get older that DHEA drops like we talk about and with some people, obviously, say with all people the diet and lifestyle strategies are gonna be really, really important, right? The blood sugar stability, obviously making sure diet’s like a Paleo template to start and then making sure we’re getting sleep and doing some movement. That’s kind of foundation. So everything we talk about after that is gonna be that already assumed. Just so we’re clear on that.
Evan Brand: Right.
Dr. Justin Marchegiani: But supplementing using DHEA, we like to do it sublingually because we bypass the liver and if we have patients, which we do quite frequently, that have digestive issues, we can bypass the gut, we can bypass the liver which can deactivate about 4 times—you have to get 4 times more orally via pill than you do with the sublingual drops. So we can bypass that, we can get the same effect of an injection without the needle by absorbing it to our sublingual and buccal tissue in the mouth.
Evan Brand: Uh-hmm. That’s great.
Dr. Justin Marchegiani: So again dosage-wise, we like to use smaller doses or lower doses, typically 5 to 10 mg is a pretty good starting dose and it’s kind of a little bit contradictory in thinking about we would actually use the more adrenally fatigued or the more adrenal dysfunction there is, we typically want to use less DHEA because of the fact that DHEA can also have an effect of lowering cortisol. So you can th—you can think of DHEA and cortisol as like a seesaw and the more DHEA we put in the system, the more it can decrease our cortisol level, so if we’re already having issues with energy and adrenal insufficiency and low cortisol and inability to regular inflammation, going too high on the DHEA can definitely cause some problems.
Evan Brand: Yes, sir.
Dr. Justin Marchegiani: So regarding that, typically we do DHEA between 5 and 10 mg sublingually, and then as a couple—so that’s spread out over 2 or 3 times—3 times over the course of the day because we’re trying to mimic normal physiology and not just give one whack at once, right? Your adrenals aren’t gonna just spit out a whole bunch of DHEA all at once. It’s gonna do it naturally so mimicking natural rhythms is gonna be the best possible way to handle it.
Evan Brand: Yeah, so if you’re at the health food store and you see 50 mg of DHEA, don’t buy and start taking that supplement just because you think you have low DHEA.
Dr. Justin Marchegiani: Definitely not worth it. And then also with DHEA, we—you alluded to like the DHEA cortisol ratio, typically we’re at this 6:1 type of ratio. We should be able to make at least 6 times the amount of cortisol in relation to one unit of DHEA. And as we start going above that, like you had a patient I think morning, Evan, that was at 30 you said, so there are—if we do the Math, they’re 5 times more catabolic than anabolic. In other words, in layman terms that means they’re breaking down 5 times faster than their body should be rebuilding and healing.
Evan Brand: Yeah, and this is actually a guy who’s doing CrossFit 3 to 4 times a week, and he’s wondering why he can’t build muscle.
Dr. Justin Marchegiani: Right, exactly. And again, there’s a lot of stuff out there on DHEA like not working, like not being good, or not being the best thing. There’s a lot of factors that go into it, right? Are we using DHEA in conjunction with the right amount of pregnenolone? Are we fixing underlying issues, right? If we just use DHEA like someone uses ibuprofen for a headache, right? Well, that may not be the underlying issue. If you’re banging your head every day and you’re taking ibuprofen for a headache, well, the underlying cause is banging your head. Now that’s kind of a drastic analogy but people have underlying analogies like infections or low stomach acid or dysbiosis or SIBO, or toxicity issues or food allergens and that—even though the banging the head is pretty obvious—it’s more subtle with the underneath things but that may still be in motion and happening every day, so we gotta make sure if we’re using DHEA and potentially pregnenolone with it, we gotta make sure it’s being used in conjunction with the comprehensive functional medicine program.
Evan Brand: Yeah, exactly, and based on labs.
Dr. Justin Marchegiani: Based on labs, yeah. And then typically for labs, we’re using that 2:10 I think—I think it’s the pg/mL ratio. It’s the typically salivary ratio that most labs use like BioHealth uses it, Diagnos-Techs uses it, CRT uses it, that’s your—your broad spectrum lab ratio and we like it—I’d say 6:10 is a pretty good place for me. What do you like?
Evan Brand: What are you—what are you saying?
Dr. Justin Marchegiani: For the lab rate—so like at the—the lab levels on the salivary lab, a DHEA-sulfate, what level do you like patients to be at regarding their DHEA?
Evan Brand: Most people they feel the best somewhere on the mid to upper end there, closer towards 6, 7, sometimes 8, definitely not what I saw this morning which was I think a 0.8 DHEA. That was just awfully low and he can feel it.
Dr. Justin Marchegiani: Wow, you saw someone at a 0.8! Yeah, that’s really low.
Evan Brand: Yeah, and this is the same guy. This is the guy whose cortisol sum was decent and he was like a 28, when we would consider something like 30 or more decent. So he was—he was decent on cortisol but the DHEA was less than 1 unit. So that’s the lowest I’ve seen, and most people say they feel best, it seems like 5, 6, 7, 8 somewhere in there. And then I’ve seen some other crazy ones—I’m sure you have, too—where DHEA was 20 or 30, just out of the roof and sometimes I found that these people were just popping DHEA supplements like Skittles.
Dr. Justin Marchegiani: Exactly and the—the range that I like for the lab of the DHEA-sulfate, that’s the salivary DHEA—DHEA-sulfate, it’s looking more at the storage form of DHEA, like 6:10 and that’s an ng/mL, nanograms per milliliter.
Evan Brand: Uh-hmm.
Dr. Justin Marchegiani: Okay, and then in the lab range like some of the blood labs, they’re a little bit different for the blood lab. We typically like in the—in the 200s for the blood lab. I’ll pull up my template that I typically use with most patients here in a sec. Any other comments on the salivary labs that—the salivary lab ranges?
Evan Brand: No.
Dr. Justin Marchegiani: Got it. Yeah, so looking at the blood labs are a little bit different. When we look at the blood, so the reference range maybe a tiny bit different here. Our blood labs, we’re typically gonna be looking at DHEA-sulfate. I like upwards of 250 to 300, and that’s micrograms per deciliters. So different reference range, different standard deviation, so upwards of 250 or so is a pretty good place to be and if you’re on DHEA drops, you gotta be mindful that you come off them for a day or at least 36 hours to 48 hours at least 2 days to get an accurate reading of what you’re DHEA levels are actually pumping out from the adrenals. Anything else you wanna add, Evan?
Evan Brand: No, that’s it.
Dr. Justin Marchegiani: Alright, great. Well, I know you got a patient here. I do as well. So wrapping it up, get your blood lab, a DHEA-sulfate done and/or get a comprehensive cortisol rhythm like Evan mentioned using the salivary DHEA. Well, great talk today, Evan. We will be in touch very soon.
Evan Brand: Take care.
Dr. Justin Marchegiani: Take care.
Evan Brand: Bye.
Dr. Justin Marchegiani: Bye.