
By Dr. Justin Marchegiani
Have you been diagnosed with and treated for small intestinal bacterial overgrowth (SIBO), and you still don’t feel any better? I see this over and over again—patients coming in after traditional treatments for SIBO, but they still feel terrible. Why is this, and what can you do to successfully tackle your SIBO? I’m going to break this down in three steps. I will address the fact that SIBO can be connected with other infections or dysfunctions, making it particularly difficult to treat.
Small intestinal bacterial overgrowth (SIBO) occurs when various bacteria living in our large intestine migrate back up into our small intestine. Our intestinal tract is about 21–22 feet long. Our stomach contents empty into our small intestine. It undergoes a series of biological processes before eventually emptying into our large intestine where a variety of bacteria, good and bad, live.
Once the bacteria from the large intestine invade the small intestine, these bacteria spit off various hydrogen or methane gases. When we do a lactulose breath test, this is what we are measuring, the hydrogen or the methane generated by the bacteria.
Hydrogen gas, for instance, is known to be associated with diarrhea, and methane gases are known to be associated with constipation. A lot of people who have SIBO may have a combination of hydrogen and methane, thus creating an alternation between constipation and diarrhea; this is very common.
The simple fact that these bacteria are now where they aren’t supposed to be, in the small intestine, disrupts digestion by affecting peristalsis (the contractions of the intestines that allow the contents to move through at a normal pace) and makes the gut very uncomfortable. When peristalsis is moving the contents too fast, we can have malabsorption where there’s not enough time to properly absorb the nutrients from our food. When peristalsis is moving the contents too slow, this can cause autointoxication where we absorb fecal toxins.
Once we have SIBO, there are some steps we can take to eliminate it.
Get expert advice on SIBO and a FREE Consult with a functional medicine doctor HERE.

Step one is to treat SIBO by starving the bacteria of the foods they thrive on:
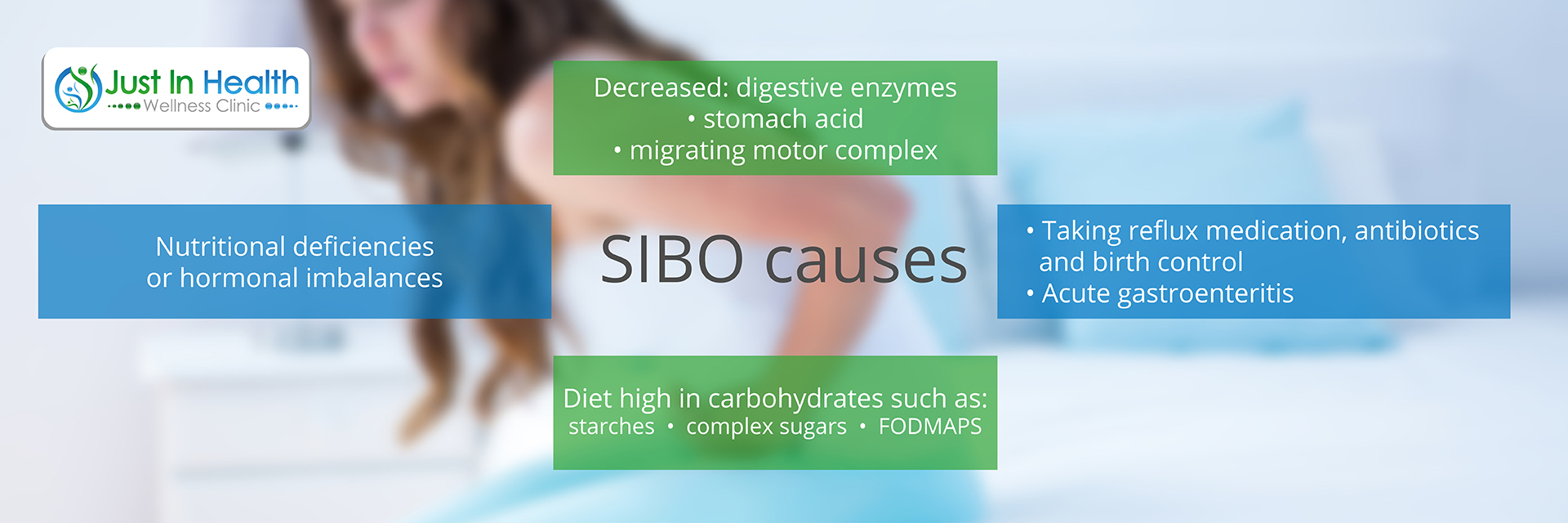
Starving the bacteria is like not filling your car up with fuel: eventually, it’s going to die. Starving the bacteria doesn’t mean you starve yourself. You just change the foods you are consuming. I recommend removing or lowering FODMAPs or changing to an autoimmune Paleo diet because there could be other food allergens, like eggs, beef, nuts, or seeds. That may not be high in FODMAPs but still may be disrupting and creating inflammation in the gut.
Step two is to attack SIBO with a functional approach toward killing it. There are a couple of different approaches.
If someone just has a SIBO infection, we can use that antimicrobial approach to knock it out of the park. But the challenge with either approach (the antibiotics and the antimicrobials) is that a lot of times people have a bigger underlying problem—an H. pylori infection, an amoeba, a protozoa, a worm, a parasitic infections, and so on—that really forms the hierarchy of the SIBO. The SIBO antibiotics and antimicrobials may not touch the underlying infections.
I saw a patient who tested positive, a year or two earlier, for an Entamoeba histolytica infection. That’s one of the mothers of all parasites, and it kills hundreds of thousands of people a year in third-world countries because it dehydrates them, causing diarrhea. She was treated four or five times with Rifaximin and Neomycin by leading conventional experts in SIBO in this country. At first, it reduced her symptoms, but those symptoms started coming back because while those antibiotics might tackle SIBO, they won’t touch an E. histolytica infection; they aren’t strong enough for that specific kind of amoeba.
So there may be a more supreme infection at the root cause of your SIBO, and that infection may be why the bacterial overgrowth is there in the first place. In order to kill SIBO, the root-cause infection must also be treated, and there are functional ways to treat these infections as well. So the goal is to determine if there is an bigger underlying infection, and if so, that needs to be knocked out before attacking SIBO with the functional approach.

Step three, we crowd out the bad bacteria with the good. Good bacteria includes Lactobacillus casei, Lactobacillus plantarum, various Bifidobacterium, and even soil-based probiotics.
So imagine the various good bacteria—we’ll call them GB—come in and gain a foothold. They take up a lot of the space that had been inhabited by the old infectious material. It’s like at the Grammys when a celebrity leaves his or her seat; a seat-holder (someone paid to sit in the seats so the theatre doesn’t look empty on TV) sits in the seat until the celebrity returns. But in our case, the GB, the good bacteria, have no intention of leaving their seat when the bad bacteria try to return. That’s what the probiotics have a really beneficial effect in doing—crowding out the bad bacteria.
Probiotics also affect the pH, and that can improve B vitamins and various nutrients, like vitamin K, as well. So there’s more than just the crowding-out aspect. There’s also a nutrient and an environmental aspect.

This is the foundational piece that a lot of doctors miss: supporting organ dysfunction. Let me explain. A patient comes in and has SIBO, iron-based anemia, adrenal fatigue, and Hashimoto’s (an autoimmune thyroid condition). If we just treated this person’s SIBO—let’s say we cut the FODMAPs and treated, attacked, and crowded out the SIBO—how would that patient do?
Depending on how good or bad the patient’s thyroid, adrenals, and anemia are, he or she would probably still feel terrible. So the rule of thumb is to support the dysfunctioning organ.
If we have an anemia, we have to get that fixed; if we have indigestion, we have to get the enzymes and the hydrochloric acid (HCl) functioning. We have to support the adrenals first and the thyroid second or at the same time, depending on how bad the thyroid is (the worse it is, the sooner we treat it). From there, we want to support the sex (male or female) hormones. So we really want to support the body’s ability to regulate energy.
Hormones are either a carpenter or a fireman. We have natural “fireman” hormones, like cortisol, that are like water putting out the fires of inflammation. And we have “carpenter” hormones, like DHEA, progesterone, estrogen, and testosterone, that are anabolic and help build us up. If the body is under chronic stress, chronically inflamed, it’s going to deplete its level of carpenters. The carpenter's ability to rebuild, its firefighters, or its ability to put out the fire are affected. So we always need to support the organ dysfunction.
It’s important to not just knock out the SIBO and its underlying infections but also to make sure all the organs are functioning optimally and the body is in balance because you’ll feel better faster.
Click here to contact a functional medicine doctor to HELP you with digestive issues and SIBO!
If you have SIBO or digestive symptoms and you want dig deeper into what the underlying cause may be, you may want to try the SIBO Solution—starve it, attack and kill it, crowd it out, and support the organ dysfunction. It’s important as well to choose the right natural supports to address the underlying infection.