
By Dr. Justin Marchegiani
Did you know that there are almost 30 million people (mostly women) that have an diagnosed thyroid disorder? Synthroid or levothyroxine (synthetic thyroid medication) is the 4th best selling drug on the market, yet with more thyroid medication being prescribed the problem doesn't seem to be getting better. Here's why!
Fatigue
Difficulty Losing Weight
Depression
Body Aches
Low Libido
Cold all the Time
Water Retention
Dry Skin
Eczema
Chronic Fatigue Syndrome
Fibromyalgia
PMS
Menopause
Diffuse Hair Loss or dry hair
Cold extremities
Constipation
Poor memory
Poor concentration
Anxiety
Weakness
Pale skin
Shortness of breath
Palpitations
PMS
Heavy menstrual flow
Muscle or joint aches
Poor motivation
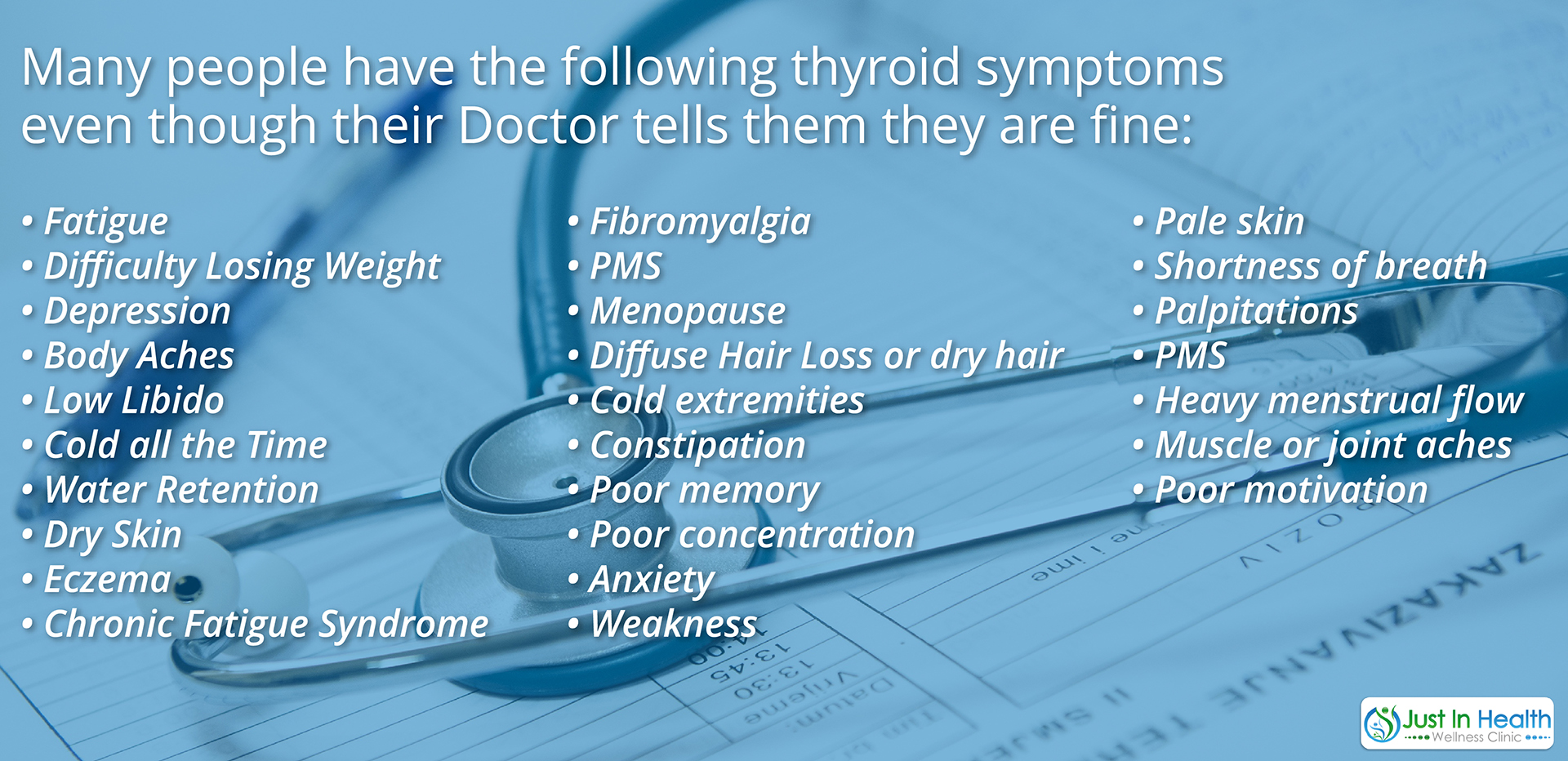
If you have 2 or more of the above symptoms and your Doctor is telling you you're fine, then this article is for you!
The typical thyroid test your Doctor is running is not a good indicator of your thyroid function. Most of the time the conventional thyroid tests are only looking at TSH (A Pituitary Hormone) and T4 (Inactive Thyroid Hormone). TSH, time and time again is shown to be a poor measure of overall thyroid function.
“TSH is a poor measure for estimating the clinical and metabolic severity of primary overt thyroid failure” (1).
Yet nearly every Doctor relies on this marker to treat their patients. So if you TSH comes back normal but intuitively you know something isn't right, what's your next step? Your next step is to get a comprehensive thyroid assessment so you can see exactly where your imbalances are occurring. Your thyroid can dysfunction in many different ways, below a picture depicting all of the different things that can effect thyroid function all the way from the brain to the gut.
If you are struggling with a thyroid imbalance and or need help looking over you lab tests feel free and reach out to by clicking here.
The problem with typical thyroid testing is the majority of treatment is dictated around TSH levels. Your TSH is a pituitary hormone, not a thyroid hormone. Research has shown that essentially the brain is more sensitive to thyroxine (T4) then the rest of the peripheral tissues so it's possible that TSH can drop to a normal level and at the same time the surrounding tissues have not received their proper fill of T4 yet.
“The serum concentration of thyroid stimulation hormone is unsatisfactory as the thyrotrophs in the anterior pituitary are more sensitive to changes in the concentration of thyroxine in the circulation than other tissues…It is clear that serum thyroid hormone and thyroid stimulating hormone concentrations cannot be used with any degree of confidence to classify patients as receiving satisfactory, insufficient, or excessive amounts of thyroxine replacement” (2).
The questions begs to be asked, “Are we treating a lab test or the patient?” The more we use a series of lab tests with other subjective and objective markers into the care plan, it's my belief the patient will start getting better faster.
Below are a series of lab tests that are essential to run to properly evaluate thyroid function.
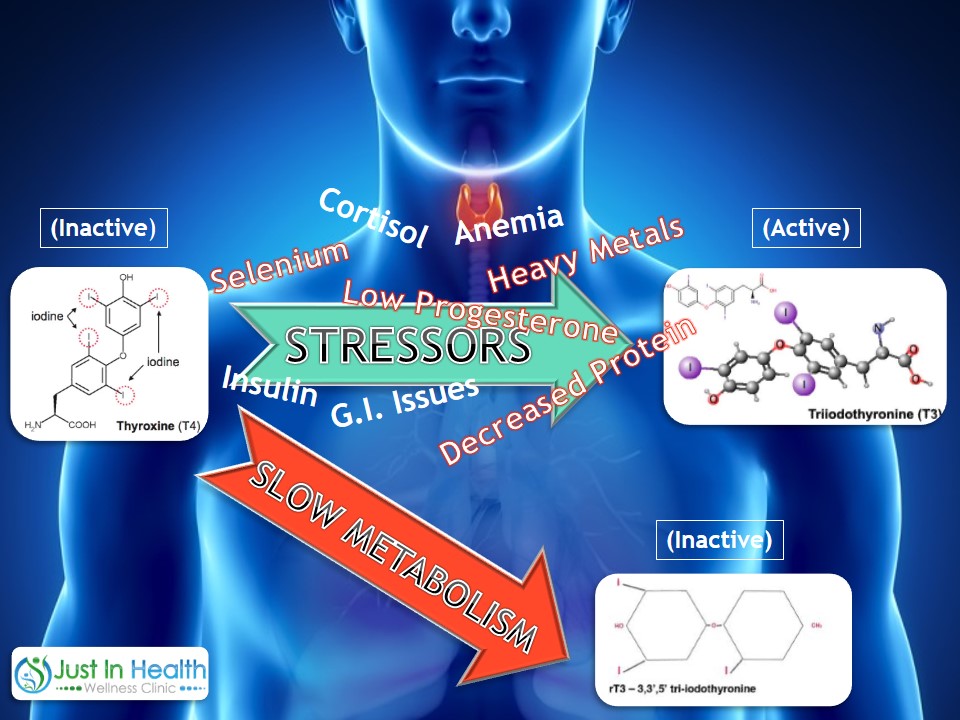
I also recommend running T4 total and free, T3 total and free, thyroglobulin, reverse T3, and T3 uptake. It’s important to assess the body’s ability to convert T4 (inactive thyroid hormone) to T3 (active thyroid hormone). Any time we see a normal level of T4 followed by a low level of T3 we know there is a conversion issue. On a conventional thyroid test, T3 would never be assessed and you would probably slip through the cracks of the medical system with an undiagnosed hypothyroid.
It is important to assess the levels of free fractions of thyroid hormones because those are the only hormones available to the receptor sites. Only 2% of hormones are free, meaning that they are bound to a protein carrier, therefore are free to bind to a receptor site and create a metabolic response. About 98% of thyroid hormone is protein bound so running both free and total thyroid hormone gives you a better perspective into the glands overall strength, the ability to convert T4 to T3 as well as the ability for thyroid hormone to bind to receptor sites.
Euthyroid patients receiving thyroxine (T4) replacement have higher serum thyroxine and free thyroxine concentrations than normal euthyroid subjects. This is not so for serum triiodothyronine and free triiodothyronine (T3) concentrations (2).
As you can see above, even patients that are given thyroid hormone replacement are not guarenteed to convert T4 thyroid hormone (Inactive) to T3 thyroid hormone (Active). Having adequate levels of T4 can make your TSH levels drop but it may not be enough to ensure your metabolically active thyroid hormone (T3) is adequate.
Did you know that 90% of all thyroid conditions stem from an underlying cause of auto-immunity (3)? Essentially the immune system is producing various antibodies that attack the thyroid tissue. Thyroid Peroxidase Ab (TPO), and Thyroglobulin Ab (TG) are produced in Hashimotos Thyroiditis which is an auto-immune condition that causes hypothyroid function over time.
Thyroid Stimulating Immunglobin Ab (TSI) or thyrotropin receptor antibodies are produced in Graves Disease, an auto-immune condition that causes hyperthyroid function.
At a minimum it's important to at least ask your doctor to run TPO and TG antibodies to see if your thyroid condition is auto-immune in nature. Most medical doctors resist running these antibodies because it doesn't change conventional protocol.
From a functional medicine paradigm it’s important to know if you are auto-immune because it changes the overall approach to how the thyroid is treated. Any time any auto-immune condition is present the focus needs to more on the immune system and the gut and less on the thyroid or injured gland.
TSH: Pituitary hormones that signals the thyroid to make T4, a poor marker of thyroid status unless elevated.
Total T4: 98% of T4 thyroid hormone that is inactive and protein bound.
Free T4: 2% of T4 thyroid hormone that is active and freely bound.
Total T3: 98% of T3 thyroid hormone that is inactive and protein bound.
Free T3: 2% of T3 thyroid hormone that is active and freely bound.
Reverse T3: Sign of a stressed physiology and a slower metabolism.
Thyroglobulin: Increases with BCP's (birth control pills) and higher levels of estrogen, decreases with elevation in testosterone like in PCOS.
T3 Uptake: How much active thyroid hormone is taken up by the receptor site. Elevated upate can be a sign of higher levels of testosterone commonly cause by PCOS (Poly Cystic Ovarian Syndrome) in females. Low uptake can be caused by elevations in estrogen primarily seen by BCP's.
TPO Antibody: 70% of auto-immune patients are positive for TPO.
TBG Antibody: Less likely positive but should still be tested to rule out auto-immunity.
TSI Antibody/Thyrotropin receptor antibodies: Auto-immune condition that causes hyperthyroidism or Graves Disease.
To get access to affordable thyroid blood testing click here!
There are some excellent calculated ratios that you can perform that can provide additional data points to assess your overall thyroid function.
Most Important Calculated Ratios (4)
TT3/RT3 Ratio: 10-14
RT3/Free T3: Ratio 20-30
Check out this awesome calculator then can help you figure out your thyroid ratio!
“The T3/rT3 ratio is the most useful marker for tissue hypothyroidism and as a marker of diminished cellular functioning.” (4)
If you would like to schedule a brief complimentary consultation to review your options and order the above lab tests; appointments can be made online by clicking here.
References:
1. British Medical Journal PMC143526.
2. British Medical Journal PMC1341585
3. Baillière's Clinical Endocrinology and Metabolism
4. The Journal of Clinical Endocrinology & Metabolism 2005; 90(12):6403–6409